A 45-year-old man, with a past medical history of type 2 diabetes mellitus of 12-year progression, currently with good treatment adherence, and no other remarkable past medical history, was referred to the gastroenterology service because of chronic anemia under study. Hypochromic microcytic anemia due to probable iron deficiency was reported (CBC: Hgb 6.8 mg/dl, Ht: 28.7%, MCV: 57.9 fl, MCH: 13.7%). The patient was asymptomatic at diagnosis. Upper gastrointestinal (GI) endoscopy was ordered for the diagnostic approach to the anemia under study.
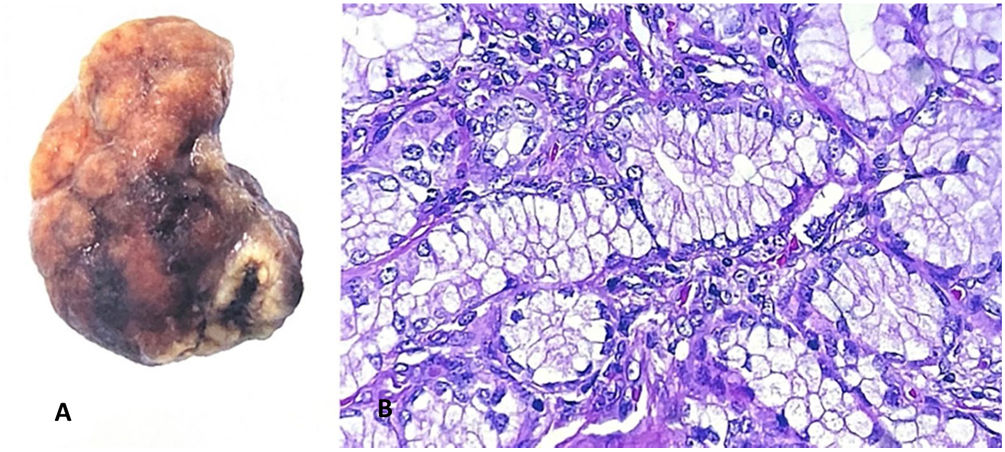
Upper GI endoscopy showed a pedunculated polyp in the duodenal bulb, measuring approximately 4 cm in diameter, in the first part of the duodenum, with signs of active bleeding. The decision was made to resect the polyp through the panendoscopy approach. Adrenaline was injected into the base of the polyp and 2 hemoclips were placed facing each other in the pedicle. Hot snare polypectomy was performed with no complications and the specimen was sent for histopathologic study (Fig. 1).
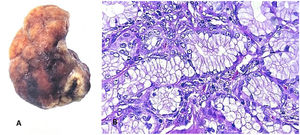
The histopathology report stated a dark brown nodular formation, measuring 4 × 2 × 2 cm, with a wrinkled surface. When cut, its consistency was soft and the interior consisted of light brown uniform tissue and a central area of bleeding, with a nodular proliferation of Brunner’s glands that included stroma and ducts. Immunohistochemical staining was positive for Ki67. Given those data, the conclusion was Brunner’s gland adenoma, with no signs of atypia (Fig. 2).
Branched acinotubular glands, called Brunner’s glands, are found in the mucosal and submucosal layers.1 The Swiss anatomist, Johan Conrad Brunner, first described them, identifying their main function as that of digestive juice secretion. The incidence of Brunner’s gland adenoma predominates in the fifth and sixth decades of life. It is considered an extremely rare tumor, with an incidence below 1% in endoscopic approaches.2 Brunner’s gland hyperplasia tends to be an incidental finding, but a symptomatic presentation can be related to malignant potential.3
Its clinical presentation is diverse, with physical examination, clinical imaging studies, or endoscopy resulting in the incidental finding in asymptomatic patients, as well as nonspecific abdominal complaints in symptomatic patients.4 The typical symptomatic presentation includes iron-deficiency anemia, gastrointestinal bleeding, ampullar obstruction, duodenal obstruction, or intestinal intussusception secondary to the presence of the tumor.5
The patient described herein had no apparent signs of upper or lower gastrointestinal bleeding, intestinal occlusion, or signs of intussusception, but did have the incidental finding of iron-deficiency anemia, and so was referred to the gastroenterology service because of the chronic anemia under study.
The pathophysiology of the origin of Brunner’s gland hyperplasia has not yet been determined. The main theory is that it is the result of excessive hypersecretion of hydrochloric acid, Helicobacter pylori coinfection, or inflammation due to the secretion of alkaline by Brunner’s glands.6 A stool antigen test for H. pylori was performed and its result was negative, ruling out an association with said infection.
Polypectomy through the panendoscopy approach is the procedure of choice for small lesions. Laparoscopy or laparotomy are reserved for tumors with sessile characteristics, when upper GI endoscopy cannot be performed or if there are complications, such as patients with hemodynamic instability due to gastrointestinal bleeding.2
In the present case, upper GI endoscopy plus hot snare polypectomy was performed, removing the specimen through the snare and endoloop, for its histologic study. The result was nodular proliferation of Brunner’s glands that included stroma and ducts. The analysis was completed using immunohistochemistry, with Ki67 positivity confirming the diagnosis.
Ethical considerationsNo informed consent was required, nor approval by an ethics committee, given that no personal data that could identify the patient were published.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Olivares LO, Gómez PC, Tamayo JS, Verdiales AK, Mendoza FY. Tumor de Brunner, abordaje endoscópico. Reporte de caso. Rev Gastroenterol Méx. 2023;88:72–74.