Percutaneous endoscopic gastrostomy (PEG) is a popular technique, through which a flexible feeding tube is endoscopically placed in the stomach. The aim of the PEG is to maintain feeding and drug administration in patients that cannot use the oral route1–3. It is a simple procedure, with a low incidence of complications. When complications do appear, the clinical picture is usually atypical, and so adequate clinical suspicion is required for their diagnosis1–4. In addition, optimal care of the device could prevent the development of equipment-related harmful complications4.
A 74-year-old man had a history of hemophilia A. One month earlier, he sought medical attention for occipital trauma and a computed tomography (CT) scan identified a parietal/temporal fracture, with no signs of intracranial bleeding. One month later, he went to the emergency service at another center due to acute worsening of alertness. Physical examination revealed deviation of the eyes and head to the right, left homonymous hemianopsia, left-sided facial muscle paralysis, and left hemiplegia. The brain CT scan showed intraparenchymal hemorrhage in the frontal and temporal lobes, with midline shift. The patient was transferred to the intensive care unit, after undergoing right parietal decompressive craniotomy. Insertion of a PEG tube was considered necessary for feeding purposes and drug administration. After a prolonged hospital stay (2 months), the patient progressively recovered an adequate level of alertness. PEG tube removal was attempted through external traction and several attempts failed. Although endoscopic removal is the recommendation in case of failure of external traction, it was decided to section the PEG tube with scissors, and the patient was informed that it would exit the body in the passage of stool. He was discharged to his home.
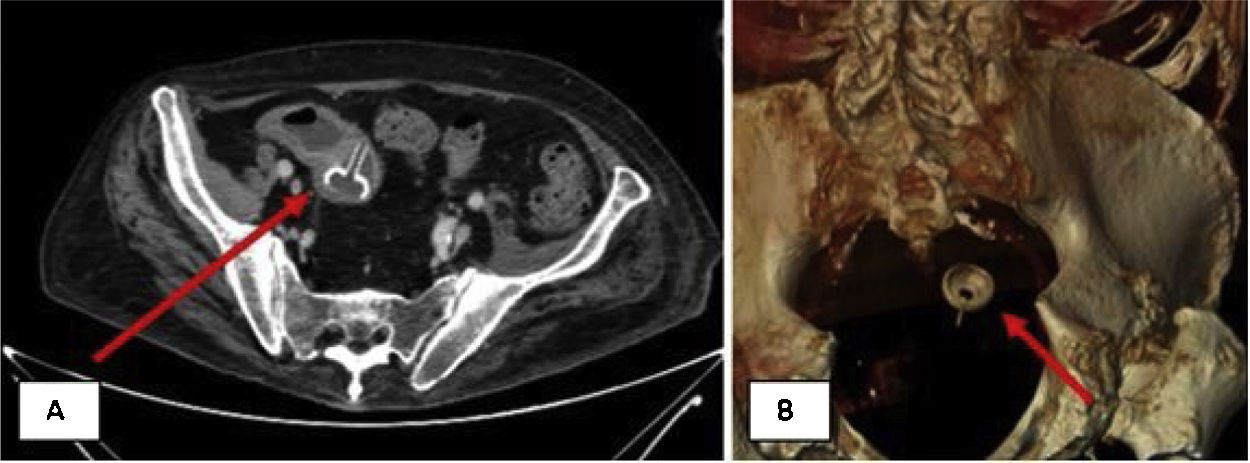
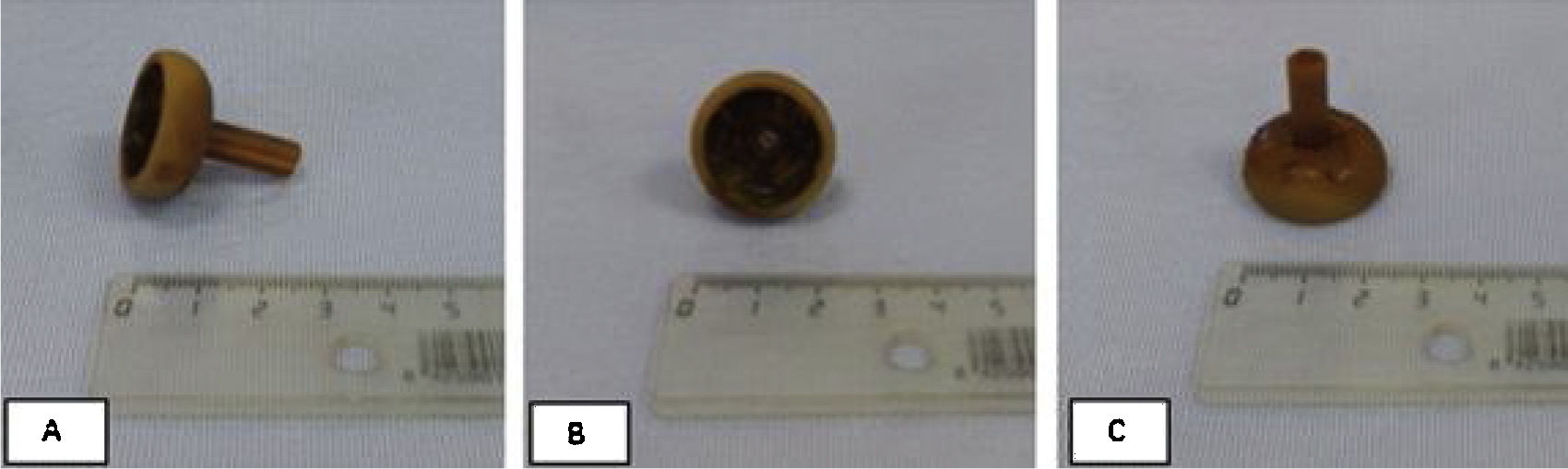
Six months later, the patient arrived at our hospital emergency department due to generalized abdominal pain, fecaloid vomiting, and fever of 3-day progression. He also described previous episodes of self-limited abdominal colicky pain, at varying locations, for the past 5 months. An abdominal CT scan revealed regional inflammation and proximal ileum ectasia due to impaction of a round foreign body, 2 cm in diameter, at the terminal ileum (Fig. 1). There were no signs of abscesses or bowel perforation. Because endoscopic removal of the PEG bumper was not feasible, the patient was transferred to the operating room and a laparotomy was performed. A foreign body, congruent with the internal bumper of a PEG, was removed from the terminal ileum (Fig. 2) through enterotomy. After recovering intestinal peristalsis and oral tolerance, the patient was discharged.
PEG is a simple, cost-effective procedure, with a low mortality rate, that ensures nutrition and drug administration. PEG is increasingly popular, especially in the management of patients after stroke2. As a consequence of its increased use, there has also been an increment in PEG-associated complications1–3. Migration of the internal bumper of the PEG is a rare complication, with few cases described in the scientific literature. Intestinal peristalsis can nudge the internal bumper, in the absence or dysfunction of the external bumper, resulting in ulcers or even perforations2,3. Clinical features are nonspecific, and patients seek medical attention at emergency services when mechanical obstruction occurs, even though abdominal pain and vomiting are symptoms that are frequently present, even months before the acute episode1–6.
Physical examination and complementary explorations between episodes can be normal, making accurate diagnostic suspicion crucial. Cases in the literature describe gastric outlet and duodenal obstruction as a complication of migrated gastrostomy tube5,6, as well as pancreatitis due to obstruction at the ampulla of Vater7. However, to the best of our knowledge, this is the first report of a case of internal bumper migration beyond the proximal ileum1. Adequate manipulation of the PEG can resolve most of those types of complications, but distal migrations are more likely to require surgical management.
Potential benefits of endoscopic control during PEG removal have been proposed4. Nevertheless, daily care and optimal manipulation appear to be the best methods for preventing complications1,3. Collecting all information about the PEG characteristics and registering the chronology of its manipulation are recommended strategies for preventing complications. Early suspicion and diagnosis can prevent distal migrations, and consequently increase the possibility of successful endoscopic management.
In conclusion, PEG has become a routine technique with potential benefits, but it is not without risks. We present herein a unique case report of distal small bowel occlusion due to migration of a PEG internal bumper. Physicians should be aware of the potential iatrogenic complications of PEG devices, to optimize the care of those patients.
Ethical considerationsInformed consent was requested from the patient to participate in the research described. The work complies with the current bioethical research regulations.
Financial disclosureNo financial support was received in relation to this article.
Author contributionsSML, AAGA, and LSR collected the data and wrote the manuscript. PDR, FGV, and FDF reviewed and approved the manuscript. All authors approved the final draft for submission. PDR is the article guarantor.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Moragón-Ledesma S, Gurjián-Arena AA, Díaz-Fontenla F, Galeano-Valle F, Demelo-Rodríguez P. Un caso inusual de obstrucción intestinal más allá de íleon proximal debido a migración interna de una gastrostomía endoscópica percutánea. Rev Gastroenterol Méx. 2022;87:122–124.