The laparoscopic approach to bowel obstruction is still controversial.
ObjectiveTo evaluate our initial results in the laparoscopic treatment of bowel obstruction.
Material and methodsA retrospective study on patients diagnosed with bowel obstruction that underwent laparoscopic surgery within the time frame of January 2008 to June 30, 2012. The variables employed were: age, sex, occlusion etiology, previous surgeries, clinical progression, pneumoperitoneum creation, use of an auxiliary incision, anesthesia duration, conversion rate, postoperative hospital stay, time needed to tolerate liquids, and complications.
ResultsTwenty-six patients, 18 women (69.2%) and 8 men (30.8%), with a mean age of 64.35 years (range: 21-92 years) were analyzed. The most frequent obstruction etiology was secondary to adhesions and presented in 12 cases. Nine patients (34.6%) underwent a completely laparoscopic approach and laparoscopy was complemented by an auxiliary incision in another 9 patients (34.6%), resulting in 18 cases (69.2%) of successful laparoscopic approach. Eight patients (30.8%) required conversion to open surgery. The mean anesthesia duration was 95min (range: 55-165min), mean postoperative hospital stay was 6 days (range: 3-72 days), and the mean amount of time needed to tolerate liquids was 3 days (range: 1-10 days). The patients that underwent complete laparoscopic approach presented with shorter hospital stay, they were able to ingest liquids earlier, and they presented with a lower number of postoperative complications; this latter variable was the only one that was statistically significant.
ConclusionsThe initial results of our experience were good, although more patients are needed in order to standardize and extend the use of this technique.
El abordaje laparoscópico de la obstrucción intestinal continúa siendo controvertido.
ObjetivoEvaluar nuestros resultados iniciales en el tratamiento laparoscópico de la obstrucción intestinal.
Material y métodosEstudio retrospectivo de pacientes diagnosticados de oclusión intestinal, e intervenidos mediante laparoscopia, desde enero de 2008 hasta el 30 de junio de 2012. Las variables empleadas fueron: edad, sexo, etiología de la oclusión, cirugías previas, evolución clínica, realización del neumoperitoneo, uso de incisión de asistencia, tiempo anestésico, tasa de conversión, días de estancia postoperatoria, tiempo hasta la tolerancia a líquidos, complicaciones.
Resultados26 pacientes, 18 mujeres (69.2%) y 8 varones (30.8%), edad media de 64,35 años (21-92 años). La etiología más frecuente de la oclusión fue secundaria a bridas, con 12 casos. En 9 pacientes (34.6%) el abordaje fue totalmente laparoscópico. En otros 9 pacientes (34.6%) se complementó con una incisión de asistencia. Así, el abordaje laparoscópico constituyó un éxito en 18 casos (69.2%). En 8 pacientes (30.8%) se convirtió a cirugía abierta. La mediana del tiempo anestésico fue de 95min (55-165min) de la estancia postoperatoria de 6 días (3-72días) y de la tolerancia de líquidos de 3días (1-10 días). Los pacientes en los que se efectuó un abordaje totalmente laparoscópico presentaron una menor estancia hospitalaria, una ingesta de líquidos más precoz y un menor número de complicaciones postoperatorias; solo esta última variable fue estadísticamente significativa.
ConclusionesLos resultados iniciales de nuestra experiencia son buenos, aunque se precisan más pacientes para poder estandarizar y extender el uso de esta técnica.
Bowel obstruction is the most frequent surgical complication in abdominal surgery and is one of the main reasons for emergency room visits. It is calculated that approximately 15-35% of the patients operated on will require hospitalization as a result of this complication, and that 2-5% of these patients will require surgical intervention, either for poor progression with conservative treatment or due to complete obstruction with the suspicion of intestinal ischemia.1–3
Traditionally, bowel obstruction has been regarded as an absolute contraindication for the laparoscopic approach due to the increased risk for iatrogenic injuries, the difficulty in managing dilated intestinal segments, and an inferior operating field.4–6
With the increased experience in this approach, this contraindication is now relative, because the abovementioned difficulties have been greatly reduced. Thus, patients operated on with this approach can benefit from the widely demonstrated advantages of laparoscopic surgery: less postoperative pain, less ileus, fewer wound infections, a lower incisional hernia rate, shorter postoperative hospital stay, esthetic benefits, and a decrease in future adhesions.4,5,7–9 This last advantage is perhaps the most important, given that the probability of a new episode of bowel obstruction in these patients increases by 30% after a first episode, by 40% after a second episode, and up to 60% after a third one.8
Despite these advances, the laparotomic approach is still regarded as the surgical treatment of choice for bowel obstruction and the role of laparoscopy in this field continues to be controversial.3,6,10
The aim of the present study was to evaluate the initial results of laparoscopic treatment of bowel obstruction in our center and to confirm whether it was a safe and effective approach in these cases.
MethodsA descriptive and retrospective analysis of all patients diagnosed with bowel obstruction and operated on with the laparoscopic approach at the Hospital General de Castellón (Comunidad Valenciana, Spain) within the time frame of January 2008 to June 2012 was carried out. The operations were performed by a total of 10 surgeons (staff specialists and residents in training).
The diagnosis of small bowel obstruction was made in relation to the clinical history, physical examination, and the radiologic findings. According to our center's existing protocol, if the patient had a past history of previous surgeries, and the clinical presentation was consistent with an intestinal sub-obstruction, initial management was conservative with a strict diet, a nasogastric catheter, and serum therapy. If after 24-48h the patient did not improve, then surgical intervention was decided upon. On the other hand, if the clinical presentation was consistent with symptoms of complete bowel obstruction, then the patient was taken directly to surgery (fig. 1).
If the patient required surgery, the approach depended on the specific criterion of the surgeon. In general terms, the criteria used for indicating the laparoscopic approach in bowel obstruction were the following:
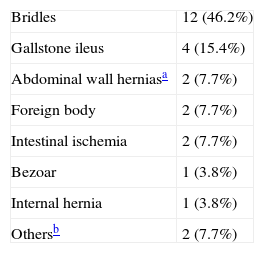
Inclusion criteriaThe approach was chosen by the surgeon responsible for each case, and basically, the patients that presented with the symptoms of bowel obstruction secondary to a foreign body (biliary lithiasis, bezoar, etc.) or the patients in whom there was suspicion of a single bridle as the cause of the bowel obstruction (see etiology in Table 1) were included.
Exclusion criteriaPatients with great abdominal distension, in other words, cases in which the small bowel segments were larger than 4cm in diameter measured through computerized axial tomography (CAT) scan, cases in which it was the surgeon's criterion that this large distension would make the correct visualization impossible after pneumoperitoneum creation, cases with complications or suspicion of intestinal fistula from the previous surgery, and cases of hemodynamic instability were all excluded.
Clinical variablesThe patients were divided into 3 groups: 1) a completely laparoscopic approach, 2) a laparoscopic approach with an auxiliary incision, and 3) conversion to open surgery.
The first group, as indicated by its name, includes those patients in whom the clinical presentation of bowel obstruction could be resolved exclusively through the laparoscopic approach. The second group included those patients in whom the procedure was carried out laparoscopically but with the necessity of making a small auxiliary incision in order to extract a foreign body or a segment of the small bowel left over from the resection. And the third group included those patients in whom it was necessary to convert to open surgery due to the impossibility of exclusively performing the surgery laparoscopically.
The different variables used in the present study were: age, sex, obstruction etiology, previous surgeries, clinical progression, pneumoperitoneum creation technique, the use of an auxiliary incision, anesthesia duration, conversion rate, postoperative hospital stay, the time needed to be able to tolerate liquids, and both intra and postoperative complications.
Conventional surgical techniqueThe patient was placed in the supine decubitus position with arms extended at the sides of the body. Both the main surgeon and the assisting surgeon stood at the patient's left side and the monitor of the laparoscope was on the right side. The pneumoperitoneum technique employed depended on the surgeon's individual preferences, but there was a greater tendency to use the open Hasson technique at the periumbilical level. When the Veress needle was used, it was inserted at the level of the left upper quadrant. After a brief examination of the peritoneal cavity, preferably with the 30° optic, a 5mm and a 10mm (sometimes a 12mm) trocar were introduced under direct vision. The location of the trocars was dependent on the intraoperative findings.
Using a pair of non-traumatic forceps, the surgeon began the examination of the small intestine starting at the ileocecal valve and reaching the transition zone, where the cause of the obstruction was found. This maneuver requires patience and care in order to avoid excessive traction on the intestinal segments, since they are very friable and there is a significant perforation risk; if possible the attempt should be made to traction the mesentery rather than the intestinal segments themselves.
When the cause is a bridle, it should be sectioned with scissors. Extreme care must be taken if electrocautery is used because there is a high risk for distant burns in other segments of the small bowel. The use of high energy instruments, such as the harmonica or bipolar scalpel, is not recommended. If there is any other cause that requires a minimal laparotomy (the extraction of a foreign body, bezoar, intestinal resection, etc.) it will be performed at the midline (taking advantage of the place where the Hasson needle is introduced) to extract the specimen and perform the resection and anastomosis outside of the abdomen.
If it is not possible to find the transition zone because the intestinal segments are very dilated or there are dense adhesions that impede advancing, then the procedure will be converted to open surgery.
Statistical analysisThe SPSS 19.0 program was used for the statistical analysis of the results. The variables were evaluated through the chi-square test and the Fisher probability test. The results were regarded as statistically significant when p < 0.05.
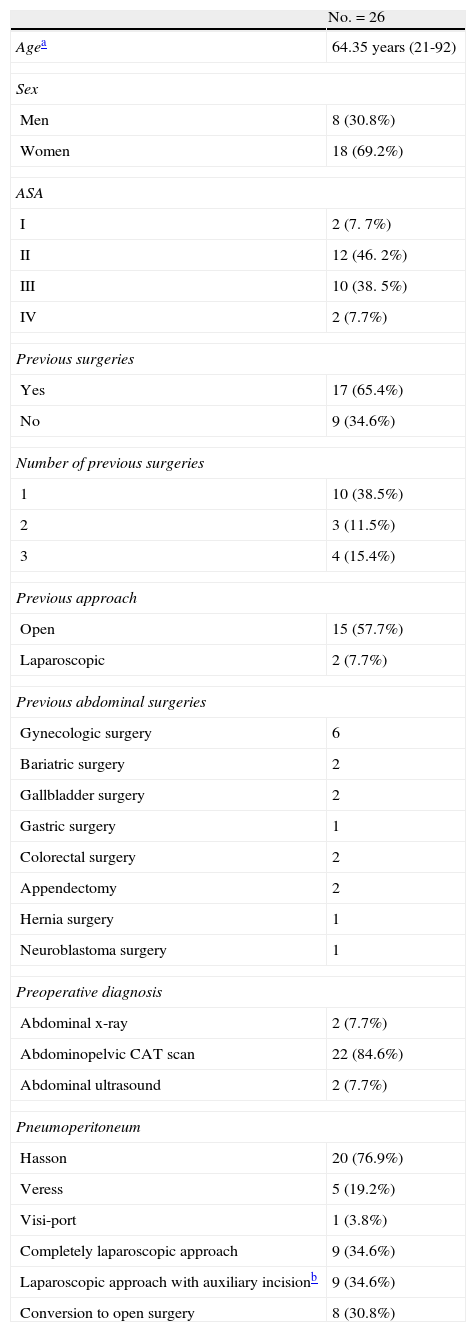
ResultsA total of 26 patients, 18 women (69.2%) and 8 men (30.8%), with a mean age of 64.35 years (range: 21-92 years), were included in the study. As shown in Table 1, bridles were the most frequent indication for the laparoscopic approach in our experience, with 12 cases (46.2%), followed by gallstone ileus with 4 cases (15.4%). The clinical characteristics and patient details are summarized in Table 2. This table shows that 17 patients (65.4%) presented with a past history of prior surgeries and there were up to 2 or more previous surgeries (almost 90% of the open approach cases) in 41.17% of these patients, which adds greater importance to the postoperative results obtained.
Clinical characteristics.
| No.=26 | |
| Agea | 64.35 years (21-92) |
| Sex | |
| Men | 8 (30.8%) |
| Women | 18 (69.2%) |
| ASA | |
| I | 2 (7. 7%) |
| II | 12 (46. 2%) |
| III | 10 (38. 5%) |
| IV | 2 (7.7%) |
| Previous surgeries | |
| Yes | 17 (65.4%) |
| No | 9 (34.6%) |
| Number of previous surgeries | |
| 1 | 10 (38.5%) |
| 2 | 3 (11.5%) |
| 3 | 4 (15.4%) |
| Previous approach | |
| Open | 15 (57.7%) |
| Laparoscopic | 2 (7.7%) |
| Previous abdominal surgeries | |
| Gynecologic surgery | 6 |
| Bariatric surgery | 2 |
| Gallbladder surgery | 2 |
| Gastric surgery | 1 |
| Colorectal surgery | 2 |
| Appendectomy | 2 |
| Hernia surgery | 1 |
| Neuroblastoma surgery | 1 |
| Preoperative diagnosis | |
| Abdominal x-ray | 2 (7.7%) |
| Abdominopelvic CAT scan | 22 (84.6%) |
| Abdominal ultrasound | 2 (7.7%) |
| Pneumoperitoneum | |
| Hasson | 20 (76.9%) |
| Veress | 5 (19.2%) |
| Visi-port | 1 (3.8%) |
| Completely laparoscopic approach | 9 (34.6%) |
| Laparoscopic approach with auxiliary incisionb | 9 (34.6%) |
| Conversion to open surgery | 8 (30.8%) |
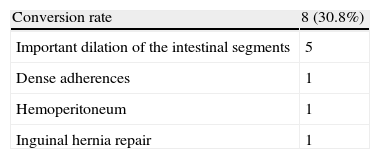
In 9 patients (34.6%) the operation could be performed exclusively with a laparoscopic approach. In another 9 patients (34.6%) the laparoscopic process was complemented with an auxiliary incision. This resulted in a total of 18 cases (69.2%) of successful laparoscopy. In 8 patients (30.8%) it was necessary to convert to an open procedure. The causes of conversion are shown in Table 3.
Given that the most frequent etiology of the purely laparoscopic approach was bowel obstruction secondary to bridles, laparoscopy had a success rate of 58.3% (5 conversions) in the management of this pathology.
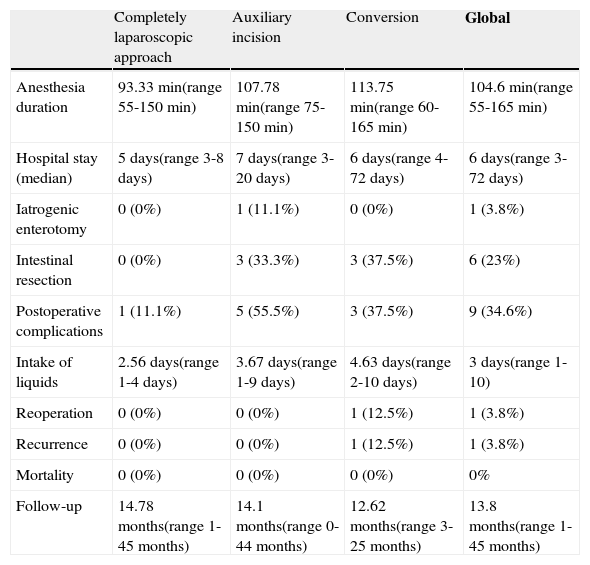
The group of patients whose procedure was exclusively laparoscopic, in absolute values, presented with shorter anesthesia duration (90min compared with 110min and 107.50min), shorter hospital stay (5 days compared with 7 days and 6 days), relatively fewer postoperative complications (11.1% compared with 33.3% and 37.5%), and an earlier intake of liquids (2.56 days compared with 3.67 days and 4.63 days).
Nevertheless, of all the results, only the lower complication rate reached statistically significant values (p = 0.046).
There were postoperative complications in 9 patients (34.6%), the most important of which were related to surgical wound infection, with 4 cases, one case of septic shock, one case of intestinal fistula, one case of intra-abdominal collection, and one case of respiratory distress. Despite the fact that some of the complications were relatively severe, there were no cases of death (0% mortality). Only one patient had to be reoperated on for an evisceration, precisely one of the patients whose unsuccessful laparoscopy was converted to open surgery, but no diagnosis was reached with either procedure.
Table 4 shows the comparison of results according to the approach employed.
Surgical treatment results.
| Completely laparoscopic approach | Auxiliary incision | Conversion | Global | |
| Anesthesia duration | 93.33 min(range 55-150 min) | 107.78 min(range 75-150 min) | 113.75 min(range 60-165 min) | 104.6 min(range 55-165 min) |
| Hospital stay (median) | 5 days(range 3-8 days) | 7 days(range 3- 20 days) | 6 days(range 4-72 days) | 6 days(range 3-72 days) |
| Iatrogenic enterotomy | 0 (0%) | 1 (11.1%) | 0 (0%) | 1 (3.8%) |
| Intestinal resection | 0 (0%) | 3 (33.3%) | 3 (37.5%) | 6 (23%) |
| Postoperative complications | 1 (11.1%) | 5 (55.5%) | 3 (37.5%) | 9 (34.6%) |
| Intake of liquids | 2.56 days(range 1-4 days) | 3.67 days(range 1-9 days) | 4.63 days(range 2-10 days) | 3 days(range 1-10) |
| Reoperation | 0 (0%) | 0 (0%) | 1 (12.5%) | 1 (3.8%) |
| Recurrence | 0 (0%) | 0 (0%) | 1 (12.5%) | 1 (3.8%) |
| Mortality | 0 (0%) | 0 (0%) | 0 (0%) | 0% |
| Follow-up | 14.78 months(range 1-45 months) | 14.1 months(range 0-44 months) | 12.62 months(range 3-25 months) | 13.8 months(range 1-45 months) |
Currently there are no randomized clinical trials in the scientific literature that compare the open and laparoscopic approaches for treating bowel obstruction.5 For this reason, and due to the lack of clear criteria for patient selection, the use of the laparoscopic approach has not been as extensive in bowel obstruction as it has been in many other digestive pathologies.
Different studies that support the safety of this approach in the hands of experienced surgeons have recently appeared.7,9,11–13 Despite the fact that there can be high conversion rates, they have been considerably reduced through increased experience and better patient selection. For example, in 1995 the Swiss Surgical Society designed a multicenter prospective study7 with 537 patients and obtained a 32.4% conversion rate. In 2001, Levar et al.11 conducted a retrospective multicenter study on 308 patients that produced a conversion rate of 54.6%. A recent meta-analysis by O¿Connor et al.12 that included 2,005 patients showed a lower conversion rate of 29%, that was reduced to 17% in the group of Mancini et al.13 In our experience the conversion rate was 30.8%, which is close to the figures published in the literature.
As mentioned above, good patient selection is essential for reducing this figure. The suspicion of a single bridle is the main indication for the laparoscopic approach (principally in patients with embryogenic adhesions or after appendectomy), together with obstruction due to foreign bodies, bezoars, or gallstone ileus. In this sense, we believe that a CAT scan prior to surgery is extremely useful in deciding upon both the indication for surgery and the approach.3,4
On the other hand, according to the bibliography reviewed and our own experience, the anesthetics used in relation to the patient's status, the suspicion of obstruction due to peritoneal carcinomatosis, intestinal distension greater than 4cm in imaging studies, and the suspicion of dense adhesions, can all be considered relative contraindications.3,5,14 Likewise, the use of the laparoscopic approach in patients suspected of presenting with ischemia or peritonitis is controversial and regarded by certain groups as relatively contraindicated. However, even if laparoscopy is technically feasible, the majority of authors, ourselves included,4,5 recommend an auxiliary incision for performing the resection and anastomosis, if they are necessary. Nevertheless, to reduce this conversion rate, more specific criteria need to be defined for case selection since surgeon preference continues to be the determining factor in the choice of approach.
Traditionally, another of the arguments against the laparoscopic approach for the surgical treatment of bowel obstruction has been the increase in unnoticed iatrogenic injuries during adhesiolysis. Wullstein et al.6 described figures close to 27% for the laparoscopic approach and 13% for the open approach. Different groups3,10 have recently published clearly lower figures (3-17%) that support the safety of this approach in the hands of expert surgeons. In our series, only one accidental enterotomy occurred; it was detected during surgery and promptly repaired. As we stated before, dissection must be performed with care, avoiding traction on the intestinal segments and taking great precautions when using electrocoagulation.4 By following these principles, the complication rate can be lowered. Likewise, another recommended surgical maneuver is pneumoperitoneum creation through an open technique to avoid intestinal injury due to patient adhesion syndrome. However, the rest of the techniques for creating the pneumoperitoneum are not contraindicated, and even though the open technique is the most frequently employed, the approach through the Veress needle is also used, as was the case with the patients in our study. In addition, it is essential to avoid placing the trocars at previous incision sites; they should be placed as far as possible from them. Likewise, the etiology of the obstruction should be identified during the operation. If that is not possible through laparoscopy, then the conversion to laparotomy is obligatory.4,5,8,10
Basically, the role of the laparoscopic approach in this field is to prevent future adhesions that would cause bowel obstruction recurrence, with the consequent socio-economic costs this implies. To the best of our knowledge, no report in relation to this aspect has been carried out for Spain, but in the United States such a cost is an estimated 1.3 billion dollars per year.4 The higher perioperative costs of laparoscopy could be compensated for by such annual expense.
The appearance of adhesions is clearly related to the use of laparotomy, with a possible presentation in 70-90% of the cases.4 This figure would be drastically reduced if the procedures were performed laparoscopically.
Our study had certain basic limitations in the selection of patients; this was carried out according to surgeon indication and so the surgeons with more experience in the laparoscopic approach operated on a greater number of patients. Furthermore, the results of the different approaches were compared and there may have been selection bias because those patients that underwent conversion to open surgery were the cases of greater technical difficulty, and so logically they would have a longer hospital stay and more complications. In our opinion, randomized prospective studies comparing the two approaches are necessary. Nevertheless, the laparoscopic approach to bowel occlusion is safe and reproducible, a fact that was supported by our series and that coincides with the international literature.4,5,7–9
In conclusion, good results in the treatment of bowel obstruction can be obtained with the laparoscopic approach, as long as the human and technical resources for performing it are available. Nevertheless, despite the increased experience with this approach, there is still a high conversion rate. Therefore, good patient selection is essential for reducing this figure. The experience of the surgical team is fundamental in these cases.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Fortea-Sanchis C, Priego-Jiménez P, Martínez-Ramos D, et al. Experiencia inicial en el abordaje laparoscópico de la obstrucción intestinal. Revista de Gastroenterología de México. 2013;78:219–224.