Peroral endoscopic myotomy has recently been developed and performed on patients with good results.
AimsTo evaluate the technical feasibility of peroral endoscopic full-thickness and partial thickness myotomy in a porcine model.
Material and methodsEighteen criollo pigs were randomly assigned to 2 groups: group A (partial-thickness myotomy) and group B (full-thickness myotomy). The mucosal defect proximal to the myotomy site was left open. On the seventh postoperative day the pig was euthanized and follow-up surgical exploration was performed. The duration of each procedure, postoperative progression of the animal, complications, and anatomopathologic findings were registered.
ResultsThe procedure was viable in all the pigs. The mean surgery duration was 81±35.3min (group A 51.11±11.12, group B 111±22.61; P<.05). The main complication during myotomy was subcutaneous emphysema (16%). The histopathologic study of the group A surgical specimens reported complete circular myotomy in all cases, and complete circular and longitudinal myotomy was reported in 100% of the group B sample.
ConclusionsThe endoscopic myotomy technique is feasible. Endoscopic partial-thickness myotomy was associated with shorter surgery duration and better results during the intraoperative period and the 7-day follow-up.
Recientemente la miotomía endoscópica por vía oral ha sido desarrollada y realizada en pacientes, con buenos resultados.
ObjetivoEvaluar la factibilidad técnica de la miotomía endoscópica por vía oral de espesor total y parcial en un modelo porcino.
Material y métodosDieciocho cerdos criollos se asignaron al azar a 2 grupos: grupo A (miotomía de espesor parcial) y grupo B (miotomía de espesor total). El defecto mucoso proximal al sitio de la miotomía se dejó abierto. Al séptimo día el cerdo fue sacrificado, realizándose exploración quirúrgica de seguimiento. Se registró el tiempo de cada procedimiento, la evolución del animal en el postoperatorio, la presencia de complicaciones y los hallazgos anatomopatológicos.
ResultadosEl procedimiento fue factible en todos los cerdos. El tiempo promedio fue de 81±35.3min (grupo A 51.11±11.12, grupo B 111±22.61; P<.05). La principal complicación transendoscópica fue el enfisema subcutáneo (16%). El reporte histopatológico de la pieza operatoria en el grupo A reportó miotomía circular completa en todos los casos, y el grupo B, miotomía circular y longitudinal completa en el 100% de la muestra.
ConclusionesLa técnica de miotomía endoscópica es factible. La miotomía endoscópica de espesor parcial se asoció a un menor tiempo quirúrgico, con mejores resultados durante el periodo transoperatorio y el seguimiento a 7 días.
Achalasia is a primary disorder of the motility of the esophagus of unknown cause that is characterized by aperistalsis of the esophageal body and, at times, by deterioration in the relaxation of the inferior esophageal sphincter.1
Esophagomyotomy continues to be the treatment of choice, and while it may not correct the esophageal aperistalsis, it does not allow natural disease progression, thus preventing long-term complications and significantly improving patient quality of life by reducing inferior esophageal sphincter pressure and favoring esophageal clearance.2
Anterior vertical extramucosal esophagomyotomy was first described by Ernest Heller in 1914. Then in 1918 it was modified by De Bruine Groeneveld who limited the procedure to an anterior myotomy, which involved a surgical incision of the circular and longitudinal fibers of the esophagus.3
As with other surgical procedures, the advent of minimally invasive surgery has reduced morbidity as well as hospital stay. However, minimally invasive surgical myotomy is still related to a perforation rate of 5 to 10% and a recurrence rate of 25 to 33% at 10-year follow-up.4
The recent emergence of the surgical approach through natural orifices has challenged laparoscopic access in the search for a less invasive procedure with the same risks, equivalent results, shorter hospital stay, a more comfortable postoperative progression, and more esthetic results to benefit the patients.5
Ortega et al. pushed the development of this new form of approach more than 3 decades ago.6 In 2007 Pasricha et al. published their experience with submucosal myotomy in pigs, limiting it to the internal muscle layer and closing the mucosal defect distal to the myotomy site.7
One year later, Inoue et al. successfully carried out the first myotomy in humans.8 And in 2011, these authors reported on a series of 116 cases with good short-term results and no serious complications.9
Nevertheless, there are still no reports on peroral endoscopic myotomy in Mexico, and so we considered it relevant to develop the endoscopic technique in a porcine model and evaluate the feasibility of its application in humans.
AimOur study aim was to analyze the technical viability of endoscopic full and partial-thickness myotomy in a porcine model.
MethodsA randomized experimental study was conducted after receiving the approval of the research and ethics committee of our institute.
Two endoscopists experienced in therapeutic endoscopy and trained in the peroral endoscopic myotomy technique (M.R.R. received his training at the European Institute of TeleSurgery of the Institute for Research Against Digestive Cancer, Strasbourg, France, and J.J.H.E. took a PG-POEM training course offered by the Society of American Gastrointestinal and Endoscopic Surgeons, San Diego, California, USA) coordinated the procedures.
Eighteen Criollo female pigs with a mean weight of 18kg (range: 16-20kg) were randomly assigned to 2 groups: 9 pigs in group A that underwent peroral endoscopic partial-thickness myotomy and 9 pigs in group B that underwent peroral endoscopic full-thickness myotomy.
The pigs were kept in a fasting state for 12h prior to the procedure and they were all given enrofloxacin at the prophylactic dose of 2.5-5mg/kg IM.
Endoscopic technique: Peroral endoscopic myotomyThe animals were given tiletamine/zolazepam (4.4mg/kg IM) and xylazine (2.2mg/kg IM). Once they were sedated, a mask was put in place for passing oxygen and later for passing isoflurane at 3% for their anesthetization. Each pig was intubated and monitored, and anesthesia was kept at 2% isoflurane.
Upper endoscopy using a Pentax (EPM-3500) processor and an EG 29 gastroscope was performed.
The submucosa was infiltrated with 0.9% saline solution 12cm above the gastroesophageal junction with an injection needle (Olympus NM-200U-0423) in order to create a welt (fig. 1).
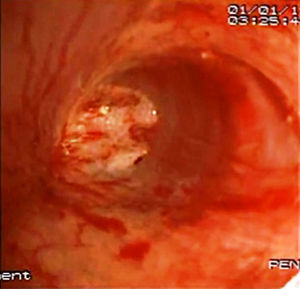
An incision with electrocoagulation was made in the wall of the welt (precut needle knife Olympus NeedleCut 3V, 30W pure cut) (fig. 2) in order to introduce the endoscope into the mucosa and dissect the submucosal layer up to the cardia (fig. 3).
Myotomy of 8cm in length (6cm esophageal and 2cm gastric) was performed at this site (fig. 4). In the group A pigs, only the internal muscle layer was sectioned, performing a partial-thickness myotomy, and in the group B pigs, both the internal and external muscle layers were sectioned. The mucosal defect was left open in both groups.
Atmospheric air was used for the insufflation, and depending on equipment availability at the bioterium, a hood (Olympus MH-588) or balloon (Boston Scientific CRE™) dilator was used for the creation of the submucosal tunnel.
The postoperative follow-up was carried out by the lead researcher and the veterinarian and lasted for 7 days, which was the period of time the majority of acute complications were expected to be found.
The duration of each of the procedures, the postoperative progression of the animal (changes in habitual activities, ability to eat food, loss of appetite, weight gain or loss, vital signs), and the presence of complications were recorded.
On the seventh postoperative day, the pigs were euthanized. Thoracic, mediastinal, and peritoneal exploration was carried out in the search for signs of perforation and infection. The macroscopic findings during autopsy and the anatomopathologic findings were registered.
Statistical analysisThe statistical inference analysis was done using the Stat® 8 and Minitab® 16 software. The following tests were employed: The Z test, the Fisher exact test, the one-way analysis of variance, and the non-parametric analysis of variance of the Mann-Whitney test.
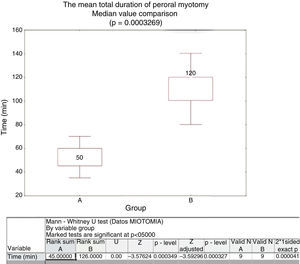
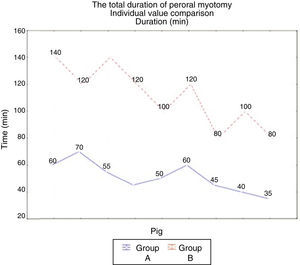
ResultsThe procedure was viable in all the pigs. The mean surgery duration was 81 ± 35.3min; group A 51.11 ± 11.12, group B 111 ± 22.61 (figs. 5 and 6).
The main complication during myotomy was subcutaneous emphysema that presented in 16% of the sample (all in group B).
Self-limited and transitory bleeding presented in 16% of the sample, mainly during the creation of the submucosal tunnel and the myotomy, with no difference in presentation between the two groups.
Only one pig presented with significant blood loss during full-thickness myotomy, requiring combination therapy (injection of saline solution at 0.9%+adrenaline, monopolar coagulation).
Esophageal mucosa tearing at the entrance site presented in the first 7 cases (group A 25% and group B 33%) and one group B pig presented with perforation of the gastric mucosa.
During follow-up the animals were found to be healthy, with no fever or loss of appetite. There were no differences in relation to changes in customary activity, the toleration of oral food intake, and weight gain or loss.
Autopsy revealed a 2mm sealed perforation in one animal from group B. None of the pigs showed signs of mediastinitis or peritonitis.
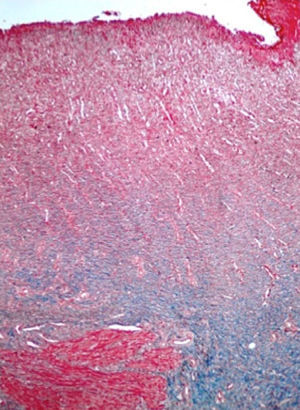
The histopathologic study of the surgical specimens reported complete circular myotomy in all the group A cases and complete circular and longitudinal myotomy in 100% of the group B animals (fig. 7).
DiscussionParischa et al. recently developed the concept of the submucosal tunnel that has made the development of peroral endoscopic myotomy feasible. Peroral endoscopic myotomy for the treatment of achalasia has been performed in humans since 2008 and produces excellent short-term results with no serious complications.10
The aim of both endoscopic and laparoscopic myotomy is to reduce inferior esophageal sphincter pressure and facilitate esophageal clearance in patients presenting with achalasia.11 Compared with laparoscopic myotomy, endoscopic myotomy has the following advantages:
First of all, because it is an incision-free procedure, it has superior esthetic results; the length of the myotomy can be flexible and is chosen by the operator, whereas the laparoscopic technique is limited by the difficulty in approaching the superior mediastinum; and finally, endoscopic myotomy is carried out through the endoluminal route with a low risk for injuring adjacent organs.12
However, there are also disadvantages. For example, it is a recent technique with no long-term results; the endoscopic approach requires general anesthesia and complex preparations; it has a similar duration to laparoscopic myotomy (100min); and it is not associated with the antireflux procedure, which could induce a greater gastroesophageal reflux potential than with the conventional laparoscopic technique.13
Finally, achalasia is a rare disease that requires referral centers in order to consolidate the technique.
We found no reports on peroral endoscopic myotomy in Mexico in our review of the literature. Even though the present study evaluated feasibility in an animal model, it is significant for being the first Mexican report. Similar studies are being conducted at other centers in the country, but the results have yet to be published.
In our experience, partial-thickness myotomy was associated with shorter surgery duration and fewer complications, which we attribute to having limited the myotomy to the circular layer. Bonin et al. found no significant differences in the reduction of the inferior esophageal sphincter pressure when partial-thickness myotomy was compared with the full thickness procedure in 24 pigs (p=0.82), but they did find reduced pressure in relation to the length of the myotomy. Even though full-thickness myotomy is feasible, it is probably not necessary.14 In addition, more studies on myotomy length and depth are required in order to have conclusive results.
In the description by Inoue et al. of the endoscopic technique, the dissected mucosal flap was joined together with endoclips. In our experimental study, the mucosal defect was left open (open flap); this did not appear to have an influence on the progression of the pigs, even in the pig from group B (pig 15) that presented with a perforation that was diagnosed postmortem.
To guarantee safety in humans, the endoscopic technique needs to be established and the material must be adequate.
First, it is important to select the appropriate type of scalpel for sectioning esophageal muscle. We used a pre-cut needle knife (Olympus NeedleCut 3V), which did not let us adequately estimate the depth of the tip. Despite this fact, our study was feasible. Inoue et al. used an endoscopic scalpel (triangle-tip knife) that they considered safe because it can selectively permit traction and cut the muscle fibers.15
The disadvantage we identified with the use of the balloon was the difficulty in placing it inside the submucosal space, in turn, facilitating loss of the dissection plane. The use of the hood allowed for adequate visual control and hemostasis. The endoscopic dissection technique reduced the amount of air that was insufflated for maintaining adequate visualization. Eleftheriadis et al. recommend using the hood in order to have precise visual control during the creation of the submucosal tunnel and the myotomy.16 During the present study, we did not find a greater incidence of complications with one technique or the other.
There were no serious complications in our study. Subcutaneous emphysema presented in 16% of the sample - all cases were in the full-thickness myotomy group. This had no repercussions on the postoperative progression of the animals. Ren et al. analyzed the complications during and after the peroral endoscopic myotomy in a case series of 119 patients. The main complication was subcutaneous emphysema that occurred in 22% of the patients during the myotomy, but no additional treatment was required for this complication.17,18.
There are important ethical considerations to be taken into account in the training process of peroral endoscopic myotomy.
Up to the present, results have been promising. Nevertheless, the low incidence of achalasia, together with potential complications (mediastinitis, bleeding, necrosis of the esophageal mucosa, esophageal perforation, peritonitis, etc.) has limited the expansion of the technique. The basic requisites proposed for surgeons and gastroenterologists that wish to perform this new technique are: a) certification in gastrointestinal endoscopy, b) knowledge of the anatomy of the esophagus and the gastroesophageal junction, c) knowledge of the pathophysiology of achalasia, and d) training in peroral endoscopic myotomy. A proposed training model encompasses: a first phase of observing the procedure performed by qualified specialists; a second phase of training on inanimate and animate models (the pig is the proposed animal model because its anatomy is similar to that of humans); a third phase of training on humans under the supervision of qualified specialists; and finally, the performance of the procedure on humans.17
The present study has several limitations. In the first place, we did not measure the inferior esophageal sphincter pressure before and after the endoscopic myotomy and therefore its effectiveness in this respect could not be evaluated. Secondly, the porcine model is not ideal because it is not equivalent to a patient with achalasia. However, we believe that sharing our experience will provide endoscopists in training with useful information for shortening the learning curve.
ConclusionsThe technique of peroral endoscopic myotomy was feasible and the complications were related to the standardization of and the experience in the procedure.
Leaving the mucosal flap open did not appear to have an impact on the post-endoscopic progression of the pigs.
Endoscopic partial-thickness myotomy was associated with shorter surgery duration and better results throughout the intraoperative period and the 7-day follow-up.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
The authors wish to thank Dr. Ramón García Cortes for the use of the Bioterium facilities and Dr. Eduardo Cárdenas Lailson for the methodological orientation and article supervision.
Please cite this article as: Quiroz-Guadarrama CD, Rojano-Rodríguez M, Herrera-Esquivel, JJ, et al. Miotomía endoscópica por vía oral de espesor total y parcial. Estudio de factibilidad en un modelo animal. Revista de Gastroenterología de México. 2013;78:225–230.