A liver mass is a focal lesion that can be differentiated from surrounding liver parenchyma through imaging techniques. The differential diagnosis is broad, ranging from benign lesions to malignant neoplasms. Past medical history provides clues to the diagnosis of a liver mass1. An incidental mass detected by imaging studies, in patients with no past medical history of liver disease, alcoholism, or cancer, is usually benign (simple cysts, hemangiomas, hepatic adenoma, and focal nodular hyperplasia)2. In patients with cancer, metastatic disease is the most frequent. A history of cirrhosis or alcohol abuse suggests hepatocellular carcinoma (HCC). Antiepileptic drugs (AEDs) are known to be associated with drug-induced liver injury and carcinogenesis, which explains the relationship between high phenytoin doses and HCC in epileptic patients3.
Hepatobiliary disorders are associated with autoimmune conditions, including celiac disease4,5. The pathophysiology is not yet clarified, but a relationship between celiac disease and hepatic malignancies has been documented6. We describe herein the case of a patient with phenytoin intake and celiac disease, presenting with a hepatic tumor located at the caudate lobe. Imaging studies were uncertain, and surgical resection was performed.
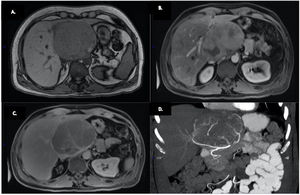
A 49-year-old man first presented with right upper quadrant abdominal pain and was admitted to the emergency department. He had a history of epilepsy treated for 20 years with phenytoin 300mg/day. An abdominal ultrasound (US) showed a 6×5×5cm isoechoic mass on the left hepatic lobe and a computed tomography (CT) scan revealed a liver hemangioma. Two years later, the patient reported having postprandial epigastric pain. A new US identified a 5cm increase of the hepatic lesion. Gadolinium-contrasted magnetic resonance imaging showed a heterogeneous 10×9×10cm hepatic mass in the caudate lobe, hypointense in the T1-weighted images and isointense in the T2-weighted images, with enhancement in the arterial phase and washout in the portal venous delayed phase (Fig. 1). An IV-contrasted CT scan showed the hepatic tumor in close relation to the right and left gastric arteries. The portal and splenic vessels were not compromised (Fig. 1). Laboratory workup was normal, except for mild hypertransaminasemia (ALT: 98 U/l, AST: 174 U/l). Tests for hepatitis B virus and hepatitis C virus were negative and alpha-fetoprotein values were normal.
A) Gadolinium-contrasted magnetic resonance imaging, showing a heterogeneous 10×9×10cm hepatic mass located at the caudate lobe, out of phase, hypointense in the T1-weighted images and isointense in the T2-weighted images. B) Arterial phase enhancement. C) Washout in the portal venous delayed phase. D) Coronal view of the CT scan. A 10cm tumor is visualized on the caudate lobe, in close relation to the right and left gastric arteries.
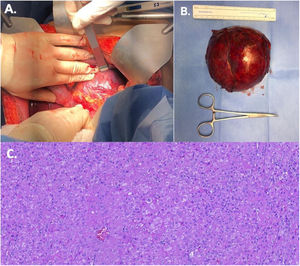
The patient was transferred to the operating room and surgical access was carried out with a bilateral subcostal incision. The hepatic tumor was situated on the caudate lobe, irrigated by the right and left gastric arteries (Fig. 2). Tumor dissection was performed, separating the celiac and portal vessels. Segmental hepatectomy of the caudate lobe was carried out (Fig. 2). The patient’s postoperative progression was satisfactory, and he was discharged 4 days after surgery.
The final histopathologic diagnosis confirmed a 10×10×11cm hepatocellular carcinoma, with 3mm margins (Fig. 2).
Seen at the outpatient clinic 3 months after surgery, the patient was asymptomatic, and his liver function tests were normal.
HCC is the most frequent type of primary liver cancer. It is the sixth most common solid tumor and the third most frequent cause of cancer-related death in the world.1,7 HCC is typically related to chronic liver disease, although 20% of the tumors may develop in noncirrhotic patients.7 Although our patient lacked the common risk factors for HCC, his use of phenytoin was chronic. Antiepileptic drugs are known to cause chronic liver injury and increase the risk for HCC, with an odds ratio (OR) of 1.2 (95% CI: 1.01–1.47). Greater risk is related to increases in the defined daily dose (DDD). An ingestion of >180 DDDs raises the OR to 14.6 (95% CI: 7.8–26.9)3. Our patient was estimated to consume an annual mean DDD of 110.
The patient had a history of celiac disease, which is associated with hepatobiliary disorders. A case report documented HCC in a patient with celiac disease, in the context of decompensated cirrhosis and hepatic venous outflow tract obstruction8. Increased intestinal permeability in celiac disease favors the entry of antigens, toxins, and cytokines into the portal circulation, which could trigger inflammation and fibrosis5.
In the present case, other causes of HCC in a noncirrhotic liver were retrospectively ruled out, such as hepatitis virus, primary sclerosing cholangitis, and hemochromatosis.
Symptom severity warranted surgical exploration and treatment, regardless of the pathologic diagnosis. No biopsy was taken.
Isolated caudate lobectomy is a challenging procedure that requires accurate knowledge of the anatomy. Incision approaches vary; in this case, a bilateral incision was made, primarily because of the size of the tumor and its anatomic relation to the lesser curvature of the stomach and left gastric artery. Tumor vasculature was successfully controlled. Previous image studies aided in the identification of the vascular structures, and no great vessel was compromised.
The final diagnosis was trabecular subtype HCC. It is the most common histologic subtype in both cirrhotic and noncirrhotic livers, and accounts for 41–76% of cases. In contrast, the fibrolamellar subtype occurs almost exclusively in noncirrhotic patients, as 5% of all HCC cases, and is detected most often in young adults with no chronic liver injury9.
Survival of noncirrhotic patients with HCC mainly depends on tumor-related factors, such as size, tumor capsule, vascular invasion, grading, R0 resection, and intraoperative blood transfusions10. Our patient had an R0 resection, with no vascular invasion. Nevertheless, tumor size was > 5cm, which conditions poor prognosis. One year after surgery, the patient has no signs of recurrence.
Ethical considerationsThe present research involved no experiments on humans or animals and was approved by the ethics committee of the School of Medicine of the Tecnológico de Monterrey and complies with current regulations in bioethical investigation.
A written statement of informed consent was obtained from the patient for treatment and publication of this work, regarding any personal information or images that could identify him.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Riojas-Garza A, González-Urquijo M, Escareño-Pérez CE, Vázquez-Ávila I, Bosques-Padilla FJ. Carcinoma hepatocelular de lóbulo caudado en un paciente no cirrótico con historia de administración de fenitoína crónica y enfermedad celíaca tratada con resección aislada de lóbulo caudado. Un reporte de caso. Rev Gastroenterol Méx. 2022;87:256–258.