The most common extranodal location of lymphoma is the gastrointestinal tract. The most frequent lymphomas are the large B-cell type, followed by MALT-type lymphoma.1 Primary intestinal follicular lymphoma is rare, occurring in 1–3% of all B-cell non-Hodgkin’s lymphomas.2
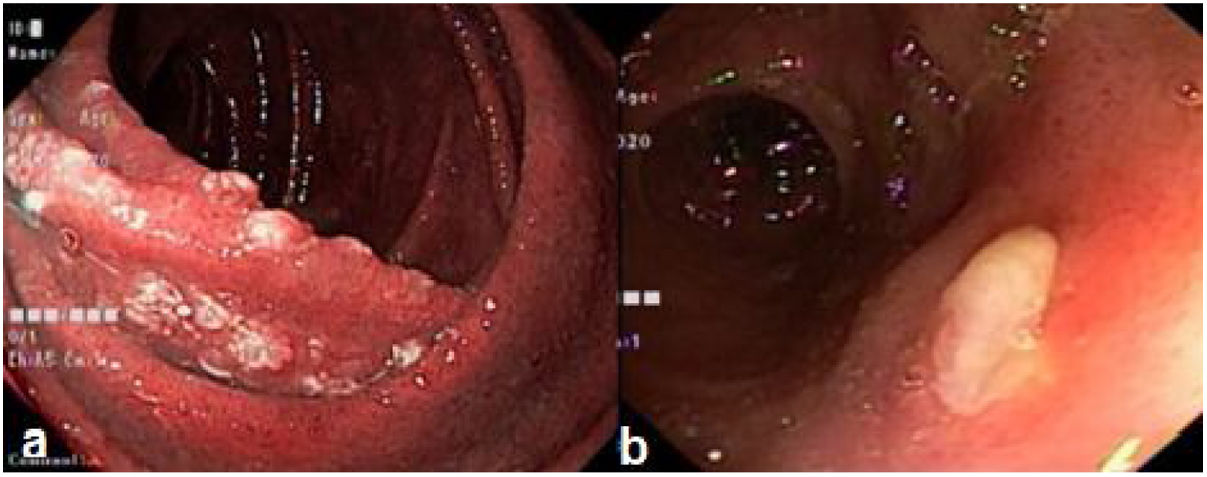
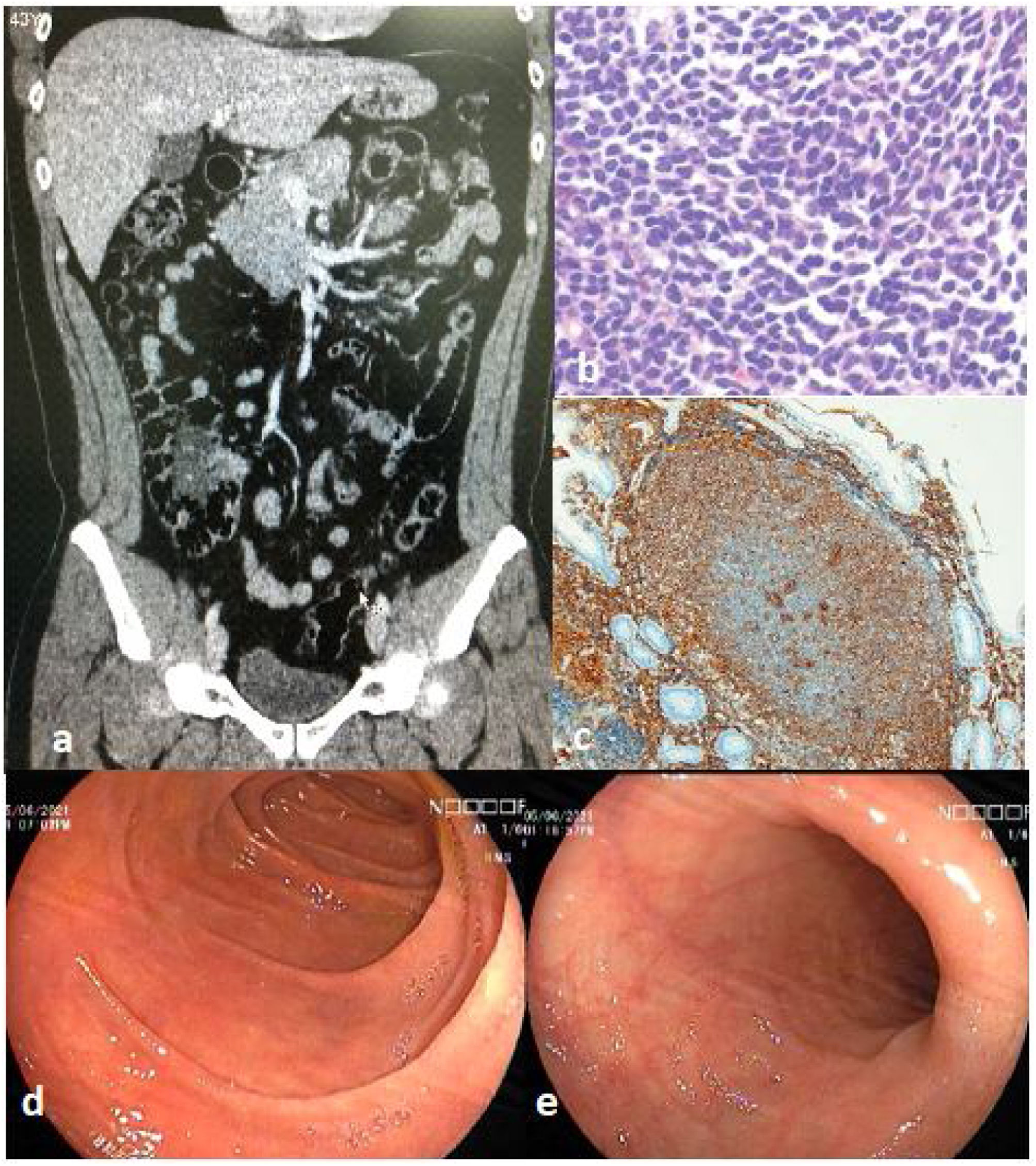
We present herein the case of a 44-year-old man who presented with 6-month progression of epigastric pain, associated with nausea and a 5 kg weight loss. Laboratory tests showed 8,170 cells/mm3 with 22% lymphocytes, Hb 14.7 g/dl, LDH 165 IU/l, and beta 2 microglobulin 1.2 mg/l. Endoscopy revealed a multifocal nodular pattern in the duodenum (Fig. 1a). Lower endoscopy showed a nodular pattern and an ulcer in the distal ileum (Fig. 1b), as well as an irregular mucosal area in the cecum. Tomography revealed mesenteric and retroperitoneal adenopathies and thickness of the cecal wall (Fig. 2a). The biopsy result was a structurally atypical lymphoid infiltrate with a nodular pattern (Fig. 2b). Immunohistochemistry was positive for CD20, CD10, BCL2 (Fig. 2c), and BCL6 (heterogeneous). Follicular dendritic cells were identified by CD23. Cyclin D1, CD3, and CD5 were negative, Ki-67 was 30%, and histiocytes were identified by CD68. With those findings, the diagnosis of primary intestinal follicular lymphoma was made. The final staging was II2 E (colon). The patient received 6 sessions of chemotherapy (R-CHOP), and at one year of follow-up, had favorable progression, with clinical, endoscopic, and imaging remission. We evaluated the duodenum and the distal ileum, and both appeared normal after one year of follow-up with chemotherapy (Figs. 2d and e).
Most patients with this type of lymphoma are adults, with an average 50 years of age. Both men and women are equally affected. They are frequently asymptomatic (43%), but some patients have abdominal pain (28%), nausea and vomiting (8%), and gastrointestinal bleeding (6%). The most frequent endoscopic presentation of follicular lymphoma is the nodular pattern.3–5 For the Lugano classification, imaging studies, such as computed tomography (CT) or positron emission tomography (PET), are necessary.6 The differential diagnosis includes lymphoid hyperplasia and duodenal xanthomas. The decrease in the vascular network and the presence of irregular vessels in the magnification are suggestive of lymphoma.7 The presence of an ulcer in the terminal ileum, as well as retroperitoneal adenopathies, can be suggestive of tuberculosis in endemic areas.8
If the patient manifests symptoms, treatment should be started, varying in accordance with the histologic and clinical grade. If the disease is disseminated or has poor prognostic factors, systemic treatment with chemotherapy combined with rituximab is indicated.9
We reported the present case, given that it is a rarity, together with the fact that there is no consensus on treatment.
In conclusion, primary intestinal follicular lymphoma is a unique lymphoproliferative entity. The disease course is indolent in the majority of cases and prognosis is excellent, as occurred in our patient.
Ethical responsibilitiesThe authors declare that no experiments on humans or animals were performed for this research. We used our work center protocols for obtaining patients from databases, preserving the anonymity of the patient described herein. We did not obtain the patient’s informed consent.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Alcántara-Figueroa CE, Valencia-Mariñas HD, León-Vega CI et al. Linfoma folicular primario intestinal: reporte de un caso. Rev Gastroenterol Méx. 2023;88:76–78.