Autoimmune pancreatitis (AIP) is a systemic fibroinflammatory disease that affects the pancreas and other organs1. Prevalence in the pediatric population is low and the most frequent clinical presentation is abdominal pain, obstructive jaundice, and weight loss2.
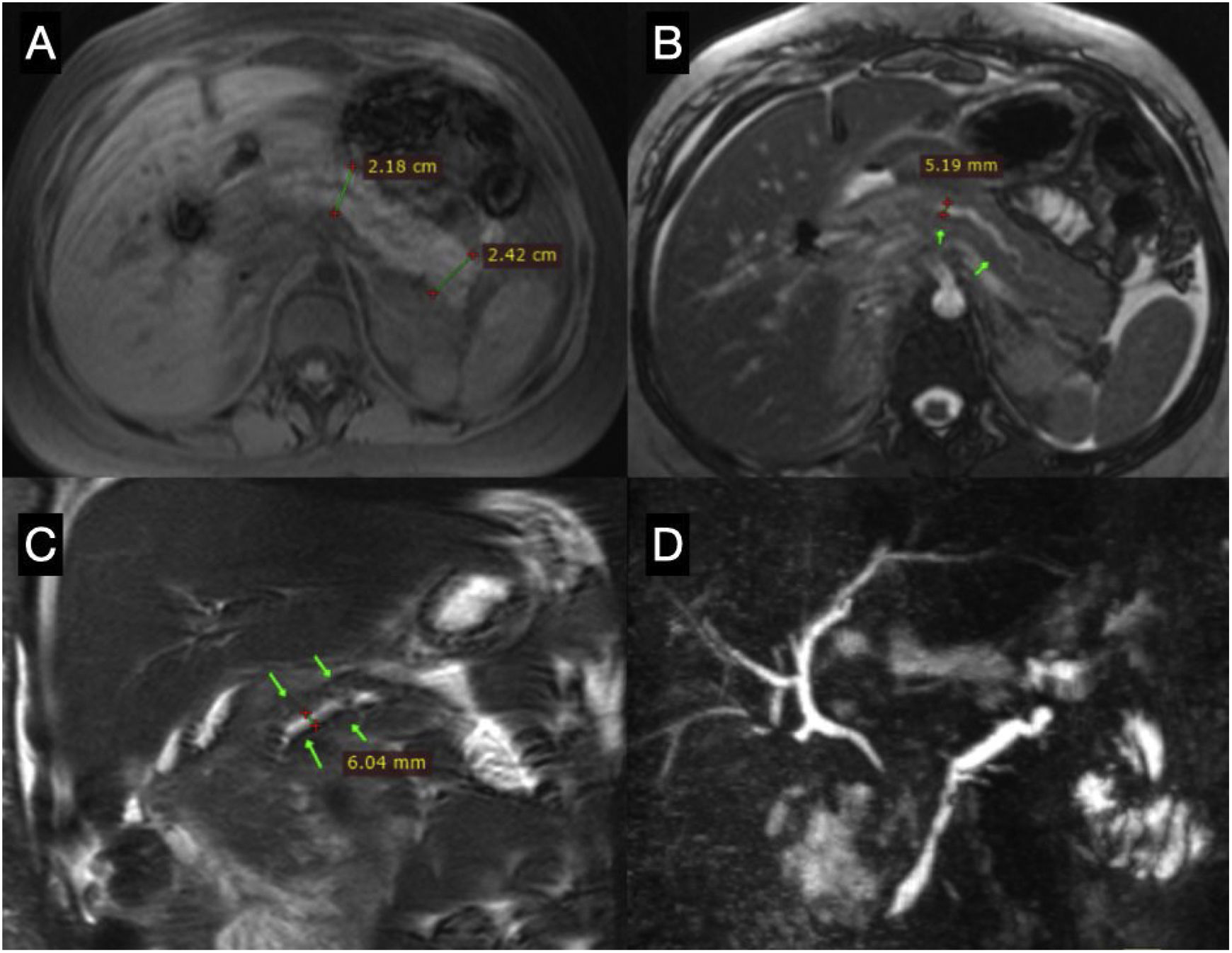
We present herein the case of a 15-year-old adolescent girl, with an unremarkable past medical history, who was seen by her family physician for chronic, intermittent, colicky abdominal pain of moderate intensity, located in the right upper quadrant, accompanied by nausea of one-month progression. Ultrasound imaging identified multiple stones, measuring 2–3mm, that occupied 70% of the gallbladder lumen, for which she was referred to the pediatric surgery department. She underwent laparoscopic cholecystectomy, revealing a fibroinflammatory process with an epiploic mass. The patient presented with postoperative intense abdominal epigastric pain, with vomiting and elevated pancreatic enzymes (amylase 1,006U/l and lipase 1,271U/l), and a computed tomography scan showed edema of the pancreas (Balthazar B). Magnetic resonance cholangiography revealed no evidence of stones and endoscopic retrograde cholangiopancreatography showed no evidence of stones in the pancreatic duct. The patient also presented with biloma that merited drainage performed by an interventional radiologist. The patient continued to receive parenteral nutrition and antibiotics, and lastly, was discharged with no apparent complications. One month later, she again arrived at the emergency department due to abdominal pain and vomiting. Laboratory test results revealed elevated pancreatic enzymes (amylase 1,248U/l and lipase 3671U/l), and an abdominal computed tomography scan showed pancreatic edema and a single peripancreatic collection (Balthazar D). Given the progression time, a new pancreatitis event was diagnosed. A recurrent pancreatitis approach was started, with a new magnetic resonance cholangiography study showing the single finding of segmental irregularity of the pancreatic duct (Fig. 1). Due to the suspicion of AIP, immunoglobulin subclasses were ordered, resulting in IgG4 levels of 221mg/dl (normal value: <140mg/dl) and negative antinuclear antibodies. The patient was started on immunosuppressive therapy with prednisone (prednisone 0.6mg/kg/day). At follow-up at more than 6 months, she presented with clinical improvement and has developed no other events of pancreatitis.
Magnetic resonance cholangiography. (A) T1-weighted axial view, showing the enlarged body and tail of the pancreas. (B) T2-weighted axial view, showing the body of the pancreas, with irregular dilation of the main pancreatic duct. (C) T2-weighted coronal view, showing the dilation of the main pancreatic duct. (D) MIP reconstruction of the cholangiopancreatography, showing irregular dilation of the main pancreatic duct and normal intrahepatic bile ducts.
Recurrent acute pancreatitis is characterized by the presentation of 2 episodes of acute pancreatitis, with complete pain resolution and pancreatic enzyme normalization between the two episodes. Recurrent acute pancreatitis occurs in 15–20% of patients after a first event of the disease, and even though AIP is rare in the pediatric population, it should be considered an etiologic possibility3.
Two forms of AIP are currently recognized. Type 1 AIP is a multisystemic disease that affects the pancreas (IgG4-related systemic disease) and type 2 AIP appears to be an autoimmune disease that specifically affects the pancreas4. In pediatrics, the study of AIP is limited to case series, and so its prevalence is unknown. Our patient presented with abdominal pain, which is found in up to 91% of children with AIP, but she did not have obstructive jaundice, which is reported in 42%2, signifying that clinical presentation can be heterogeneous. Gallstones are not seen in AIP, and a study that evaluated biliary tract involvement in adults with AIP reported the presence of bile duct stricture and the thickening of the bile duct wall and gallbladder wall as the most frequent findings5. Likewise, only 22% of children are likely to have elevated IgG4 levels2. That finding guided the diagnosis of our patient, in addition to the magnetic resonance images of the pancreas. She presented with the remission of pain after the administration of the steroid, thus meeting 3 of the criteria for the diagnosis of AIP, according to the International Consensus Diagnostic Criteria for Autoimmune Pancreatitis6, which includes one or more of the following 5 characteristics:
- 1.
Imaging studies: (a) pancreatic parenchyma (on computed tomography or magnetic resonance imaging) and (b) pancreatic duct (endoscopic retrograde cholangiopancreatography or magnetic resonance cholangiography).
- 2.
Serology (IgG4, IgG, and antinuclear antibodies).
- 3.
Involvement of other organs.
- 4.
Histopathology of the pancreas.
- 5.
Response to steroid therapy.
Due to previous abdominal interventions and the clinical, imaging, and biochemical characteristics consistent with AIP, we decided to forego pancreatic biopsy in our patient, in addition to the fact that endoscopic ultrasound imaging is not available at our center.
In conclusion, AIP should be studied in children with recurrent acute pancreatitis. The clinical manifestations can be heterogeneous. Even though the frequency of the disease in the pediatric population is low, multicenter studies are needed to characterize the clinical presentation, diagnosis, and progression of AIP in children.
Ethical considerationsThe authors obtained a written statement of informed consent from the patient described in this article and the document is in the possession of the corresponding author. The present work meets the current bioethical research norms, and because of the type of publication, does not require approval from the hospital’s ethics committee. The authors declare that this article contains no personal information that could identify the patient.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
The authors wish to thank Dr. Daniel Mendoza, a Radiology and Imaging Specialty resident physician at the Hospital General de Puebla “Dr. Eduardo Vázquez N”, for his contribution to processing the images presented in this case.
Please cite this article as: Peña-Vélez R, Jaramillo-Bermeo DA, Peña-Vergara MA, Bolaños A, Gil-Vargas M. Pancreatitis autoinmune en pediatría, una enfermedad poco frecuente. Rev Gastroenterol Méx. 2023;88:74–76.