Timely detection and diagnosis of hepatitis C virus (HCV) involves identifying the population that is predisposed to treatment and prevention, thus limiting complications and preventing infection. The aim of this study was to analyze and describe risk factors associated with anti-HCV antibody detection in a population with access to public healthcare that participated in a national screening program.
Material and methodsAn analytic cross-sectional study was conducted that utilized data related to rapid tests carried out between September 2021 and October 2022 in 26 of the 32 states of Mexico. Anti-HCV reactive tests were selected, according to age and sex, for analyzing and comparing possible risk factors through descriptive and inferential statistics. The geographic distribution and density of the screening program at the state and municipal levels was analyzed.
ResultsThere were 75,185 anti-HCV antibody detections, 2,052 reactive tests, and mean participant age was 44.3 years (±15.1). Occupation: 32.3% were employees, 19% were housewives, and 18.2% were healthcare workers. Five out of every 10 cases had no indication of risk factors, but there was a 1.4 and 5-times greater likelihood of anti-HCV detection in men with a history of sharps injury or intravenous psychoactive substance use, compared with women. Regarding place of residence, 80% of the reactive tests were concentrated in the State of Mexico, Mexico City, and Guanajuato.
ConclusionsThe evidence herein helps determine the population and risk factors that should be focused on in carrying out the HCV microelimination strategy of continuous screening, diagnosis, medical treatment access, and epidemiologic surveillance.
La detección y el diagnóstico oportuno del virus de la hepatitis C (VHC) implica identificar la población susceptible de tratamiento, prevenir, limitar complicaciones y evitar contagios. El objetivo de este estudio fue analizar y describir los factores de riesgo asociados a la detección de anticuerpos contra el VHC (anti-VHC) en la población con acceso a la seguridad social que participó en programa nacional de tamizaje.
Material y métodosEstudio transversal/analítico que utilizó datos relacionados con pruebas rápidas realizadas entre septiembre de 2021 y octubre de 2022 en 26 de las 32 entidades federativas de México. Se seleccionaron los reactivos anti-VHC para analizar y comparar, según sexo y edad, los posibles factores de riesgo mediante estadística descriptiva e inferencial. Se analizó la distribución y la densidad geográfica del programa de tamizaje a nivel de la entidad federativa y del municipio.
ResultadosSe realizaron 75,185 detecciones anti-VHC; 2,052 reactivos (2.7%), promedio 44.3 años (±15.1). Ocupación: 32.3% empleado, 19% ama de casa y 18.2% trabajador de sector salud. Hasta 5 de cada 10 pacientes no indicaron factores de riesgo, pero en comparación con las mujeres, los varones con antecedente de accidente con material punzocortante o uso de sustancias psicoactivas intravenosas mostraron 1.4 y 5 veces más probabilidad de detección anti-VHC. Según el lugar de residencia, el 80% de los reactivos se concentró en Estado de México, CDMX y Guanajuato.
ConclusionesLa evidencia sugiere cuál es la población y los factores de riesgo en los que se debe focalizar la estrategia de microeliminación del VHC, mediante el continuo tamizaje, diagnóstico, acceso a tratamiento médico y seguimiento epidemiológico.
Hepatitis C virus (HCV) infection continues to be a public health problem, in both high-income and low-income countries due to the spectrum of health, social, and economic consequences attributable to the disease.1,2 According to a recent report, the incidence rate in Mexico during 2020 was 0.28%,3 whereas prevalence was 1.4%.4 The difference in those two figures could be explained by infection routes and/or different risk factors that have been reported in the Mexican population. In this sense, exposure to contaminated blood has been the main mechanism of infection reported in different scientific articles2,5 (exposure when sharing needles for the intravenous injection of psychoactive substances, accidents caused by sharp instruments [sharps injury] in healthcare workers, and transfusions). However, sex-related mechanisms (multiple partners or high-risk intercourse) and intrauterine mechanisms (mother to child) have also been identified.6
Hepatitis C caused by HCV is recognized as an inflammation of the liver. It can manifest as acute infection that tends to be asymptomatic, but progress to chronic disease that can present with complications.7 Thus, approximately 30% of diagnosed persons spontaneously eliminate the virus in the 6 months following infection and do not need treatment,2 whereas the disease tends to progress to chronicity in 70%.6,8 Because the clinical symptoms of HCV are unspecific, up to 8 of every 10 persons are unaware of having the disease,1 and as a result, do not receive timely treatment. Possible consequences of the disease are cirrhosis, hepatocellular carcinoma, or liver failure.6
Regarding HCV, population groups with a higher risk for infection have been recognized; for example, migrating populations from countries with intermediate and high endemicity, certain indigenous groups, intravenous or intranasal psychoactive substance users, persons with a history of transfusions before 1995 or a history of incarceration, men that have sex with men, male and female sex workers, persons with human immunodeficiency virus (HIV), and children of mothers with chronic hepatitis B or C infection, especially if they are diagnosed with HIV.9
Therefore, screening programs are a useful strategy in terms of public health, not only for detecting disease and identifying the population that requires a clinical diagnosis, but also for defining the susceptible population for receiving medical treatment, thus limiting infection chains and gradually eliminating HCV infection. This is in line with the strategy of the World Health Organization (WHO) for the 5 hepatitis viruses (A, B, C, D, and E).10 Screening implies reducing both incidence and mortality rates, which is also feasible, thanks to the availability of new medical treatments.11 In this sense, the WHO recommends screening mainly in populations with risk factors and/or behaviors associated with this disease,2,3,12 to increase the number of opportune clinical diagnoses.13 Therefore, the aim of this study was to analyze and describe the risk factors associated with anti-HCV antibody detection in a population with access to public healthcare that participated in a national program carried out from September 2021 to October 2022 in Mexico.
Material and methodsAn analytic cross-sectional study was conducted, utilizing the STROBE checklist for observational studies. The study included data obtained through a health information system related to an institutional HCV microelimination strategy. Said strategy has been implemented since September 2021 by primary and secondary care hospitals that belong to the Instituto Mexicano del Seguro Social (IMSS), a national public healthcare system, distributed in the 32 Mexican states. The population with access to the IMSS (insured population and workers) has voluntarily participated in the strategy. In brief, one of the essential components of the institutional HCV microelimination strategy is screening. It involves the use of a questionnaire (Table 1) with dichotomous questions directed at identifying risk factors and high-risk behaviors. The participants, after giving their informed consent, undergo anti-HCV antibody detection tests, through Advanced Quality™ (InTec Products, Inc., Fujian, China), which has a reported specificity and sensitivity of 97-99% and 100%, respectively. Persons with reactive tests then undergo confirmatory testing and the corresponding diagnosis is made. Access to the necessary medical treatment is guaranteed and the corresponding surveillance and epidemiologic follow-up is carried out, until the HCV is eliminated, and the persons are cured.
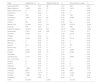
Absolute and relative risk factors reported by the population with access to public healthcare that participated in the institutional anti-HCV antibody screening program, 2021-2022.
| No | Yes | |
|---|---|---|
| n (%) | n (%) | |
| 1 Do you share or have you shared razor blades, razors, or toothbrushes? | 1,619 (78.9%) | 433 (21.1%) |
| 2 Do you have or have you had tattoos, piercings, permanent eyeliner tattooing or microblading? | 1,166 (56.8%) | 886 (43.2%) |
| 3 Do you use or have you used intravenous psychoactive substances (drugs) even if only once? | 1,953 (95.2%) | 99 (4.8%) |
| 4 Do you use or have you used intranasal psychoactive substances (drugs)? | 1,924 (93.8%) | 128 (6.2%) |
| 5 Did you receive a blood or blood product (plasma, platelets) transfusion before 1995? | 1,796 (87.5%) | 256 (12.5%) |
| 6 Did you receive any type of transplant before 1995? | 2,034 (99.1%) | 18 (0.9%) |
| 7 Do you have HIV infection? | 1,923 (93.7%) | 129 (6.3%) |
| 8 At the time of your birth, did your mother have or was diagnosed with hepatitis C? | 2,015 (98.2%) | 37 (1.8%) |
| 9 Do you engage in or have you engaged in high-risk sexual practices (multiple sexual partners)? | 1,575 (76.8%) | 477 (23.2%) |
| 10 Do you engage in or have you engaged in unsafe sexual intercourse? | 705 (34.4%) | 1,347 (65.6%) |
| 11 Do you have or have you had a sexual partner with hepatitis C virus infection? | 1,983 (96.6%) | 69 (3.4%) |
| 12 Do you have or have you had a sexually transmitted disease? | 1,887 (92%) | 165 (8%) |
| 13 Do you use or have you used psychoactive substances for sexual purposes (chemsex)? | 2,020 (98.4%) | 32 (1.6%) |
| 14 Have you been in prison? | 2,005 (97.7%) | 47 (2.3%) |
| 15 Do you receive or have you received hemodialysis? | 2,024 (98.6%) | 28 (1.4%) |
| 16 Have you had a sharps injury?a | 280 (13.6%) | 337 (16.4%) |
| 17 Have you had mucosal exposure to or injury or lesions from sharps used by persons infected with hepatitis C?a | 524 (25.5%) | 85 (4.1%) |
| 18 Are you in contact with medical equipment, such as catheters and endoscopes?a | 395 (19.2%) | 214 (10.4%) |
HCV: hepatitis C virus; HIV: human immunodeficiency virus.
With respect to the secondary source, 75,185 detections were made at the national level, during the September 2021/October 2022 time period. For the present study, only the participants whose anti-HCV antibody reactive tests were reported in that same time period, and whose data were complete and available for analysis, were selected. In addition, the characteristics of sex, age, occupation, and place of residence were collected, together with the following dichotomous variables, reported as risk factors in other publications3,7,10,14: shared razor blade, razor, or toothbrush use; a history of tattoos, piercings, and eyeliner tattoos and microblading; intravenous or intranasal psychoactive substance (drug) use; a history of blood or blood product transfusion or transplantation before 1995; HIV diagnosis; birth to an HCV-infected mother, multiple sexual partners; regular engagement in unsafe sexual intercourse; a sexual partner with HCV; a history of sexually transmitted disease; engagement in psychoactive substance use for sexual purposes (chemsex); a history of incarceration; a history of hemodialysis; sharps injury; mucous membrane exposure to or injury from sharps used by persons with HCV; and contact with medical equipment, such as catheters and endoscopes.
Statistical and geographic analysisThe variables were analyzed using descriptive and inferential statistics, depending on their nature. The results of the frequency analysis of the occupation variable are shown in a word cloud, whereas participant age was obtained through summary measures (mean, standard deviation, median, and minimum and maximum values). Absolute and relative frequencies were calculated for the dichotomous variables.
As a complement, a bivariate analysis was performed to identify the variables associated with anti-HCV antibody detection, which were considered in the final model through logistic regression, adjusted by sex and age according to the risk factors, resulting in the association measurements of odds ratio (OR) and coefficients (B0, B1), and the consequent statistically significant variables (p < 0.05). The models were created using the Windows SPSS® version 27 program.
A process of geolocation was carried out, based on place of residence of the participants with reactive tests in the screening program, preserving anonymity and confidentiality, to create a map for visualizing distribution and spatial density of the anti-HCV antibody detections at the state and municipal level.
Ethical considerationsThis study follows the current health and bioethical research regulations established by the General Health Law15 and the respective Health Research Regulation.16 The study was classified as a non-risk analysis because it involved no experiments on animals or humans. Data were obtained from a secondary source, maintaining anonymity and confidentiality, and did not nominally identify any patient. Given the above, informed consent from the patients was not required.
ResultsA total of 2,052 anti-HCV antibody reactive tests (2.7%) were analyzed and 67.3% (n = 1,381) of the population that participated in the screening tests were women. Mean patient age was 44.3 years (± 15.1), with a median of 42 and a range of 15 to 95. Regarding occupation, employee was the most frequent category (n = 664, 32.3%), followed by housewife (n = 389, 19%), and healthcare professional (n = 374, 18.2%) (with medicine, nursing, and social work as the main professions reported) (Fig. 1).
Occupational frequency analysis reported by the population with public healthcare access that participated in an institutional anti-HCV antibody detection program, 2021-2022. The word cloud presents the results of the frequency analysis according to occupation that was reported by the population with access to public healthcare (general population and health institution workers), who participated in the institutional screening program for anti-HCV antibodies, corresponding to September 2021 and October 2022.
Source: prepared by the authors based on institutional registries of detections of anti-HCV antibodies in the population with access to public healthcare, 2021 and 2022.
Table 1 shows the absolute and relative frequencies of the factors analyzed in the population that participated in the screening. Even though the majority had a negative result, a small percentage reported risk factors, such as tattoos, piercings, eyeliner tattoos, or microblading (43.2%), multiple sexual partners (23.2%) and shared razor blade, razor, and toothbrush use (21.2%), among others.
Table 2 describes the risk factors calculated through logistic regression models adjusted for sociodemographic characteristics. Even when age was not statistically significant, compared with women, men showed a 3 to 28-times higher probability (p < 0.0001) of presenting with the following risk factors: birth to an HCV-infected mother; a history of hemodialysis; a history of blood or blood product transfusion before 1995; a history of incarceration; intranasal psychoactive substance use or chemsex; and unsafe sexual intercourse. The probability of anti-HCV antibody detection regarding sharps injury and intravenous psychoactive substance use in men, was 1.4-times and 5-times higher, respectively, than in women (Table 2).
Risk factors of the population with access to public healthcare that participated in the institutional anti-HCV antibody screening program, 2021-2022, adjusted by sociodemographic characteristics.
| Sexa | Age | Constant | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Beta (0) | ORb | P | Beta (0) | ORb | P | Beta (0) | ORb | P | |
| 1 Do you share or have you shared razor blades, razors, or toothbrushes? | – | – | – | – | – | – | – | – | – |
| 2 Do you have or have you had tattoos, piercings, permanent eyeliner tattooing or microblading? | – | – | – | – | – | – | – | – | – |
| 3 Do you use or have you used intravenous psychoactive substances (drugs) even if only once? | −0.28 | 0.76 | p = 0.006* | −0.04 | 0.96 | p < 0.0001* | 1.62 | 5.06 | p < 0.0001* |
| 4 Do you use or have you used intranasal psychoactive substances (drugs)? | 1.69 | 5.43 | p < 0.0001* | 0.00 | 1.00 | p = 0.922 | −3.81 | 0.02 | p < 0.0001* |
| 5 Did you receive a blood or blood product (plasma, platelets) transfusion before 1995? | 2.36 | 10.58 | p < 0.0001* | −0.01 | 0.99 | p = 0.046* | −3.48 | 0.03 | p < 0.0001* |
| 6 Did you receive any kind of transplant before 1995? | −0.40 | 0.67 | p = 0.012* | 0.07 | 1.07 | p < 0.0001* | −5.13 | 0.01 | p < 0.0001* |
| 7 Do you have HIV infection? | – | – | – | – | – | – | – | – | – |
| 8 At the time of your birth, did your mother have or was diagnosed with hepatitis C? | 3.36 | 28.73 | p < 0.0001* | −0.04 | 0.96 | p < 0.0001* | −3.34 | 0.41 | p < 0.0001* |
| 9 Do you engage in or have you engaged in high-risk sexual practices (multiple sexual partners)? | – | – | – | – | – | – | – | – | – |
| 10 Do you engage in or have you engaged in unsafe sexual intercourse? | 1.10 | 3.02 | p < 0.0001* | 0.00 | 1.00 | p = 0.910 | −1.64 | 0.19 | p < 0.0001* |
| 11 Do you have or have you had a sexual parter with hepatitis C virus infection? | – | – | – | – | – | – | – | – | – |
| 12 Do you have or have you had a sexually transmitted disease? | – | – | – | – | – | – | – | – | – |
| 13 Do you use or have you used psychoactive substances for sexual purposes (chemsex)? | 1.12 | 3.06 | p < 0.0001* | -0.03 | 0.97 | p < 0.0001* | −1.62 | 0.20 | p < 0.0001* |
| 14 Have you been in prison? | 2.25 | 9.48 | p < 0.0001* | -0.02 | 0.98 | p = 0.061 | −4.43 | 0.01 | p < 0.0001* |
| 15 Do you receive or have you received hemodialysis? | 2.51 | 12.25 | p < 0.0001* | 0.04 | 1.04 | p < 0.0001* | −6.99 | 0.00 | p < 0.0001* |
| 16 Have you had a sharps injury? | −0.52 | 0.59 | p < 0.0001* | −0.03 | 0.98 | p < 0.0001* | 0.37 | 1.45 | p = 0.018* |
| Have you had mucosal exposure to or injury or lesion from sharps used by a person with hepatitis C? | – | – | – | – | – | – | – | – | – |
| Are you in contact with medical equipment, such as catheters and endoscopes? | – | – | – | – | – | – | – | – | – |
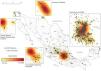
Fig. 2 shows the location and distribution of the anti-HCV antibody reactive tests reported in the institutional screening program, according to place of residence. The states with the highest number of reactive tests were Estado de México (45.4%, n = 931), Mexico City (26%, n = 531), and Guanajuato (12.1%, n = 249), whereas at the municipal level, the greatest spatial density of the reactive tests was found in Ecatepec de Morelos (Estado de México), Gustavo A. Madero (Mexico City), León (Guanajuato), Nezahualcóyotl (Estado de México), and Chalco (Estado de México). According to the number of detections (Table 3), the highest values were registered in the following states, in descending order: Mexico City (32.5%, n = 24,444), Estado de México (16.6%, n = 12,475), Veracruz (12.2%, n = 9,138), Chihuahua (5.4%, n = 4,081), and Baja California (4.9%, n = 3,686). However, there was no statistical relation between the number of detections and reactive tests reported, according to state (data not presented).
Shows the distribution and spatial density of anti-HCV detections according to the place of residence reported by the population with access to public healthcare (general population and health institution workers), who participated in the institutional screening program, corresponding to September 2021 and October 2022. Thus, the greater intensity of the shaded areas represents a greater concentration of reactive detections, suggesting the municipalities and states where the incidence rates could be higher, compared with other places in Mexico.
Source: prepared by the authors based on institutional registries of anti-HCV antibody detection in the population with access to public healthcare, 2021 and 2022.
Absolute and relative frequencies of anti-HCV antibody detections in a population with access to public healthcare that participated in the institutional screening program, 2021-2022.
| State | Detections (n) | % | Reactive tests (n) | % | Nonreactive (n) tests | % |
|---|---|---|---|---|---|---|
| Aguascalientes | 580 | 0.77 | 48 | 2.34 | 534 | 0.73 |
| Baja California | 3,686 | 4.90 | 72 | 3.51 | 3,618 | 4.95 |
| Baja California Sur | 11 | 0.01 | 0 | 0.00 | 11 | 0.02 |
| Campeche | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| Chiapas | 755 | 1.00 | 8 | 0.39 | 749 | 1.02 |
| Chihuahua | 4,081 | 5.43 | 95 | 4.64 | 3,986 | 5.45 |
| Coahuila | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| Colima | 291 | 0.39 | 0 | 0.00 | 291 | 0.40 |
| Mexico City | 24,444 | 32.51 | 531 | 25.88 | 23,879 | 32.65 |
| Durango | 257 | 0.34 | 2 | 0.10 | 255 | 0.35 |
| Estado de México | 12,475 | 16.59 | 931 | 45.37 | 11,590 | 15.85 |
| Guanajuato | 2,301 | 3.06 | 249 | 12.13 | 2,024 | 2.77 |
| Guerrero | 2,383 | 3.17 | 9 | 0.44 | 2,376 | 3.25 |
| Hidalgo | 1 | 0.00 | 0 | 0.00 | 1 | 0.00 |
| Jalisco | 2,539 | 3.38 | 30 | 1.46 | 2,512 | 3.44 |
| Michoacán | 2 | 0.00 | 0 | 0.00 | 2 | 0.00 |
| Morelos | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| Nayarit | 574 | 0.76 | 3 | 0.15 | 571 | 0.78 |
| Nuevo León | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| Oaxaca | 2,573 | 3.42 | 15 | 0.73 | 2,560 | 3.50 |
| Puebla | 2,408 | 3.20 | 19 | 0.91 | 2,389 | 3.27 |
| Querétaro | 1 | 0.00 | 0 | 0.00 | 1 | 0.00 |
| Quintana Roo | 2,701 | 3.59 | 21 | 1.02 | 2,680 | 3.66 |
| San Luis Potosí | 1 | 0.00 | 0 | 0.00 | 1 | 0.00 |
| Sinaloa | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| Sonora | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| Tabasco | 2 | 0.00 | 0 | 0.00 | 2 | 0.00 |
| Tamaulipas | 1,658 | 2.21 | 8 | 0.39 | 1,651 | 2.26 |
| Tlaxcala | 829 | 1.10 | 0 | 0.00 | 829 | 1.13 |
| Veracruz | 9,138 | 12.15 | 9 | 0.44 | 9,130 | 12.48 |
| Yucatán | 1,492 | 1.98 | 2 | 0.10 | 1,490 | 2.04 |
| Zacatecas | 2 | 0.00 | 0 | 0.00 | 2 | 0.00 |
| Total | 75,185 | 2,052 | 73,133 |
Anti-HCV antibodies were detected mainly in participants < 45 years of age and in women. Even though 50% of the population that participated in the screening program had no risk factors, sharps injury and intravenous psychoactive substance use increased the probability of anti-HCV antibody detection in men, compared with women, regardless of occupation. Considering that the population included in the institutional screening program has access to public healthcare, the recommendation is that the IMSS ensure the continuum of screening, diagnosis, medical treatment access, and epidemiologic follow-up, through the available material, human, and medical unit resources, to feasibly eliminate HCV infection and contribute to reducing the morbidity burden it has in Mexico.
Regarding its seroprevalence in the Mexican population, a recent study conducted in Western Mexico reported a value of 3.9%,12 which is a higher figure, compared with those in high-income countries, such as the United States (2.1%)6 or Poland (0.9-1.9%).17 The National Health and Nutrition Survey (ENSANUT, the Spanish acronym) reported a higher prevalence in men than in women, at 0.49% (95% CI 0.24-0.59) and 0.29% (95% CI 0.14-0.63), respectively.11,18 Other studies have not identified significant differences between sexes but an even higher seroprevalence of up to 6% has been reported.1 Particularly in healthcare workers, seroprevalence reported in Mexico has ranged from 0.5 to 1.3%.19 However, the differences between the cited values could be explained by the fact that the majority of studies have included populations tied to hospitals and have not been representative,11 with the exception of the seroprevalence reported by the ENSANUT.18 Seroprevalence differences could also be attributable to the anti-HCV antibody detection test utilized, the type of population participating in the screening programs (open population, institutional health care sector workers, blood and blood product donors), differences in access to healthcare service, and availability of medical treatment,17 as well as the risk for infection attributable to certain specific population groups, which should be a priority in HCV elimination strategies, taking into account known risk factors.
Evidence has shown a greater consensus on HCV risk factors in the general population, such as a history of hemodialysis, having received a blood transfusion before HCV screening, drug use, intranasal or intravenous psychoactive substance use, and sexual factors.3,6,7 In addition, other studies on healthcare workers have reported sharps injury (66.7%) and medical or odontology-related injury (58.6%) as risk factors.4,5,19 In our study, which included a public healthcare sector with access to insurance, a history of sharps injury and intravenous psychoactive substance use was found to increase the probability of anti-HCV antibody detection, with a higher frequency in participants < 45 years of age. In addition to the fact that the factors identified in our study coincide with those reported in other publications, they are also preventable and can be modified. Thus, our results underline the need to reinforce the dissemination of information on how to prevent HCV infection attributable to widely recognized risky practices, such as the use of tattoos and piercings, intravenous drugs, and certain cosmetic procedures.3,17 They also highlight the need to reinforce safety norms and protective measures for both healthcare workers and the general population, particularly regarding invasive medical interventions, injections, and blood product administration,10 in order to prevent sharps injuries involving infectious biologic material and reduce occupational hazards,5 because HCV is one of the most common occupational infections,10,20 as well as one of the main causes of chronic liver disease.6,10,17 In addition, these results contribute to strengthening the available evidence on determining which population screening programs should be directed at, given that the probability of detection is higher, according to place of residence, sex, age, occupation, and risk factors.17 Thus, it is possible to adapt and focus actions of detection, diagnostic confirmation, case monitoring, and epidemiologic follow-up, in order to increase the program’s positive impact on HCV elimination.
From a geographic perspective, a higher incidence of HCV was reported in previous years in states characterized by high population density and constant migratory flows, such as occurs in the northern (Baja California), western (Sinaloa, Jalisco), and central (Estado de México and Mexico City) areas of Mexico,3 compared with the southern zone.6 Our results show an even higher rate of anti-HCV antibody detection in those same areas, suggesting that HCV infection has increased in recent years. With respect to the institutional HCV microelimination strategy conducted by the IMSS, it is possible that the number of reactive tests increases in direct relation to the increase in the number of detections, particularly in Mexico City, Chihuahua, and Baja California. Therefore, we consider that this evidence can be used in the planning and implementation of this program because it identifies the states that could have a higher prevalence of HCV at the national level, enabling a prioritized focus on screening strategies, when they are necessary, and the performance of monitoring and epidemiologic follow-up. Extending the coverage of the institutional microelimination strategy in the northern (Coahuila, Nuevo León, Sinaloa, Sonora) and southeastern (Campeche) states of Mexico, where we found a lower number of detections (Table 3), is also a relevant suggestion.
Certain limitations of the present study need to be considered. Even though the anti-HCV antibody screening strategy was implemented nationally, it only covered 26 states (81.2%), signifying that its results are not representative. Moreover, at the northern border of Mexico (Tijuana, Baja California) and the western (León, Guanajuato) and central (Estado de México and Mexico City) areas, there was a higher number of anti-HCV reactive tests, but these are states that also have more material, human, and health infrastructure resources, compared with others, signifying that anti-HCV antibody detection could be over-represented. In addition, the spectrum of risk factors analyzed was limited and ruling out the causal association with other infection factors in the cases that were detected through the institutional strategy was not possible. Nevertheless, 100% of the persons with reactive tests underwent a reverse transcription polymerase chain reaction (RT-PCR) confirmatory test. The fact that the results come from an institutional HCV microelimination strategy, implemented at the Mexican public healthcare institution that has over 54 million beneficiaries should also be underlined. Therefore, not only does our study provide useful information for the IMSS, it also complements public health strategies implemented by the National Health System in Mexico, such as the Health Department’s National Hepatitis C Elimination Program, which includes screening, diagnostic testing, and when necessary, medical treatment.21 Thus, the evidence provided by our study highlights where territorial coverage should be extended in order to increase the HCV detection possibilities at the national level, as well as suggests the places (municipal and state) that could currently register a greater HCV burden, establishing where the continuation of screening programs is required, and in turn, guaranteeing medication for reactive and confirmed cases.
In conclusion, the present study suggests that having up-to-date knowledge of the risk factors and high-risk behavior of populations is important for reinforcing and disseminating relevant preventive measures, regarding HCV infection in the general population. The HCV microelimination program of the IMSS identified the at-risk population groups and their characteristics (sex, age, occupation), previously described in the literature, that should be prioritized, in line with established national21 and international10 strategic goals. This was done through the implementation of questionnaires for identifying risk factors, screening, diagnostic confirmation tests, access to medical treatment, monitoring, and epidemiologic follow-up, making the control and eventual elimination of HCV a feasible endeavor in the population insured by the IMSS.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study, signifying there was no need to use any type of financial plan.
Conflict of interestThe authors declare they have no personal or financial relation with other persons or organizations that could give rise to a conflict of interest related to this article.
The authors wish to thank the volunteers that participated in the screening programs, providing the data needed for the analysis presented in this manuscript, which in turn, should improve the impact of the Mexican National Program for the Elimination of Hepatitis C.