Primary hepatic Burkitt’s lymphoma (PHBL) is a rare form of extranodal lymphoma that accounts for 40% of the cases of HIV-related lymphomas1. Prolonged immunosuppression, as occurs with HIV infection, is a risk factor for Burkitt’s lymphoma2. On the other hand, type A hemophilia is a congenital bleeding disorder characterized by coagulation factor VIII deficiency and is potentially fatal in patients with hematologic neoplasia (lymphoproliferative disorders) or solid tumors3. We present herein an interesting case of PHBL in an HIV-positive patient undergoing antiretroviral therapy (ART), in which the complexity of a coexisting hereditary bleeding disorder (type A hemophilia) was associated with great difficulty for its study due to the risk of fatal complications.
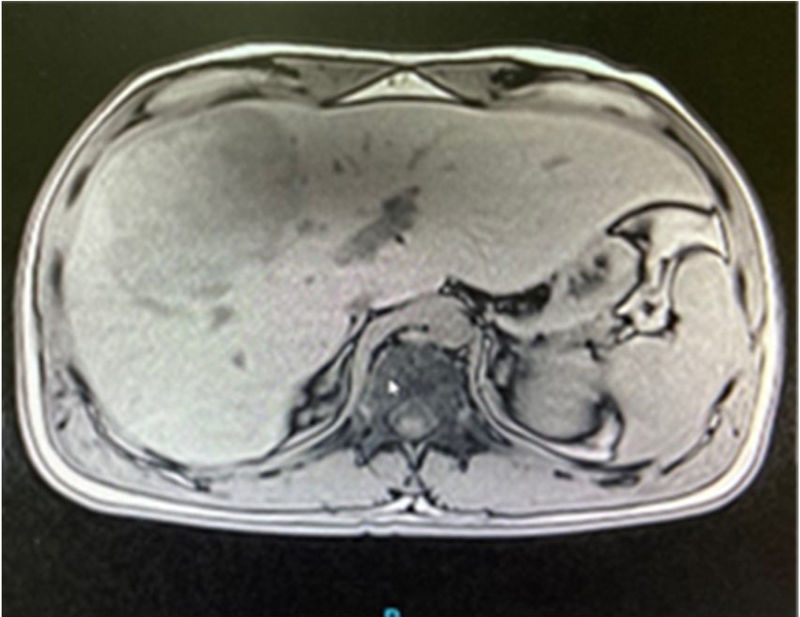
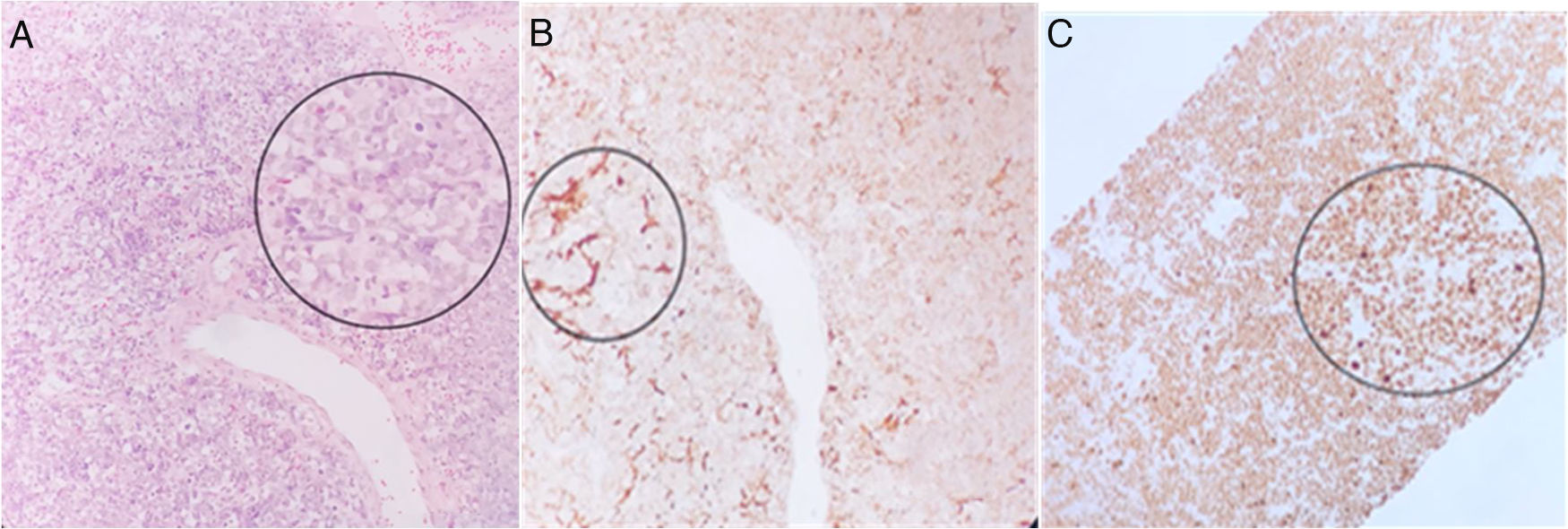
A 32-year-old man was born in Veracruz and resided there. He had a past medical history of type A hemophilia and HIV positivity (2018) managed with tenofovir, emtricitabine, and raltegravir, with a CD4(+) count of 44. He was referred to us from Veracruz because he presented with 2-month progression of oppressive, intermittent pain in the right hypochondrium of 5/10 intensity, hyporexia, and 4 kg weight loss, in addition to fever of up to 39 °C, predominantly in the evenings, chills, and night sweats. The striking biochemical profile results were leukocytes 6.04 thousand/mm3, ALT 56 U/L, GGT 252 U/L, AP 333 U/L, PT 14 s, INR 0.9, ESR 60 mm/h, CRP 112 mg/L, procalcitonin 0.16 ng/mL, and AFP 3.91 ng/mL. Fresh stool exam for amoebiasis and TORCH panel were negative. A heterogeneous parenchyma with an irregular lesion, measuring 21 × 14 × 14 cm at its longitudinal, transverse, and anteroposterior axes, was revealed in the triple-phase liver computed tomography (CT) scan; segments VI-VIII were involved, consistent with a neoproliferative liver lesion of the right liver lobe (LIRADS M), of likely malignancy, as well as a conglomerated intercaval and para-aortic lymph node mass (Fig. 1). Given those characteristics, a CT-guided liver biopsy was performed, which was a high-risk procedure due to the concomitant hemophilia. The patient was evaluated at the hematology speciality department to administer factor VIII, before and after the procedure, to reduce the risk for fatal complications. Immunohistochemistry of the sample was positive for CD45, CD20, BCL6, CD10, and Ki-67 in 90% of the neoplastic cells, confirming the diagnosis of Burkitt’s lymphoma (Figs. 2a, b, and c).
a) Liver biopsy. Slide stained with H&E at ×40, identifying a lesion with a solid pattern of small, round, blue cells, with monotonous nuclei substituting the liver parenchyma. b) Immunohistochemistry CD20 slide at ×40, identifying an immune reaction in the cells substituting the liver parenchyma. c) Immunohistochemistry Ki-67 slide at ×40, identifying an intense immune reaction in 100% of the cells, consistent with Burkitt’s lymphoma. The figure can only be seen in color in the online version of the article.
HIV-positive patients are at high risk for developing lymphoma, but since the advent of ART, there is greater control of its incidence, especially regarding PHBL4. Diagnosing PHBL is difficult, with increased risks in the presence of concomitant hemophilia, particularly with respect to biopsy, given that it is an invasive procedure, and so early diagnosis is hindered. The present case was also a therapeutic challenge due to the fact that thrombocytopenia is a complication associated with chemotherapy and can aggravate the bleeding tendency in patients with severe hemophilia, causing a potentially fatal bleeding event.
In conclusion, PHBL is an extremely rare form of extranodal lymphoma. HIV infection is associated with a higher risk for lymphoid tumors, the least common of which is PHBL. Even though ART has reduced the incidence of lymphoma, it continues to be among the main causes of death from AIDS.
Ethical considerationsThe present scientific letter meets the current regulations in bioethical research and was approved by the institutional ethics committee. It contains no personal information that could identify the patient.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Morgan DS, Guzmán AR, Barranco B, Salamanca M, Archundia AT. Linfoma de Burkitt primario en hígado en paciente con virus de la inmunodeficiencia humana asociada a tratamiento antirretroviral y hemofilia coexistente. Rev Gastroenterol Méx. 2023;88:71–72.