¿ Introduction
Bile duct injury following cholecystectomy can result in morbidity and decreased survival.1,2 Bile duct strictures following cholecystectomy injury have been successfully treated endoscopically with dilation and stenting. However, treatment of complete bile duct occlusion resulting from ligation has not been previously described. We describe the use of an endoscopic intervention that resulted in successful recanalization of the common hepatic duct (CHD) following accidental ligation during cholecystectomy.
¿ Case presentation
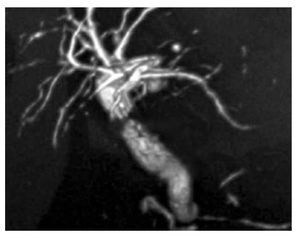
A 75 year old woman underwent cholecystectomy (laparoscopic converted to open) for symptomatic cholelithiasis. Following discharge, the patient was readmitted 25 days later with abdominal pain and jaundice. Laboratory evaluation revealed direct hyperbilirubinemia of 17 mg/dL (normal 0 - 0.2 mg/dL) and alkaline phosphatase elevation of 977 IU/L (normal 90 - 234 IU/L). Magnetic resonance cholangiopancreatography (MRCP) showed intrahepatic biliary dilation and complete stenosis of the CHD, 2 cm distal to the confluence (Bismuth I lesion), Figure 1.
¿ Figure 1. Magnetic resonance cholangiopancreatography (MRCP) reveals intrahepatic biliary dilation and complete interruption of the common hepatic duct located 2 centimeters distal to the bifurcation (Bismuth I).
¿ Technique
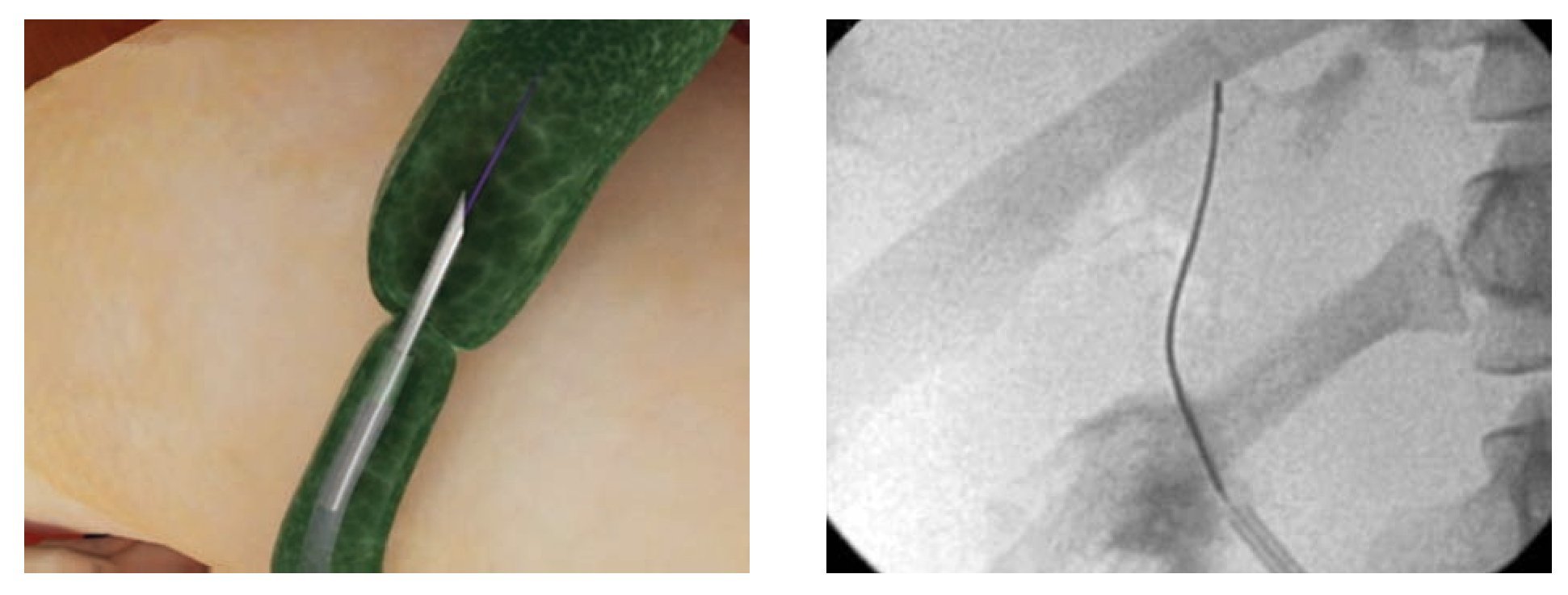
Device: The Artifon Catheter (Scitech, Sao Paulo, Brazil), boasts a retractable 18-gauge needle and a flexible metallic sheath at the distal end (Figure 2a, 2b). It was designed for biliary cannulation by puncturing the bile duct transduodenally and passing a 0.025" or 0.035" guidewire using the Seldinger technique.3 A second lumen allows for simultaneous injection of contrast.
¿ Figure 2a. The Artifon needle catheter is designed for puncture access to the biliary system. It has a double lumen - one for insertion of a 0.025" or 0.035" guidewire and one for contrast injection. 2b.The catheter displays a retractable needle and a flexible metallic sheath at its distal end.
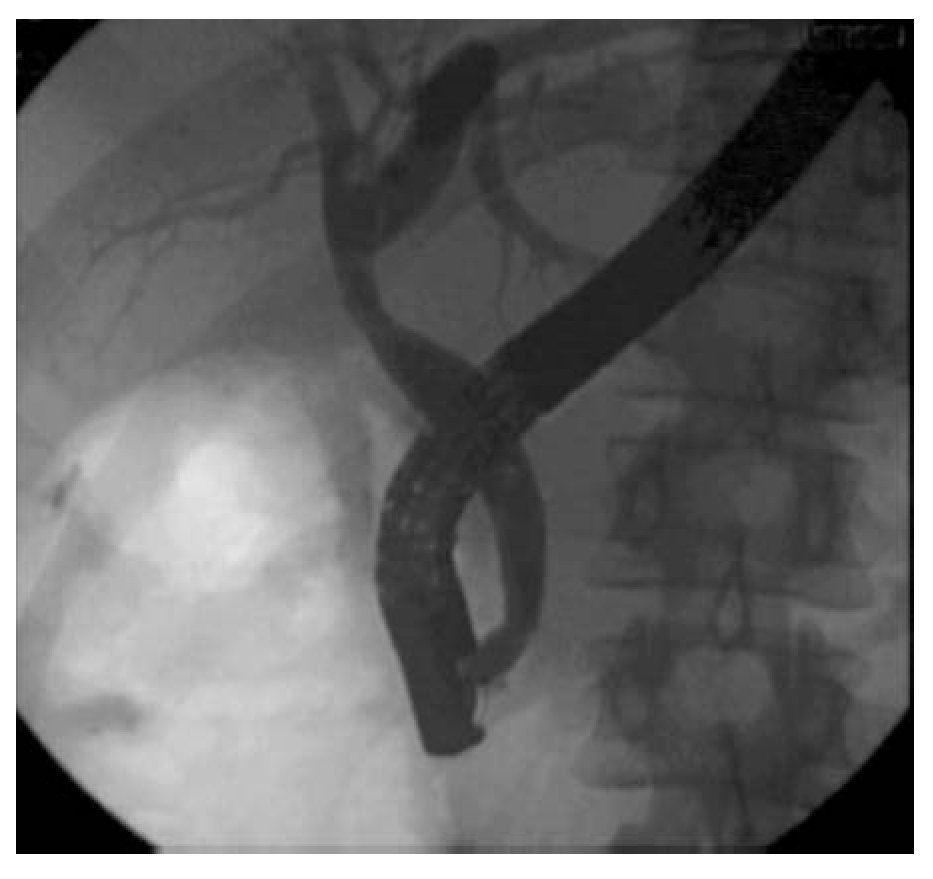
Procedure: The patient underwent ERCP using moderate sedation. The common hepatic duct (CHD) was cannulated using an Autotome RX 44 sphincterotome and 0.035" guidewire (Boston Scientific, Natick, MA). Cholangiography confirmed interruption of the CHD. In addition, contrast extravasation consistent with a bile leak was seen distal to the ligated segment. The sphincterotome was exchanged for an Artifon catheter. Under fluoroscopy, the 18-gauge needle was advanced from the sheath and into the proximal CHD as it punctured through the center of the ligated stump. The guidewire was then advanced into the proximal CHD (Figure 3a, 3b). An 8.5Fr x 10 cm plastic stent was placed. Thirty days later, the stent was removed and the stricture was dilated with an 8 mm balloon. Three plastic 10Fr, 10 cm long stents were positioned across the tract (Figure 4). Six months later repeat cholangiography demonstrated resolution of the bile leak and mild residual narrowing of the CHD (Figure 5). Stents were not reinserted. The patient remains well 18 months later with normal labs.
¿ Figure 3a. Schematic illustration of needle puncture through the center of ligated stump, with insertion of a guide wire into the proximal CHD. 3b. Fluoroscopic image demonstrating guidewire passage into the proximal CHD after puncture access with the needle catheter.
¿ Figure 4. Fluoroscopic image demonstrating three plastic stents bridging the CHD tract.
¿ Figure 5. Follow-up cholangiogram shows complete resolution of the bile leak and minimal residual narrowing of the CHD tract.
¿ Discussion
The optimal treatment of post-cholecystectomy bile duct injury is dependent on early recognition, taking into consideration the anatomic location and severity of the lesion. In minor cystic or bile duct leaks (Amsterdam type A and B), biliary sphincterotomy or stenting is effective. Strictures without bile leakage (Amsterdam type C lesions) can often be managed non-operatively with dilatation and stenting. Although successful endoscopic treatment of a completely transected bile duct (Amsterdam type D) has been reported early after cholecystectomy,4 the presence of clips at the distal stump and the lack of continuity between biliary segments usually mandate operative repair.2
Surgical repair of post-operative biliary injuries is technically challenging and carries a high risk of early and late complications.5,6 Combined endoscopic and percutaneous approaches have been attempted to treat severe strictures in selected cases.7,8 In the present case a specialized needle catheter afforded access to the proximal biliary tree across the ligated segment. This allowed for successful non-surgical management. As long as the lesion is short enough and can be adequately traversed by the needle puncture, this endoscopic technique allows successful creation of a permanent internal fistula. This method is comparable to what has been described using percutaneous interventional techniques and avoids the need for external puncture and catheters.7,8 We believe this approach is a promising non-surgical alternative in patients with short length transections of the bile duct.
Correspondence: Everson L. A. Artifon, M.D., Ph.D.
Associate Professor. School of Medicine, Sao Paulo University.Director, Biliary and Interventional Endoscopy - Ana Costa Hospital Rua Guimaraes Passos, 260-Apto 121. Vila Mariana, Sao Paulo-SP, Brazil, 01508-010.
Phone / Fax: 55-11-3069-6221.
Email: eartifon@hotmail.com