The different forms of lubrication are among the most simple, accessible, and economic techniques that have been implemented for improving the diagnostic performance of colonoscopy.
AimTo determine whether the use of oil improved the number of complete colonoscopies, facilitated the procedure, reduced pain, or improved the study's diagnostic performance, compared with the conventional lubrication technique.
Patients and methodsOne hundred and seventy-five patients referred for colonoscopy were alternately allocated to receive treatment with the standard lubrication method with chlorhexidine gel (group 1) or lubrication with corn oil administered through the working channel (group II). The number of complete colonoscopies, the length of time needed to reach the cecum, the degree of difficulty estimated by the endoscopist and the assistant, the level of pain at the end of the study estimated by the patient, and the endoscopic findings were all determined.
ResultsEighty-eight patients made up group I and 87 made up group II. No statistically significant differences were found between the two groups in relation to general characteristics, the number of complete colonoscopies (93 vs. 97%, respectively), the time needed to reach the cecum (8:00 vs. 8:41min, respectively), the level of pain at the end of the study, or the detection of polyps. The degree of difficulty was slightly lower in group II, but with no statistical significance.
ConclusionsLubrication with oil during colonoscopy did not improve the number of complete colonoscopies, did not facilitate the study, nor did it reduce pain or increase the diagnostic performance of the study, when compared with the conventional technique.
Entre las técnicas más simples, accesibles y económicas que se han implementado para mejorar el rendimiento diagnóstico de la colonoscopia destacan las diferentes formas de lubricación.
ObjetivoDeterminar si el uso de aceite mejora la proporción de colonoscopia completa, facilita el procedimiento, reduce el dolor y mejora su rendimiento diagnóstico en comparación con la técnica de lubricación convencional.
Pacientes y métodosCiento setenta y cinco pacientes enviados a colonoscopia fueron sorteados para utilizar el método de lubricación estándar con gel de clorhexidina (grupo i) o lubricación con aceite de maíz administrado por el canal de trabajo (grupo ii. Se determinó la proporción de colonoscopias completas, el tiempo requerido para llegar al ciego, el grado de dificultad estimado por el endoscopista y por la asistente, el dolor después del estudio estimado por el enfermo y los hallazgos endoscópicos.
ResultadosSe incluyó a 88 en el grupo i y 87 en el grupo ii. No se observaron diferencias entre los grupos en las características generales, la proporción de colonoscopias completas (93 vs. 97%, respectivamente, p = NS), el tiempo necesario para alcanzar el ciego (8:00 vs. 8:41min, respectivamente, p = NS), el dolor al término del estudio ni en la detección de pólipos. El grado de dificultad fue discretamente menor en el grupo ii pero sin significación estadística.
ConclusionesLa lubricación con aceite durante la colonoscopia no mejora la proporción de colonoscopia completa, no parece facilitar el estudio, no reduce el dolor y no aumenta rendimiento diagnóstico del examen en comparación con la técnica convencional.
Colonoscopy is the diagnostic method of choice for studying symptoms and diseases of the colon, especially for the detection of polyps and colorectal cancer.1 This diagnostic method has reduced mortality from colorectal cancer through the detection and treatment of premalignant polyps and malignant lesions in their early stages.2 To that end, it is indispensible that colonoscopy is performed meeting the basic quality parameters, such as being carried out after adequate bowel cleansing, achieving cecal intubation in the greatest number of cases possible, performing the study within the correct withdrawal time, achieving an adequate adenoma detection rate, and performing the procedure following screening recommendations and at the accepted monitoring intervals.3,4
Different techniques and devices have been implemented for improving the diagnostic performance of colonoscopy. These include better imaging systems and electronic chromoscopy,5 instruments that facilitate cecal intubation,6 enable visualization of the blind spots,7,8 and that optimize revision, reducing folds and flexures.9,10 Nevertheless, there are simpler, more accessible, and more economic ways to facilitate colonoscope insertion, reduce pain during the procedure, and increase polyp detection: i.e. lubrication techniques with water and oil.11 Unfortunately, this subject has rarely been considered for study in endoscopy, and therefore there is not enough existing evidence, especially in relation to the lubrication technique with oil, to establish its usefulness.
The aim of our study was to determine whether the use of lubrication with oil during deep sedation and conscious sedation colonoscopy improved the number of complete studies, facilitated the procedure, reduced pain, and improved diagnostic performance, when compared with the conventional technique.
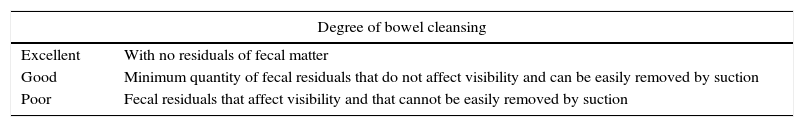
Patients and methodsAll the patients seen at the private practice of one of the researchers (RCS) within the time frame of January 2013 and February 2014 were invited to participate in the study. All the patients with appropriate indication for colonoscopy according to the American Society for Gastrointestinal Endoscopy12 that accepted to participate in the study and that signed statements of informed consent were included. Those patients with absolute contraindication for colonoscopy, inflammatory bowel disease, colon resection, active gastrointestinal bleeding, debilitating or decompensated chronic diseases, or hemodynamic instability were excluded. All patients with inadequate bowel cleansing were eliminated from the study. In relation to the latter, both the endoscopist and the assistant independently evaluated the degree of cleansing utilizing the scale developed by Brocchi et al. (Table 1). If both of them decided that the preparation was poor up to the sigmoid colon, the patient was eliminated from the study. Those patients with good or excellent bowel preparation up to the sigmoid colon then proceeded to group assignation by alternate allocation.
Degree of bowel cleansing.
| Degree of bowel cleansing | |
|---|---|
| Excellent | With no residuals of fecal matter |
| Good | Minimum quantity of fecal residuals that do not affect visibility and can be easily removed by suction |
| Poor | Fecal residuals that affect visibility and that cannot be easily removed by suction |
Modified from Brocchi et al.13
All the eligible patients received bowel preparation the day before their study with 4 l of polyethylene glycol in divided doses and they were alternately allocated to one of the 2 groups. The standard lubrication method with chlorhexidine gel in the anal region and on the tube of the endoscope in the quantity considered necessary for facilitating insertion and movement of the equipment was used in group I. In group II, the gel was used in the same manner, and in addition, 30ml of corn oil were instilled through the working channel in the sigmoid colon at the splenic angle and the hepatic flexure. The oil was aspirated during the withdrawal of the equipment. The procedures were performed by the same endoscopist (RCS) and assisted by the same nurse (CRV) who obviously had to know the lubrication method being used in each case, but the patients were not aware of the method being used. The majority of the procedures were carried out under deep sedation with propofol administered by an anesthesiologist, but some stable patients with no concomitant diseases had conscious sedation with intravenous midazolam and fentanyl administered by the endoscopist. All the procedures were performed with oxygen supplementation through nasal points, vital sign monitoring, and continuous oxygen saturation, as well as the administration of butylhyoscine (a single 10mg intravenous dose).
The number of patients in whom intubation of the cecum and terminal ileum was achieved, the time it took to reach the cecum, the complementary procedures performed (e.g. polypectomy or biopsy), and the endoscopic findings were registered during the study. All studies in which cecal intubation was not achieved were considered “incomplete”. Using the study by Brocchi et al.13 as a reference, the grade of difficulty was independently estimated by the endoscopist and the assistant, using the visual analog scale (VAS) of 0-100mm in which 0 was defined as “very easy” and 100 as “very difficult”. Pain estimated by the patient was also registered at the end of the study using the same VAS of 0-100mm in which 0 was defined as “no pain” and 100 as “unbearable pain”.
An independent observer carried out the time measurements, registering the hour at which the study began up to reaching the cecum and insertion, when possible, into the ileum. The time lapse from the withdrawal from the ileum or cecum up to the extraction of the endoscope was also registered. Likewise, the length of time the endoscope remained stationary for performing complementary procedures such as biopsy or polypectomy was also registered. For the purposes of our study, the time lapse encompassing the withdrawal from the ileum or cecum and the extraction of the endoscope was referred to as the “actual withdrawal time”, and the amount of time employed in the complementary procedures was subtracted from it. Only those patients with complete colonoscopy were considered for the calculations of the withdrawal time and the actual withdrawal time.
Statistical analysisAll the clinical data were recorded on a collection sheet and placed in a database (Excel 2015 for Office 365, Microsoft Corporation, Redmond, WA, USA). The descriptive data were expressed through percentages, means, and ranges. The chi-square test and the Fisher's exact test were used for the comparative analysis and calculated with the Epi Info application for the iPad (Epi InfoTM, version 2.0.2. Centers for Disease Control and Prevention, Atlanta, GA, USA). All p values greater than 0.05 were considered statistically non-significant.
ResultsA total of 212 patients with an appropriate indication for colonoscopy were attended to and invited to participate during the study period. Thirty-five patients were excluded for different reasons: 13 for debilitating or decompensated chronic diseases (diabetes mellitus, ischemic heart disease, or renal insufficiency), 7 due to prior colorectal surgery, 3 due to ulcerative colitis, 3 due to active colonic bleeding, and 9 patients that did not consent to participate. Two patients were eliminated from the study for poor bowel cleansing.
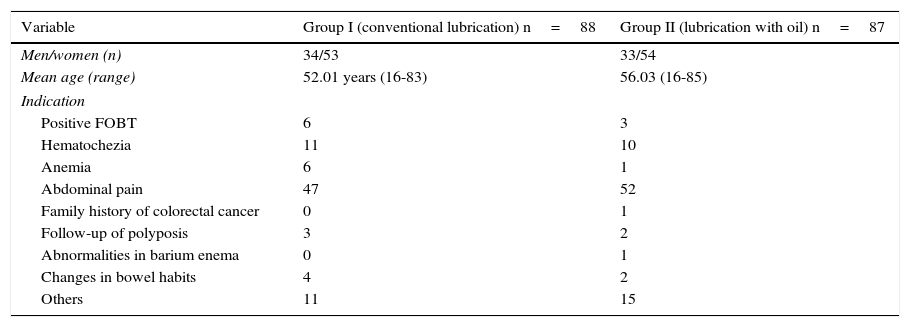
One hundred seventy-five patients were included in the study: 88 in group I (conventional lubrication) and 87 in group II (lubrication with oil). The patients in both groups were similar in age, sex distribution, and colonoscopy indication (Table 2). Even though the mean age in group II was slightly higher, it did not reach statistical significance. The number of patients above the age of 60 years was similar in the two groups: 24 in group I and 32 in group II were above 60 years of age (28 vs. 36%, respectively, p=NS).
General group characteristics.
| Variable | Group I (conventional lubrication) n=88 | Group II (lubrication with oil) n=87 |
|---|---|---|
| Men/women (n) | 34/53 | 33/54 |
| Mean age (range) | 52.01 years (16-83) | 56.03 (16-85) |
| Indication | ||
| Positive FOBT | 6 | 3 |
| Hematochezia | 11 | 10 |
| Anemia | 6 | 1 |
| Abdominal pain | 47 | 52 |
| Family history of colorectal cancer | 0 | 1 |
| Follow-up of polyposis | 3 | 2 |
| Abnormalities in barium enema | 0 | 1 |
| Changes in bowel habits | 4 | 2 |
| Others | 11 | 15 |
The cecum was reached in a similar number of patients in the two groups. Complete colonoscopy was achieved in 82 subjects in group I and 85 subjects in group II (93 vs. 98%, respectively, p=NS). Colonoscopy was considered incomplete in 6 subjects in group I and in 2 subjects in group II (7 vs. 2%, respectively, p=NS). The mean time needed to reach the cecum was also similar in the two groups: 8min in group I (range: 2-34min) and 8min 41 s in group II (range: 3-27min) (p=NS). The number of subjects in whom terminal ileum intubation was achieved was also similar: 70 patients in group I and 68 patients in group II (79 vs. 78%, respectively, p=NS). The mean withdrawal time was significantly greater in the patients in the conventional lubrication group (21min, range: 10-59min) compared with the oil lubrication group (13min, range: 5-33min), but the mean actual withdrawal time was the same between the two groups: 9min (range: 3-18min) in group I and 9min (range: 5-20min) in group II (p=NS).
The grade of difficulty evaluated by the physician and expressed through the VAS (in mean mm) was slightly lower in the group lubricated with oil, but there was no statistical difference (group I: 19mm [range: 3-67mm] vs. group II: 16mm [range: 3-69mm], p=NS). The grade of difficulty evaluated by the assistant and expressed through the VAS (in mean mm) was similar in the two groups (group I: 13mm [range: 0-63mm] vs. group II: 14mm [range: 0-84], p=NS). Polyps were detected in 17 of the group I patients and in 15 of the group II patients (19 vs. 17%, respectively, p=NS). Loop polypectomy was performed in 7 of the group I patients and in 5 of the group II patients (8 vs. 6%, respectively, p=NS). No cases of colorectal cancer were detected.
Patient abdominal pain estimated by nurse acting as the assistant was similar in the two groups (mean VAS group I: 6mm [range: 0-61mm] vs. mean VAS group II: 5mm [range: 0-82mm], p=NS). The patients of the group that received oil lubrication complained of greater abdominal pain before release, but the difference was not statistically significant (mean VAS group I: 10mm [range: 0-70mm] vs. mean VAS group II: 14mm [range: 0-100mm], p=NS).
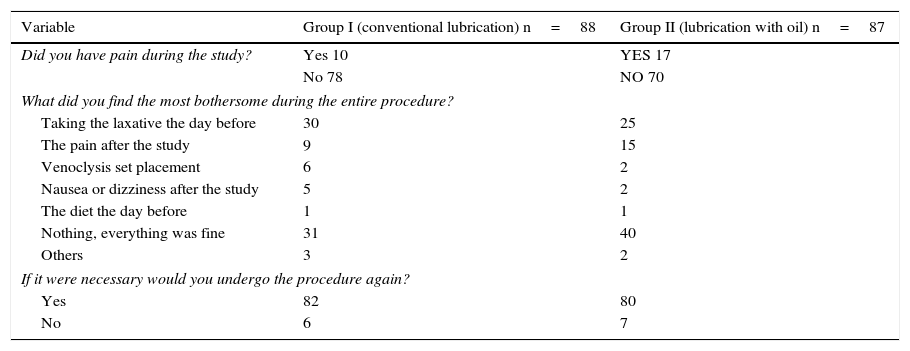
Table 3 shows the most frequent discomfort reported by the patients in relation to the procedure and their acceptance or not of a possible future colonoscopy.
Survey results applied upon patient release.
| Variable | Group I (conventional lubrication) n=88 | Group II (lubrication with oil) n=87 |
|---|---|---|
| Did you have pain during the study? | Yes 10 | YES 17 |
| No 78 | NO 70 | |
| What did you find the most bothersome during the entire procedure? | ||
| Taking the laxative the day before | 30 | 25 |
| The pain after the study | 9 | 15 |
| Venoclysis set placement | 6 | 2 |
| Nausea or dizziness after the study | 5 | 2 |
| The diet the day before | 1 | 1 |
| Nothing, everything was fine | 31 | 40 |
| Others | 3 | 2 |
| If it were necessary would you undergo the procedure again? | ||
| Yes | 82 | 80 |
| No | 6 | 7 |
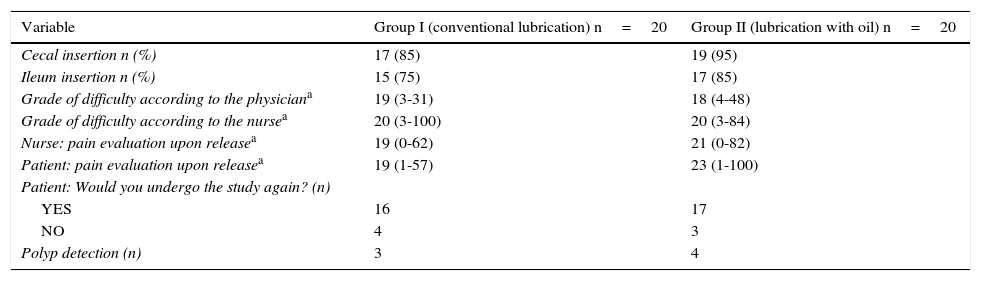
The results in those patients whose colonoscopy was performed exclusively with conscious sedation and analgesia are shown in Table 4. No statistically significant differences were observed in the different parameters evaluated using this particular form of sedation.
Results in patients that underwent colonoscopy with analgesia and conscious sedation.
| Variable | Group I (conventional lubrication) n=20 | Group II (lubrication with oil) n=20 |
|---|---|---|
| Cecal insertion n (%) | 17 (85) | 19 (95) |
| Ileum insertion n (%) | 15 (75) | 17 (85) |
| Grade of difficulty according to the physiciana | 19 (3-31) | 18 (4-48) |
| Grade of difficulty according to the nursea | 20 (3-100) | 20 (3-84) |
| Nurse: pain evaluation upon releasea | 19 (0-62) | 21 (0-82) |
| Patient: pain evaluation upon releasea | 19 (1-57) | 23 (1-100) |
| Patient: Would you undergo the study again? (n) | ||
| YES | 16 | 17 |
| NO | 4 | 3 |
| Polyp detection (n) | 3 | 4 |
Our study demonstrated that lubrication with oil during colonoscopy did not improve the number of complete colonoscopies, did not facilitate the study, did not reduce pain after the procedure, and did not increase the diagnostic performance of the study when compared with the conventional technique. Results were the same for patients that underwent deep sedation assisted by an anesthesiologist and those that had conscious sedation.
Colonoscopy is an invaluable method in clinical practice, but its greatest impact has been demonstrated in the decrease in mortality from colorectal cancer, due to the detection and treatment of adenomatous polyps and early stage cancer.2 In the last few years, special relevance has been given to quality indicators for reaching optimum colonoscopy effectiveness14 and new techniques and tools have been developed for the purpose of improving its diagnostic performance. These include better imaging systems and electronic chromoscopy,5 as well as instruments that facilitate insertion into the cecum,6 enable visualization of the blind spots,7,8 and optimize revision, reducing folds and flexures.9,10 But there are more accessible, simpler, and more economic ways to facilitate colonoscope insertion, reduce pain during the procedure, and increase polyp detection: i.e. the lubrication techniques with water and oil.11
There are 2 varying techniques of water-aided colonoscopy: water immersion and water exchange.15 The water immersion technique is characterized by a sufficient amount of water infused during the insertion of the equipment so that the direction in which the colonoscope is to be moved can be seen and the water is suctioned out during equipment withdrawal.16 The water exchange technique is a modality in which water is infused and suctioned during the introduction of the equipment and the bags of air or gas that are met during insertion are systematically removed.17 Both technical variants have been shown to attenuate patient discomfort and reduce pain during colonoscopy, especially when the procedure is performed without sedation,18 with minimum sedation, or with on-demand sedation.17 A review of the literature and a meta-analysis that included 9 studies and more than 1,200 patients showed that warm water infusion during colonoscopy resulted in less pain than the standard air insufflation technique, reducing the need for sedation/analgesia and improving patient acceptation of colonoscopy without increasing adverse reactions.19 Another systematic review that included only controlled and randomized studies showed that the water immersion and water exchange techniques significantly reduced pain, compared with air insufflation.20 However, the benefit of the water immersion technique is not limited to pain reduction. It has recently been applied as therapy in sigmoid colon volvulus, lesion resection, the management of lower intestinal bleeding, and the detection of abnormal colon morphology in patients with irritable bowel syndrome.21 Controlled, comparative, and randomized studies suggest that the water exchange technique may be superior to the water immersion technique for optimizing the detection of adenomas, particularly in the proximal colon.20,22,23 Due to all its qualities, water immersion has recently been used successfully in complex therapeutic procedures such as peroral esophageal myotomy (POEM)24 to such a degree that expert opinion states that water instillation during colonoscopy is a technique that all endoscopists should use, at least in certain procedures.25
Another variant of this technique, such as the administration of oil, has been used in a fewer number of studies and with controversial results. Brocchi et al.26 instilled corn oil through the working channel and found that its use was associated with a greater frequency of cecal insertion and less pain, compared with the conventional technique. The same authors compared oil instillation, the use of warm water, and the conventional technique in 510 patients that underwent colonoscopy, demonstrating that the use of corn oil and warm water was associated with a greater frequency of cecal insertion in a shorter period of time and less pain, compared with the conventional technique, but with no difference between the first 2 techniques.13 In contrast, Park et al.27 compared oil instillation, the use of warm water, and the conventional technique with the administration of antispasmodics in 117 patients that underwent colonoscopy without sedation performed by endoscopists in training. They found that the use of water facilitated the procedure, whereas the use of oil was associated with greater pain. There was no difference in the frequency with which cecal insertion was achieved in the 3 groups. Due to its simplicity, low cost, and potential increase in the diagnostic performance of colonoscopy, we decided to conduct the present study evaluating the potential usefulness of oil lubrication. However, our work showed no substantial differences between the use of oil and the conventional technique in relation to facilitating the study, pain, or diagnostic performance of colonoscopy in patients under deep sedation or in those that only received conscious sedation.
The main strength of our study lies in the random assignation of the lubrication technique carried out on groups of subjects with similar clinical characteristics and the fact that the same endoscopist-assistant pair performed the colonoscopies. Colonoscopy facilitation and its associated pain were evaluated, taking into account the estimation of the patient, the nurse, and the physician. Both techniques were compared in a blind manner in patients that underwent colonoscopy under deep sedation and under conscious sedation. Nevertheless, our study did not include a group for comparing the water immersion or water exchange techniques because it is our opinion that they been sufficiently evaluated, showing their superiority to the conventional method. Another weakness of our study is the low number of patients that underwent colonoscopy under conscious sedation. Finally, even though polyp detection was similar to that with the conventional technique, the suctioning of oil can cause visual field alterations, which we feel reduces its practicality. We believe that despite the fact that this technique did not provide advantages for the majority of patients, further studies on specific populations are necessary, such as on those patients that underwent failed conventional colonoscopy or those with known anatomic alterations (e.g. dolichocolon, redundant sigmoid colon, or non-critical stricture).
We conclude that lubrication with oil during colonoscopy does not improve the number of complete colonoscopies, facilitate the study, reduce pain, or increase the diagnostic performance of the examination, when compared with the conventional technique.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that the procedures followed conformed to the ethical standards of the responsible committee on human experimentation and were in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestJosé Luis Rodríguez-García declares that he has no conflict of interest.
Ramón Carmona-Sánchez is a Member of the Advisory Counsel of Mayoly-Spindler and is a Speaker for Mayoly-Spindler and Asofarma. He participated in a clinical research study for Laboratorios Senosiain, Mexico.
Carmen Rosas Vitorino declares that she has no conflict of interest.
Please cite this article as: Rodríguez-García JL, Carmona-Sánchez R, Rosas-Vitorino C. Usefulness of oil lubrication during colonoscopy: A comparative study with the conventional technique. Revista de Gastroenterología de México. 2016;81:28–34.