Cystic fibrosis (CF) is a genetic disease whose gastrointestinal compromise mainly involves the pancreas, bile ducts, and liver. Our aim was to analyze abdominal ultrasound findings.
MethodsA retrospective, descriptive study was conducted on adults (patients ≥ 16 years of age) diagnosed with CF, within the time frame of 2006-2019. Clinical and genetic parameters, body mass index, forced expiratory volume in one second, pancreatic insufficiency, CF-related diabetes, cirrhosis secondary to CF, and abdominal ultrasound images were analyzed.
ResultsSeventy patients, 39 of whom were men (55.8%), had a mean age of 27 years and a mean body mass index of 21.3 ± 2.8 kg/m2 (r: 17-30.9). Forty-seven (67.1%) presented with pancreatic insufficiency, 6 (8.5%) with cirrhosis secondary to CF, and 21 (30%) had CF-related diabetes. Median forced expiratory volume in one second was 47% and the F508del mutation was found in 56.1%. Images of the pancreas: no pathologic findings in 49 (70%), increased echogenicity in 18 (25.7%), and cysts in 3 (4.3%). Gallbladder images: microgallbladder in 3 (4.2%), biliary sludge in 2 (2.8%), gallstones in 7 (10%), and a history of cholecystectomy in 4 (5.8%). Liver and spleen images: no pathologic findings in 47 (67.2%), homogeneous hepatomegaly with splenomegaly in 2 (2.8%), a heterogeneous pattern of the parenchyma in 11 (15.8%), increased echogenicity in 4 (5.7%), and heterogeneous echo patterns, lobulated liver contour, and splenomegaly in 6 (8.5%).
ConclusionAbdominal ultrasound is a safe, low-cost technique that enables the identification of some degree of chronic liver and pancreatic diseases, improving the approach and follow-up decisions in adult patients with CF.
La fibrosis quística (FQ) es una enfermedad genética cuya afectación gastrointestinal implica principalmente al páncreas, los conductos biliares y el hígado. El objetivo es analizar los hallazgos ecográficos abdominales.
MétodosEstudio retrospectivo, descriptivo de adultos ≥16 años con diagnóstico FQ, periodo evaluado 2006-2019. Se analizaron los parámetros clínicos, genéticos, el índice de masa corporal, el volumen espiratorio forzado en el primer segundo, insuficiencia pancreática, diabetes relacionada con FQ, cirrosis secundaria a FQ e informes de la ecografía abdominal.
ResultadosSetenta pacientes, 39 (55.8%) varones, mediana de edad: 27 años. Media de índice de masa corporal 21.3 ± 2.8 kg/m2 (r: 17-30.9). Insuficiencia pancreática en 47 (67.1%), cirrosis secundaria a FQ en 6 (8.5%), diabetes relacionada con FQ en 21 (30%) pacientes. Mediana volumen espiratorio forzado en el primer segundo 47%. F508del en el 56.1%. Imágenes en páncreas: sin hallazgos patológicos en 49 (70%), aumento de la ecogenicidad en 18 (25.7%) y quistes en 3 (4.3%). Imágenes en vesícula biliar: microvesícula en 3 (4.2%), barro biliar en 2 (2.8%), cálculos biliares en 7 (10%), antecedente de colecistectomía en 4 (5.8%). Imágenes en hígado y bazo: sin hallazgos patológicos en 47 (67.2%) hepatomegalia homogénea con esplenomegalia en 2 (2.8%). Patrón heterogéneo del parénquima en 11 (15.8%), ecogenicidad aumentada en 4 (5.7%) ecoestructura heterogénea, bordes lobulados y esplenomegalia en 6 (8.5%).
ConclusiónLa ecografía abdominal es una técnica segura y de bajo costo que permite identificar algún grado de hepatopatía crónica y pancreática mejorando las decisiones en el abordaje y seguimiento de pacientes adultos con FQ.
Cystic fibrosis (CF) is a multisystemic, monogenic recessive autosomal hereditary disease characterized by the presence of mutations in the gene located on chromosome 7 that encodes the cystic fibrosis transmembrane conductance regulator (CFTR) protein1.
Messenger RNA (mRNA) of the CFTR was identified through immunohistochemistry techniques in submucosal glands of the human lung, sweat glands, pancreas, intestinal crypts, and bile ducts2. At present, 2,104 CF-causing mutations have been described and are listed in the Cystic Fibrosis Genetic Analysis Consortium3.
In Argentina, under the neonatal screening law (Law 26.279), serum immunoreactive trypsin, together with the search for other congenital and/or genetic diseases, is determined. Its incidence in the country is approximately 1:7,000 live births, and according to the National Cystic Fibrosis Registry (RENAFQ, the Spanish acronym), a total of 1,458 cases were registered for 2020, 851 (58%) of which were individuals above 12 years of age4,5. Survival has increased in recent years and the current mean survival is close to 50 years6, as a result of professional multidisciplinary care teams and pharmacologic advances. The emergence of CFTR modulators in the past decade, whose action is based on correcting the function of the altered CFTR protein, according to the types of mutations identified, stand out7.
Abdominal ultrasound is a safe and accessible diagnostic method for characterizing digestive disease associated with cystic fibrosis. Complete fat replacement is the most common radiologic pancreatic abnormality and hyperechogenicity of the pancreas is the most frequent ultrasound finding in patients with cystic fibrosis and exocrine pancreatic insufficiency. Pancreatic cysts are small (1 to 3 mm in diameter). A total of 12-24% of the patients with CF have gallstones and a frequency of small gallbladders (microgallbladder)8. Abdominal ultrasound also plays a fundamental role in diagnosing cystic fibrosis-associated liver disease (CFLD), given that it can evaluate changes in the liver parenchyma consistent with cirrhosis of the liver, steatosis, and bile duct abnormalities9.
The aim of the present study was to analyze the results of the ultrasound evaluation of the gallbladder, pancreas, liver, and spleen, in adult patients diagnosed with CF, seen at the cystic fibrosis unit of our hospital.
MethodsA retrospective, descriptive analysis was conducted on patients ≥ 16 years of age, seen at the CF unit, within the time frame of January 2006 and June 2019. The diagnosis of CF was based on the clinical criteria, sweat test and/or detection of the two CFTR gene mutations.
The following variables were analyzed: age, sex, age at diagnosis, genetic study, body mass index (BMI), forced expiratory volume in one second (FEV1), fecal elastase, fasting glucose, and glucose level 2 h after oral 75 g glucose overload.
Fecal elastase concentration < 200 μg/g was established for diagnosing pancreatic insufficiency (PI). The diagnosis of underlying cirrhosis was made through the finding of histologic changes consistent with liver tissue, due to macroscopic characteristics of the liver during the surgery or clinical and laboratory signs of the disease10. The diagnosis of cystic fibrosis-related diabetes (CFRD) was made when fasting glucose was above 126 mg/dl and/or was above 200 mg/dl at 2 h.
The BMI was calculated using the weight/height2 (kg/m2) formula. Respiratory function was evaluated by the forced expiratory volume in one second (FEV1) measurement.
The genetic study included the search for mutations, using the reverse allele specific oligonucleotide (ASO)-PCR and INNO-LiPA CFTR 19 and 17 (Innogenetics) methodology.
A diagnostic imaging specialist reviewed the written reports and abdominal ultrasound images that were performed at our hospital and at other institutions.
The ultrasound studies were carried out after an 8 h fast, utilizing a 2009 Phillips HD7 echograph (convex [C] and linear [L] transducers) and a 2007 ESAOTE MYLAB 40 echograph (convex [C], linear [L], and endocavity [E] transducers), under standard conditions. The echographic signs included the evaluation of 9 parameters11.
The cystic images in the pancreas were divided into generally round anechoic structures and oval structures larger than 1 cm (macroscopic cysts).
Pancreatic lipomatosis was defined when the pancreatic echogenicity was partially or completely greater than that of the liver (or the kidney, in the case of liver hyperechogenicity).
Gallstones were demonstrated through a typical acoustic shadow in the gallbladder.
Biliary sludge was defined as a level of multiple fine intravesical echoes located in a descending position.
Microgallbladder was defined as a gallbladder under 2-3 cm in length and under 0.5-1.5 cm in width.
Hepatic steatosis was defined through the finding of an increase in “bright liver” echogenicity, in relation to the renal cortex.
The longitudinal diameter of the right liver lobe is usually utilized to measure the size of the liver. A value above 15.5 cm was considered hepatomegaly.
The ultrasound parameters utilized to evaluate liver cirrhosis were liver size, lobulated liver contour (irregularity of the hepatic surface), heterogeneity of the liver parenchyma, nodularity, and splenomegaly.
Splenomegaly was considered when the bipolar diameter was greater than 13 cm.
Statistical analysisThe data were collected on a worksheet, utilizing Microsoft Excel 2010 software, and processed using MedCalc version 18.9. The results were grouped in tables for easier management and the values were expressed as mean ± 1 SD or median and range. The qualitative variables were compared using the chi-square test or the Fisher’s exact test and the quantitative variables were compared using the Student’s t test. Statistical significance was set at a p < 0.05.
Ethical considerationsThe present manuscript contains no personal information that could identify the patients, all of whom signed written statements of informed consent, accepting to be evaluated, as well as consenting to the analysis and publication of the resulting data. This study meets the current bioethical research norms and was approved by the hospital’s ethics committee.
ResultsA total of 70 adult patients (≥ 16 years of age), diagnosed with CF and treated by a multidisciplinary team from a center for adults in La Plata, Argentina, were included in the study. Thirty-one of the patients were women (44.2%) and 39 were men (55.8%), with a median age of 27 years (range: 16-65). Median age at the time of diagnosis was 2 years (range: 4 months-26 years).
A genetic study was performed on 65 patients. The F508del mutation was the most frequent and it was found in 73/130 of the alleles analyzed (56.1%).
The mean BMI was 21.3 ± 2.8 kg/m2 (range 17-30.9).
The median FEV1 was 47% (range: 11-107).
The pancreatic status characteristics showed that 47/70 (67.1%) of the patients presented with PI and 23/70 (32.9%) presented with pancreatic sufficiency (PS). CFRD was diagnosed in 21/70 (30%) of the patients.
Six (8.5%) patients in our series were diagnosed with cirrhosis of the liver, and it was associated with pancreatic insufficiency in all of them.
Table 1 describes the study variables with their absolute and relative distribution. Table 2 shows the ultrasound findings.
Absolute and relative distribution of the variables analyzed in the study patients with CF (n = 70).
| Variables | n = 70 |
|---|---|
| Sex | |
| Women n (%) | 31 (44.2) |
| Men n (%) | 39 (55.8) |
| Age (years), median (range) | 27 (16-65) |
| BMI (kg/m2) (x ± SD) | 21.3 ± 2.8 |
| FEV1 (median and range) % | 47 (11-107) |
| PI (elastase < 200 ug) n (%) | 47 (67.1) |
| F508del n (%) | 73/130 alleles (56.1) |
| CFRD n (%) | 21 (30) |
| Cirrhosis secondary to CF n (%) | 6 (8.5) |
BMI: body mass index; CF: cystic fibrosis; CFRD: cystic fibrosis-related diabetes; FEV1: forced expiratory volume in one second; PI: pancreatic insufficiency; SD: standard deviation.
Abdominal ultrasound results in adult patients with CF.
| Alterations detected in the abdominal ultrasound | n (%) |
|---|---|
| Pancreatic findings | 21/70 (30) |
| Pancreatic lipomatosis | 18 (25.7) |
| Pancreatic cysts | 3 (4.3) |
| No pathologic findings | 49 (70) |
| Gallbladder findings | 16/70 (22.8) |
| Biliary sludge | 2 (2.8) |
| Microvesicles | 3 (4.2) |
| Gallstones | 7 (10) |
| Cholecystectomy | 4 (5.8) |
| No pathologic findings | 54 (77.2) |
| Liver and splenic findings | 23/70 (32.8) |
| Homogeneous hepatomegaly with splenomegaly | 2 (2.8) |
| Increased liver echogenicity | 4 (5.7) |
| Heterogeneous echo patterns, lobulated liver contour, and splenomegaly | 6 (8.5) |
| Heterogenous liver echo patterns | 11 (15.8) |
| No pathologic findings | 47 (67.2) |
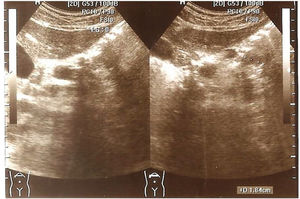
Findings in the pancreas. Of the 70 patients, 21 (30%) had a pancreatic alteration revealed in the ultrasound: 18 (25.7%) patients had pancreatic lipomatosis and 3 (4.3%) had pancreatic cysts (Figs. 1 and 2). There were no pancreatic alterations identified through ultrasound in the remaining 70% of the patients.
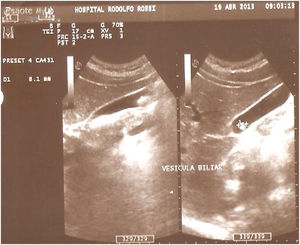
Findings in the gallbladder. Alterations of the gallbladder revealed in the ultrasound studies were present in 16/70 (22.8%) of the patients: biliary sludge in 2 (2.8%), microgallbladder in 3 (4.3%), gallstones in 7 (10%), and a history of cholecystectomy in 4 (5.7%) (Fig. 3). No pathologic alterations were demonstrated through ultrasound in 54/70 (77.2%) of the patients.
Findings in the liver and spleen. A total of 23/70 (32.8%) patients presented with anomalies in the liver and/or spleen: 2 (2.8%) had homogeneous hepatomegaly with splenomegaly, 4 (5.7%) had increased hepatic echogenicity, 6 (8.5%) presented with ultrasound parameters consistent with cirrhosis of the liver (heterogeneous echo response in the liver parenchyma, lobulated liver margin, and splenomegaly) (Fig. 4). Eleven (15.8%) patients had a heterogeneous echo response, whereas 47/70 (67.2%) had no findings demonstrable through ultrasound in the liver or spleen.
A comparative analysis was carried out with respect to the ultrasound findings between patients diagnosed with CF in childhood and those diagnosed in adulthood. No significant difference was found between the two groups, regarding alterations of the pancreas (p = 0.4) or the gallbladder (p = 0.2), or hepatosplenic anomalies (p = 0.2). Upon analyzing the ultrasound findings between patients with CFRD and non-diabetic patients, there were no significant differences between the two groups regarding alterations of the pancreas (p = 0.2) or the gallbladder (p = 0.3), or hepatosplenic (p = 0.7) anomalies. There was a significant difference in the pancreatic hyperechogenicity (lipomatosis) analysis between the patients with normal exocrine function and those with pancreatic insufficiency (PI) (p = 0.002).
DiscussionAbdominal ultrasound as a complementary study should be carried out every six months, yearly, or in relation to medical criteria, according to the diagnostic and treatment guidelines for patients diagnosed with CF12.
Increased echogenicity of the pancreas and the loss of the fine lobular pattern of the pancreas as typical findings in the abdominal ultrasound are established, in accordance with the processes described by the pathologic anatomy8. In our cohort of 70 patients, 21 (30%) had pancreatic hyperechogenicity. The difference in the results of the pancreatic hyperechogenicity (lipomatosis) analysis between the patients with normal exocrine pancreatic function and those with pancreatic insufficiency (PI) was statistically significant (p = 0.002). In their study on 21 patients above 15 years of age, diagnosed with CF, Engjom et al.13 described a directly proportional relation of hyperechogenicity to the loss of pancreatic function, as a consequence of pancreatic fat replacement. They concluded that magnetic resonance imaging evaluated pancreatic fat infiltration more accurately, surpassing ultrasound, as a more valid and reliable marker of exocrine pancreatic insufficiency in CF. Concurring with the results of those authors, we detected pancreatic cysts only in patients with PI, and detected no pancreatic calcifications in our case series.
Our results differed from those of Dietrich et al.14, regarding the pancreatic ultrasound findings described in 66 adult patients with CF. They reported the presence of ultrasound signs consistent with pancreatic lipomatosis in 35% of the patients versus 25.7% of the cases observed in our case series. We underline the fact that pancreatic cysts were detected in 18% of the patients in that case series, as opposed to only 4.3% of the patients in our study.
CFTR expression in the gallbladder is one of the highest in all human tissue15. For some time, patients with CF have been known to develop gallbladder abnormalities that can include a small or absent gallbladder, gallbladder dysfunction, symptomatic gallstones, and malignancy16. In reference to ultrasound findings in the gallbladder of 114 patients diagnosed with CF, in children as well as in adults, Tabori et al.17 demonstrated a 3% frequency of gallstones, whereas microgallbladder was detected in 21%. In the study by Dietrich et al.14, microgallbladder was found in 18/72 (25%) of adults with CF, whereas no subjects had undergone cholecystectomy. Those findings differ from ours, with respect to the fact that gallstones were the most frequent abnormality detected through ultrasound (10%). Only 4 of our patients had a history of cholecystectomy due to gallstones and only 3 patients presented with microgallbladder (4.2%).
Cystic fibrosis-associated liver disease (CFLD) is a chronic inflammatory sclerosing cholangiopathy that is the most important non-pulmonary cause of death, accounting for a mortality rate of 2.5 to 3.3%18. It frequently manifests in patients before they reach 20 years of age and can progress to advanced liver disease, biliary cirrhosis, portal hypertension, and liver decompensation19.
Abdominal ultrasound imaging results (the presence of hepatomegaly and/or splenomegaly), together with other parameters (physical examination and laboratory tests), make up the criteria for CFLD. They were established by Debray20, and more recently, by Koh21.
With respect to CFLD, focal biliary cirrhosis (20-30%) is the resulting lesion attributable to the CFTR mutation, which in some cases can progress to multilobular biliary cirrhosis (10%), with the development of portal hypertension (PHT) (2-5%), whereas, regarding the diagnosis of hepatic steatosis (25-60%), other contributing variables must be considered, such as diabetes, obesity, and nutritional deficiencies in essential fatty acids, carnitine, and oligometals20,22.
With respect to liver ultrasound findings, in their case series on 114 patients, Tabori et al.17 found steatosis in 42/114 (37%), whereas a coarse/irregular parenchyma was detected through ultrasound in 25/114 (22%) of the cases and splenomegaly was revealed in 12/114 (11%). In their case series of 72 adult patients, Dietrich et al.14 detected irregular echo patterns in 17/72 (24%), whereas hepatic steatosis was identified in 16/72 (22%).
Regarding the hepatic ultrasound findings revealed in our case series, 11 (15.8%) patients presented with a parenchyma with a heterogeneous liver echo pattern. Six (8.5%) patients had a heterogeneous parenchyma with lobulated liver contour and splenomegaly, consistent with cirrhosis of the liver and portal hypertension23,24. Even though steatosis is described as the most common hepatic manifestation in patients with CF, with a prevalence of 25 to 60%18, in our cases, a diffuse increase in liver echogenicity caused by fat infiltration from the parenchyma was found in only 4 (5.7%) of the patients.
ConclusionAbdominal ultrasound is a safe, low-cost technique that enables the identification of some degree of chronic liver and pancreatic diseases, improving the approach and follow-up decisions made in adult patients with CF.
Unlike numerous studies conducted on children with CF, data published in Latin America referring to ultrasound findings in adults are limited, thus we believe our study on the analysis of gastrointestinal comorbidities in patients with CF provides relevant information in the context of the increasing survival of those patients.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Baran E, D’Ascenzo MV, Bosia JD, Montaña P. Hallazgos de la ecografía abdominal en pacientes adultos con fibrosis quística. Rev Gastroenterol Méx. 2022. https://doi.org/10.1016/j.rgmx.2022.05.003