Subtotal cholecystectomy has been employed in cases of tecnically difficult cholecystectomy to prevent common bile duct injury. Given that there are few reports in Mexico on the theme, we consider it important to present the 18-year experience of a surgical group in the South-Southeast of Mexico.
AimTo determine the safety of laparoscopic subtotal cholecystectomy in patients with acute cholecystitis.
Materials and methodsA retrospective, observational, and comparative study was conducted on patients with gallstones that underwent laparoscopic cholecystectomy. The variables analyzed were: anthropometric characteristics, comorbidities, conversion rate, surgery duration, hospital stay, and morbidity and mortality. Statistical analysis: Descriptive statistics were applied through measures of central tendency and dispersion and standard deviation, utilizing the SPSS v22 program.
ResultsA total of 1,101 medical records of patients with gallstones were reviewed. Of those patients, 223 presented with acute cholecystitis (20.25%) and they were divided into 2 groups: A) total cholecystectomy (82.95%) and B) subtotal cholecystectomy (17.05%). The anthropometric characteristics, risk factors, conversion rate, and hospital stay were similar in both groups. Only surgery duration was longer in the subtotal cholecystectomy group. Complications were more frequent, there was 1 death, and there was no bile duct injury in the subtotal cholecystectomy group. Those results were not statistically significant between the two groups.
ConclusionsSubtotal cholecystectomy is a valuable resource in patients with acute cholecystitis. In our case series, it was a safe and reliable procedure for preventing bile duct injury. A larger number of cases are needed to corroborate those results.
La colecistectomía subtotal ha sido empleada en casos de colecistectomía técnicamente difícil con objeto de evitar la lesión de la vía biliar principal. En México existen pocos reportes, por lo que consideramos importante presentar la experiencia de 18 años de un grupo quirúrgico en el sur-sureste de México.
ObjetivoDeterminar la seguridad de la colecistectomía subtotal laparoscópica en pacientes con colecistitis aguda.
Material y métodosEstudio retrospectivo observacional y comparativo en pacientes con litiasis vesicular sometidos a colecistectomía laparoscópica. Variables analizadas: Características antropométricas, comorbilidades, tasa de conversión, duración del acto quirúrgico, estancia hospitalaria, morbimortalidad. Análisis estadístico: Se aplicaron mediadas centrales y de dispersión y desviación estándar, por estadística descriptiva aplicando el programa SPSS v22.
ResultadosSe revisaron 1,101 expedientes de pacientes con litiasis vesicular, 223 presentaron colecistitis aguda (20.25%), los cuales fueron divididos en 2 grupos: A) Colecistectomía total (82.95%) y B) Colecistectomía subtotal (17.05%). Las características antropométricas, los factores de riesgo, el índice de conversión y estancia hospitalaria fueron similares en ambos grupos, solamente el tiempo quirúrgico fue superior en el grupo de colecistectomía subtotal. Las complicaciones se presentaron con mayor frecuencia en la subtotal presentando una defunción y no hubo lesión de la vía biliar, todos sin significación estadística entre ambos grupos.
ConclusionesLa colecistectomía subtotal es un valioso recurso en pacientes con colecistitis aguda; en nuestra serie fue un procedimiento seguro y confiable para evitar la lesión de la vía biliar. Se requieren mayor número de casos para corroborar dicha afirmación.
Laparoscopic cholecystectomy is the treatment of choice for gallstone disease. Its performance has increased significantly in recent decades because of its safety and the advantages it offers the patient. However, it is not exempt from complications, which vary from 0.5 to 1.2%, and accidental injury to the biliary tract is the most severe.1–5
Iatrogenic complications occur more frequently in patients that undergo surgery during an acute or complicated disease process, such as acute cholecystitis, hydrocholecyst or pyocholecyst, scleroatrophic gallbladder, or Mirizzi syndrome, or when there is an added regional pathology, such as cirrhosis. They condition great technical difficulty for adequately identifying the anatomic elements of Calot's triangle or inhibiting the hepatic surgical site bleeding the surgeon faces during the surgery. Thus, the term “technically difficult cholecystectomy” was adopted, in which there is a risk for accidentally causing injury to the biliary tract.6–9
To prevent said complication, in 1955, Madding performed the first subtotal cholecystectomy on a case that was technically very difficult, as a substitute for total cholescystectomy.10 In 1997, Bornman and Terblanche reported their experience in the management of acute cholecystitis associated with portal hypertension due to cirrhosis of the liver.11 Experiences with open or laparoscopic subtotal cholecystectomy were recently published in the international literature as safe procedures for resolving cases of complicated gallstone disease, or in patients with cirrhosis of the liver.12–22 There are few Mexican reports on the theme, therefore we decided to share the experience of our surgical group performing said technique in the South-Southeast of Mexico.23
The aim of our study was to determine the safety of laparoscopic subtotal cholecystectomy in patients with acute cholecystitis operated on over an 18-year period at a hospital in the Southeast of Mexico.
Materials and methodsA retrospective, observational, and comparative study was conducted on patients diagnosed with acute cholecystitis that underwent laparoscopic cholecystectomy over the 18-year period from 1999 to 2017.
The variables analyzed were age, sex, comorbidities, intraoperative findings, surgical incidents, conversion rate, surgery duration, hospital stay, and morbidity and mortality.
Description of the techniqueThe surgical technique consisted of freeing the adhesions from the omentum, colon and/or duodenum, puncturing the content inside the gallbladder and carefully dissecting Calot's triangle to precisely identify the cystic duct, closing it with a 00 silk purse-string ligature. An anterograde section was carried out in the gallbladder wall from Hartmann's sac, beginning at the neck and continuing to the fundus, leaving part of the gallbladder wall at the hepatic surgical site. The residual wall was cauterized, and the mucosa removed through electrocautery applied as a spray. An external drain was invariably placed. The decision to perform laparoscopic cholecystectomy was made during the surgical act, considering the difficulty in identifying the structures of the hepatic hilum, the cystic artery and cystic duct, as well as the degree of inflammation of and surrounding the gallbladder.
Statistical analysisIn the descriptive statistics, the results were evaluated through measures of central tendency and dispersion and standard deviation, utilizing the SPSS v22 program.
Ethical considerationsThe study was conducted in accordance with the principles of the Declaration of Helsinki and the protocol was approved by the Bioethics and Research Committee of the School of Medicine of the Universidad Veracruzana, Región Veracruz-Boca del Río. Informed consent was not requested for the publication of the present article because no personal data appeared in the manuscript that could identify the patients.
ResultsWithin the study period, 1,101 patients diagnosed with gallstone disease underwent laparoscopic cholecystectomy, and 223 of them (20.25%) presented with acute cholecystitis. Of those cases, 185 (82.95%) underwent total cholecystectomy (group A) and 38 (17.05%) underwent subtotal cholecystectomy (group B).
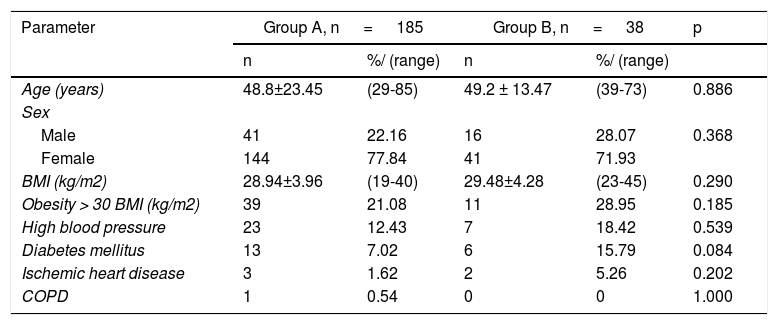
The anthropometric characteristics of the two groups were similar. The mean age was 48.8 ± 23.45 years in group A and 49.2 ± 13.47 years in group B, with ranges of 29-85 years and 39-73 years, respectively (p=0.886). Women were the predominant sex, with 77.84% and 71.05% in each group, respectively (p=0.368). The mean BMI was 28.94 ± 3.96kg/m2 in group A and 29.48 ± 4.28kg/m2 in group B, with ranges of 19-40kg/m2 and 23-45kg/m2, respectively (p=0.290). The most frequent risk factor was obesity, presenting in 21.08% of the group A patients and 28.95% of the group B patients (p=0.185). High blood pressure presented in 12.43% of the group A patients and in 18.42% of the group B patients (p=0.539); diabetes mellitus in 7.02% of the group A patients and 15.79% of the group B patients (p=0.084); three patients (1.62%) in group A and 2 patients (5.26%) in group B presented with ischemic heart disease (p=0.202); and one patient (0.54%) in group A had COPD (p=1.000) (Table 1).
Anthropometric characteristics and risk factors in the two groups.
| Parameter | Group A, n = 185 | Group B, n = 38 | p | ||
|---|---|---|---|---|---|
| n | %/ (range) | n | %/ (range) | ||
| Age (years) | 48.8±23.45 | (29-85) | 49.2 ± 13.47 | (39-73) | 0.886 |
| Sex | |||||
| Male | 41 | 22.16 | 16 | 28.07 | 0.368 |
| Female | 144 | 77.84 | 41 | 71.93 | |
| BMI (kg/m2) | 28.94±3.96 | (19-40) | 29.48±4.28 | (23-45) | 0.290 |
| Obesity > 30 BMI (kg/m2) | 39 | 21.08 | 11 | 28.95 | 0.185 |
| High blood pressure | 23 | 12.43 | 7 | 18.42 | 0.539 |
| Diabetes mellitus | 13 | 7.02 | 6 | 15.79 | 0.084 |
| Ischemic heart disease | 3 | 1.62 | 2 | 5.26 | 0.202 |
| COPD | 1 | 0.54 | 0 | 0 | 1.000 |
BMI: body mass index; COPD: Chronic obstructive pulmonary disease.
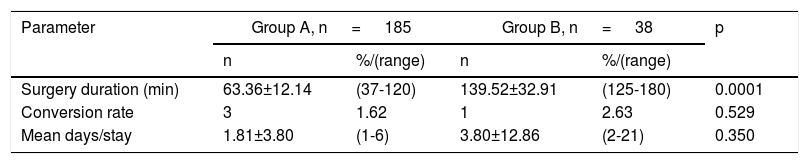
Mean surgery duration in the group A patients was 63.36 ± 12.14min, with a range of 37-120min, whereas it was 139.52 ± 32.91min in the group B patients, with a range of 125-180min (p=0.0001).
The conversion rate was 1.62% for group A and 2.63% for group B (p=0.529). Mean hospital stay for group A was 1.81 ± 3.80 days, with a range of 1-6 days, and 3.80±12.86 days for group B, with a range of 2-21 days (p=0.350) (Table 2).
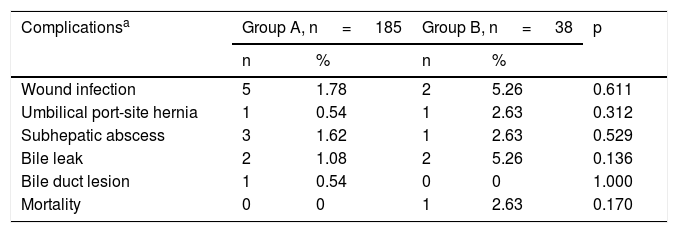
Progression was satisfactory in 173 patients in group A (93.51%), with complications in 12 cases (6.49%), and progression was satisfactory in 31 patients in group B (81.58%), with complications in 7 cases (18.42%) (p=0.874). The follow-up period was 6 months. There were 9 cases (11.13%) of minor complications: wound infection at the port site in 2.70% of the patients in group A and 5.26% of the cases in group B (p=0.611) and umbilical port hernia in 0.54% and 2.63% of the cases, respectively (p=0.312). There were 4 cases (21.05%) of bile leak through the cystic pedicle: 2 cases (1.08%) in group A and 2 cases in group B (5.26%). Common bile duct section occurred in one case (0.54%) in group A and in no cases in group B (p=0.136/1.000).
The overall mortality rate in the patient total was 0.49%, occurring in one group B patient in the early postoperative period due to pulmonary thromboembolism (2.63%), and there were no deaths in the group A patients (p=0.170) (Table 3).
Postoperative morbidity and mortality in the two groups.
| Complicationsa | Group A, n = 185 | Group B, n = 38 | p | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Wound infection | 5 | 1.78 | 2 | 5.26 | 0.611 |
| Umbilical port-site hernia | 1 | 0.54 | 1 | 2.63 | 0.312 |
| Subhepatic abscess | 3 | 1.62 | 1 | 2.63 | 0.529 |
| Bile leak | 2 | 1.08 | 2 | 5.26 | 0.136 |
| Bile duct lesion | 1 | 0.54 | 0 | 0 | 1.000 |
| Mortality | 0 | 0 | 1 | 2.63 | 0.170 |
Gallstone disease is considered a public health problem because it now affects 8-10% of the adult population worldwide. There is a 4:1 female:male ratio and the predominant age range is 30 to 60 years. Variations depend on geographic, alimentary, hereditary, and racial factors. It is believed that every year, 1.8% of the population will develop the disease and that 1-3% will be symptomatic cases requiring cholecystectomy.1,2 Frequency in Mexico is estimated at 6-10% of the adult population and is the second most widely performed surgery in secondary and tertiary care hospital centers.24
Acute cholecystitis is the most frequent complication of gallstones, especially in symptomatic patients (6-11%) and the risk factors are female sex, age ≤ 40 years, fertility, and obesity, in particular a BMI > 34, with an estimated mortality of 2 to 12%. In that group of patients, there is an increase in morbidity of 12-38%. In the last 5 years, procedure-related morbidity, notably accidental common bile duct injury, has been reduced to acceptable figures that vary between 0.5 and 1.2%.3–7
Technically difficult cholecystectomy is defined as the procedure that usually increases surgical risk, compared with simple or standard cholecystectomy, and tends to present with an incidence of 16%. It is regularly associated with severe inflammation that distorts the normal anatomy of Calot's triangle due to edema and inflammation of elements of the hepatic hilum, empyema, gangrene, perforation, and Mirizzi syndrome, or in cirrhotic patients in whom there is an increased risk for bleeding.8,9
In 1955, Madding was the first to perform subtotal cholecystectomy on case that was technically very difficult, as a substitute for total cholecystectomy to prevent bile duct injury,10 and in 1997, Bornman and Terblanche reported their experience in the management of acute cholecystitis associated with portal hypertension due to cirrhosis of the liver.11 In 1995, Nassar introduced a scale for evaluating the procedure's grade of difficulty, depending on the state of the cystic pedicle, and the importance of adhesions. It includes 4 grades, with grades 3 and 4 indicating procedures of greater difficulty.
In their editorial article, Strasberg et al. precisely defined the differences between partial cholecystectomy and subtotal cholecystectomy. They established subtotal dissection as the best laparoscopic procedure, suturing the cystic orifice and resecting the gallbladder from Hartmann's sac, with fenestration of the gallbladder remnant or suturing its edges, thus preventing injury to the common bile duct and reducing the possibility of bile leak.19
In 1999, our surgical team first performed laparoscopic subtotal cholecystectomy on a patient in whom the procedure was technically difficult. Since then, we have performed it on 37 more cases of acute cholecystitis, representing 3.36% of the 1,101 patients that underwent cholecystectomy due to gallstone disease in Veracruz, within the 18-year study period. In general, anthropometric characteristics are similar to those of uncomplicated patients, as demonstrated in our case series. Mean age in the two groups was 49.2 ± 13.47 years, with a range of 39-73 years; women were predominant at 71.93%, compared with the 28.07% of cases that were men; and BMI was 29.48 ± 4.28kg/m2 with a range of 23-45kg/m2. Our results were similar to those in the studies by Shaffer and Davis.1,20
In our study, the risk factor of obesity was higher in the subtotal cholecystectomy group (21.08% [grupo A] vs. 28.95% [grupo B]), whereas high blood pressure, diabetes mellitus, and ischemic heart disease were higher in the subtotal cholecystectomy group at 18.42, 15.79, and 5.26%, respectively. COPD presented in 0.54% of the total cholecystectomy cases. However, none of the values of the parameters were statistically significant (Table 1).
Technically difficult cholecystectomy results in longer surgery duration, as well as conversion to open surgery, as shown by Elshaer et al. and Strasberg et al.9,19 In our case series, the performance of subtotal cholecystectomy took twice the amount of time as that of total cholecystectomy, and the difference was statistically significant. The conversion rate and mean days of hospital stay were similar in the two groups and not statistically significant, even though hospital stay in one patient that underwent subtotal cholecystectomy was 21 days due to an external biliary fistula that was treated conservatively.
Postoperative progression was satisfactory in the majority of the cases. Complications presented in 19 patients (8.52%). They were considered minor in 11.13% of the cases (port-site infection or hernia) and were slightly higher with subtotal cholecystectomy than with total cholecystectomy (5.6% and 2.63%, respectively). Major complications, such as subhepatic abscess and bile leak through the cystic pedicle were similar in the two groups and favorably resolved, maintaining drainage through canalization placed at the gallbladder bed until completely healed. The mean follow-up period was 6 months. There were no cases of bile duct injury with subtotal cholecystectomy and only one case with total cholecystectomy, which was resolved in the same surgery through biliointestinal diversion, with satisfactory patient progression. No patient required reintervention. There was only one death and it was in the subtotal cholecystectomy group, corresponding to a 73-year-old woman, who was obese and had high blood pressure. She presented with pulmonary thromboembolism on postoperative day three. The complications were acceptable, and the mortality rate was within universally accepted parameters, with no statistical significance between the two study groups.
ConclusionSubtotal cholecystectomy can be resorted to in cases of acute cholecystitis to prevent accidental biliary tract injury.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo financial support was received in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Roesch-Dietlen F, Pérez-Morales AG, Martínez-Fernández S, Díaz-Roesch F, Gómez-Delgado JA, Remes-Troche JM. Seguridad de la colecistectomía subtotal laparoscópica en colecistitis aguda. Experiencia en el sureste de México. Revista de Gastroenterología de México. 2019;84:461–466.