Double-balloon enteroscopy is a recently introduced endoscopic method that enables complete visualization of the small bowel, as well as biopsy sampling and therapeutic interventions in that part of the intestine. The aim of the present study was to describe the experience acquired at our hospital to determine the characteristics of the patients that underwent the procedure.
Materials and methodsA descriptive, cross-sectional study was conducted on all patients above 18 years of age admitted to the Hospital Universitario de la Fundación Santa Fe de Bogotá for double-balloon enteroscopy, within the time frame of January 2013 to December 2017.
ResultsThe study sample included 93 procedures in 73 patients. Mean patient age was 57.91 years, with a similar number of men and women. There were no severe complications. The most frequent indication for the enteroscopy was gastrointestinal bleeding (overt or occult), presenting in 49.46% of the patients, followed by chronic diarrhea (16.13%). Video capsule endoscopy was the previous study most frequently performed (53.76%). Anterograde double-balloon enteroscopy was carried out in 49 patients and 44 patients underwent the retrograde procedure. A total of 86.02% of the enteroscopies were diagnostic procedures and 13.98% were therapeutic. Normal enteroscopy was the most frequent finding (59.68%), followed by the presence of ulcers (15.05%).
ConclusionsOur results were similar to those reported worldwide, with respect to indications, insertion route, and insertion depth, and there were no severe complications.
La enteroscopia de doble balón es un método endoscópico recientemente introducido que permite la completa visualización, toma de biopsias e instauración de medidas terapéuticas del intestino delgado. Mediante este estudio, se busca describir la experiencia adquirida en nuestra institución con el fin de determinar las características de los pacientes que fueron llevados a esta intervención.
Materiales y métodosSe realizó un estudio descriptivo de corte transversal donde se incluyeron todos los pacientes mayores de 18 años que ingresaron al Hospital Universitario de la Fundación Santa Fe de Bogotá para la realización de enteroscopia de doble balón desde el 01 de enero de 2013 hasta el 31 de diciembre de 2017.
ResultadosLa muestra recolectada fue de 93 procedimientos en 73 pacientes, la media de edad fue de 57.91 años, la proporción de varones y mujeres fue muy similar, y no se presentaron complicaciones graves. Con respecto a la indicación para la realización de la enteroscopia, la más frecuente fue el sangrado digestivo (manifiesto y oculto) en el 49.46% seguida por la diarrea crónica en el 16.13%. La videocápsula endoscópica fue el estudio previo más frecuente (53.76%). Cuarenta y nueve procedimientos fueron realizados por vía anterógrada y 44 fueron realizados por vía retrógrada. El 86.02% de las enteroscopias fueron realizadas con fines diagnósticos y el 13.98% con fines terapéuticos. La enteroscopia normal fue el hallazgo más frecuente (59.68%), seguido por la presencia de úlceras (15.05%).
ConclusionesNuestros resultados son similares a los mundiales con respecto a las indicaciones, vía de inserción y profundidad, sin presentarse complicaciones graves.
Double-balloon enteroscopy (DBE) is a recently introduced endoscopic method that enables complete visualization of the small bowel, as well as biopsy sampling and therapeutic interventions in that part of the intestine.1,2
It is a relatively simple technique that has been implemented at the Hospital Universitario de la Fundación Santa Fe de Bogotá as a diagnostic and therapeutic method used in cases of small bowel pathology since January of 2013.
The primary aim of the present study was to describe the experience with double-balloon enteroscopy at the Hospital Universitario de la Fundación Santa Fe de Bogotá within the time frame of January 2013 to December 2017.
The specific aims were to characterize the adult patient population that underwent the procedure, describe the endoscopic indications and findings, describe the characteristics of the enteroscopy procedure, and to determine the diagnostic and therapeutic efficacy, as well as the complications, of the procedures performed.
Materials and methodsA descriptive, cross-sectional study was conducted that included all the adult patients admitted to the Hospital Universitario de la Fundación Santa Fe de Bogotá to undergo DBE, within the time frame of January 1, 2013 to December 31, 2017.
Selection criteriaInclusion criteria: above 18 years of age; programmed to undergo DBE, regardless of the access route; procedure performed within the time frame of the study.
Exclusion criteria: missing data in relation to indications for and characteristics of the procedure.
Data analysis planThe data were collected, registered, and then verified to correspond to the type of variable, its corresponding unit, the conceptual definition, the proper indicator, and the codification, if applicable.
With respect to the population characterization variables, the distribution of the categorical or qualitative variables was determined through relative frequencies, and percentages and mean, median, mode, and standard deviation were obtained for the continuous or quantitative variables as measures of central tendency and dispersion. The STATA® v. 11 software was utilized for the data analysis.
Ethical considerationsThe protocol was approved by the Subdepartment of Clinical Studies and Clinical Epidemiology of the Department of Medicine and by the Corporative Committee of Research Ethics of the Fundación Santa Fe de Bogotá.
ResultsInitial patient characteristicsThe study sample included 93 procedures in 73 patients that underwent DBE at the Hospital Universitario de la Fundación Santa Fe de Bogotá within the time frame of January 1, 2013 to December 31, 2017. The mean age of the patients was 57.91 years, with a standard deviation of 16.3 years. The percentage of men was 45.16% (43 patients) and the percentage of women was 54.84% (51 patients).
The most frequent indication for enteroscopy was gastrointestinal bleeding (overt or occult) in 49.46% of the patients (n=46), followed by chronic diarrhea in 16.13% (n=15). Other less frequent indications were suspected neuroendocrine tumor (11.83%), small bowel lesion (5.38%), and bowel obstruction (5.38%) (Table 1).
Initial patient characteristics.
| Characteristic (n=93) | |
| Age in years, mean (SD) | 57.91 (16.30) |
| Women, number (%) | 51 (54.84) |
| Indication for enteroscopy | |
| Overt bleeding, number (%) | 33 (35.48) |
| Chronic diarrhea, number (%) | 15 (16.13) |
| Occult bleeding, number (%) | 13 (13.98) |
| Neuroendocrine tumor, number (%) | 11 (11.83) |
| Dolor abdominal, number (%) | 6 (6.45) |
| Small bowel lesion, number (%) | 5 (5.38) |
| Bowel obstruction, number (%) | 5 (5.38) |
| Crohn's disease, number (%) | 2 (2.15) |
| Familial polyposis, number (%) | 2 (2.15) |
| Anastomosis stricture, number (%) | 1 (1.08) |
| Study performed prior to the procedure | |
| Video capsule, number (%) | 50 (53.76) |
| Abdominal tomography, number (%) | 28 (30.11) |
| CT enterography, number (%) | 7 (7.53) |
| PET scan, number (%) | 2 (2.15) |
| Abdominal magnetic resonance, number (%) | 1 (1.08) |
| Bowel transit, number (%) | 1 (1.08) |
| Video capsule findings* | |
| Ulcers, number (%) | 23 (46) |
| Small bowel lesion, number (%) | 6 (12) |
| Polyps, number (%) | 5 (10) |
| Angioectasias, number (%) | 5 (10) |
| Bleeding, number (%) | 2 (4) |
| Duodenal atrophy, number (%) | 1 (2) |
| GIST, number (%) | 1 (2) |
| Normal, number (%) | 5 (10) |
| Undiagnosed due to poor preparation, number (%) | 2 (4) |
CT: computed tomography; GIST: gastrointestinal stromal tumor; PET: positron emission tomography, SD: standard deviation.
Video capsule endoscopy was the most frequent study performed prior to the enteroscopy (53.76%), followed by abdominal computed axial tomography (30.11%), and CT enterography (7.53%). Of the patients that underwent video capsule endoscopy, 46% presented with ulcers, 12% had evidence of small bowel lesions, and 10% presented with polyps. Video capsule endoscopy was normal in 5 patients (Table 1).
Characteristics of the enteroscopy procedureOf the 93 procedures, the access route in 49 was anterograde and it was retrograde in 44. A total of 86.02% were performed for diagnostic purposes and 13 (13.98%) were both diagnostic and therapeutic. A biopsy for pathologic study was taken in 35 of the diagnostic procedures. The mean duration of anterograde enteroscopy was 78min and was similar for the retrograde procedure. The mean length of extension in the anterograde procedure was 315cm and 157cm with the retrograde approach (Table 2). In one case, visualization of the intestine was complete, utilizing both the anterograde and retrograde routes, confirmed by viewing the tattoo. No enteroscopy was complete by way of a single access route.
Enteroscopy characteristics.
| Characteristic (n=93) | |
|---|---|
| Diagnostic procedure, number (%) | 80 (86.02) |
| Tattooing performed, number (%) | 42 (45.16) |
| Pathology samples taken, number (%) | 35 (37.63) |
| Access approach | |
| Anterograde, number (%) | 49 (52.69) |
| Retrograde, number (%) | 44 (47.31) |
| Anterograde procedure (n=49) | |
| Duration in minutes, mean (SD) | 78.08 (39.69) |
| Length in centimeters, mean (SD) | 315.92 (121.05) |
| Retrograde procedure (n=44) | |
| Duration in minutes, mean (SD) | 78.20 (43.29) |
| Length in centimeters, mean (SD) | 157.34 (98.51) |
| Endoscopic findings | |
| Normal, number (%) | 53 (56.98) |
| Ulcers, number (%) | 14 (15.05) |
| Lesion with a subepithelial tumor aspect, number (%) | 8 (8.60) |
| Angioectasias, number (%) | 5 (5.38) |
| Polyp, number (%) | 3 (3.23) |
| Bowel segment stricture, number (%) | 2 (2.15) |
| Reduced villi, number (%) | 2 (2.15) |
| Lymphatic cyst, number (%) | 1 (1.08) |
| Obstructive meconium, number (%) | 1 (1.08) |
| Complications | |
| None, number (%) | 89 (95.7) |
| Abdominal pain, number (%) | 1 (1.08) |
| Contained microperforation, number (%) | 1 (1.08) |
| Ileus with pneumatosis intestinalis, number (%) | 1 (1.08) |
| Esophageal hematoma, number (%) | 1 (1.08) |
SD: standard deviation.
Normal enteroscopy was the most frequent finding (56.98%), followed by the presence of ulcers (15.05%), evidence of a lesion with the aspect of a submucosal tumor (8.60%), and angioectasias (5.38%) (Table 2).
Upon analyzing the cases that underwent video capsule endoscopy prior to the double-balloon enteroscopy, 13 (26%) of the 50 endoscopies performed had diagnostic correlation.
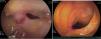
Of the 13 therapeutic enteroscopies performed, the most frequent procedure was endoscopic therapy with the submucosal infiltration of diluted adrenaline (saline solution at 0.9%/9 cc plus 1mg of adrenaline) in 38.46% of the patients, followed by argon therapy in 23.08%, and polypectomy in 3 cases (Table 3). One hundred percent of the cases in which endoscopic therapy with the submucosal infiltration of diluted adrenaline (saline solution at 0.9%/9 cc plus 1mg of adrenaline) was carried out, corresponded to ulcers, and the 3 cases in which argon therapy was performed, corresponded to angioectasias (Fig. 1). Argon was not available at the time monotherapy with adrenaline was performed. A patient with a history of bariatric surgery with symptoms of abdominal pain and bloating underwent balloon dilation, dilating the pylorus 2cm with the balloon, with no complications.
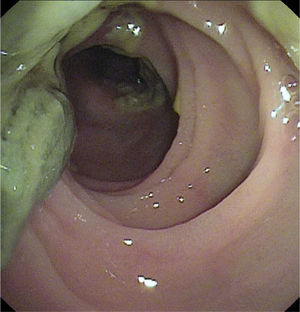
In a post-lung transplantation patient, enteroscopy was carried out to resolve bowel segment obstruction secondary to cystic fibrosis with distal ileal obstruction due to pseudo-meconium. The enteroscopic instillation of diatrizoic acid resulted in successful unblocking of the bowel segment (Fig. 2).
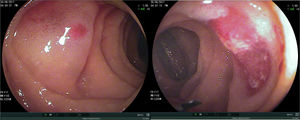
Findings in patients with enteroscopy indication for overt or occult bleedingUpon analyzing the specific subgroup of patients indicated for enteroscopy to study overt or occult gastrointestinal bleeding, the results were reported as normal in 52.17% of the cases. The main finding was the presence of ulcers, followed by angioectasias and tumor-like lesions (Table 4). The tumor-like lesions were tattooed with India ink before the surgical procedure to facilitate their location (Fig. 3).
Findings in patients with procedure indication for overt or occult bleeding.
| Enteroscopy finding | n=46 |
|---|---|
| Normal, number (%) | 24 (52.17) |
| Ulcers, number (%) | 10 (21.74) |
| Angioectasias, number (%) | 5 (10.87) |
| Lesion with a subepithelial tumor aspect, number (%) | 4 (8.69) |
| Small bowel xanthoma, number (%) | 2 (4.35) |
| Bowel segment stricture, number (%) | 1 (2.17) |
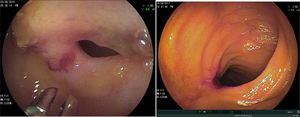
Biopsies were taken in 35 patients and were normal in 51.43% of the cases. Findings consistent with Crohn's disease were reported in 5 patients (14.28%) and inflammatory ulcers in 3 patients (8.57%) (Fig. 4). Other reported findings were GISTs, neuroendocrine tumors, and lymphangioectasias (Table 5). Four of the patients with subepithelial tumor-like lesions were operated on at our hospital and the pathology report was consistent with GIST in 50% of the cases and neuroendocrine tumor in the remaining 50%. Another 4 patients were operated on outside of our hospital and therefore their pathology reports were unavailable. Adenocarcinoma of the colon was reported in one patient that had undergone a previous colonoscopy at another hospital one month earlier, with normal results.
Findings in the biopsies taken at enteroscopy.
| Biopsy report | n=35 |
|---|---|
| Normal, number (%) | 18 (51.43) |
| Crohn's disease, number (%) | 5 (14.28) |
| Inflammatory ulcers, number (%) | 3 (8.57) |
| GIST, number (%) | 2 (5.71) |
| Neuroendocrine tumor, number (%) | 2 (5.71) |
| Lymphangioectasia, number (%) | 2 (5.71) |
| Hyperplastic polyp, number (%) | 1 (2.86) |
| Tubular adenoma with no dysplasia, number (%) | 1 (2.86) |
| Adenocarcinoma of the colon, number (%) | 1 (2.86) |
DBE is a method that enables visualization, biopsy sampling, and therapeutic intervention in the small bowel. It is a very useful procedure in patients with overt or occult gastrointestinal bleeding whose origin has not been documented through conventional endoscopic methods.3,4
In our study, the percentages of oral and anal access routes in the enteroscopies performed were similar, at 52% and 47%, respectively. Our results showing more frequent oral access varied slightly from those reported internationally, which is probably related to the type of indication. In our analysis, chronic diarrhea and neuroendocrine tumors were the most frequent indications and both access routes were required in those patients to increase diagnostic yield.5–8 Mean procedure duration in those studies was the same, at 78min for the two routes (oral and anal), and was similar to the duration reported in the Turkish study by Akarsu et al.,9 with a mean duration of 60min and 68min for the oral and anal routes, respectively. Procedure duration was also comparable in the European studies, reported at 70min and 90min, respectively.10,11 Regarding insertion length, our mean oral and rectal measurements were similar to those presented in the Asian and European literature, in which longer lengths were achieved through the anal route in the Asian studies.10,11
In our study, the most frequent indication for DBE was gastrointestinal bleeding. Overt bleeding was documented in 35.48% of the patients and occult bleeding evaluation in 13.98% for a combined total of 49.46%. That was similar to previous studies that reported gastrointestinal bleeding as the main indication for the procedure in more than 30% of the patients.5,6 Other indications in our study were chronic diarrhea in 16.13% of the cases and suspected neuroendocrine tumor in 11.83%, which was higher than that reported in previous studies.7
More than 90% of the double-balloon enteroscopies in our study were performed for diagnostic purposes, 45% were performed to carry out tattooing, and 37% were performed to take samples for their pathologic study. Thirteen procedures were performed with therapeutic intent and the most frequent intervention was the submucosal infiltration of adrenaline (saline solution at 0.9%/9 cc plus 1mg of adrenaline). Those percentages varied in previous studies, depending on the indications and endoscopic findings. For example, in a Chinese study describing an 8-year experience, biopsies were taken in 45% of the patients during enteroscopy and the most frequent finding was Crohn's disease.5
The diagnostic efficacy of enteroscopy reported in the literature varies between 40 and 80% and the frequency of therapeutic intervention between 15 and 55%.7,8 In our study, general diagnostic efficacy was 47.31%, corresponding to patients with positive findings at enteroscopy, which is within expected parameters according to previous studies. However, by analyzing only the findings that at some point could have a clinical impact, the diagnostic yield was 39%. That can be explained by the low diagnostic yield of enteroscopy for chronic diarrhea (under 50%) and neuroendocrine tumors (between 3 and 10%), which were the most frequent indications for the procedure in our study, after gastrointestinal bleeding.10,11 The frequency of therapeutic intervention in our study was calculated at 13.98% and is below the percentage published in previous studies in the international literature.7,8
The complete enteroscopy rate, defined as the examination of the entire intestine (visualization of the cecum through the anterograde route or visualization of the previously marked tattoo through either route), was 1.08% in our study, which is below the wide range of 8 to 77% reported in previous international studies.7,12 In Mexican studies, the complete enteroscopy rate has been reported from 0 to 4.3%, similar to our study results.6,7 Perhaps the low diagnostic yield is associated with the learning curve at our hospital and with the initial indication for enteroscopy.
In the present study, 53.76% of the patients underwent video capsule endoscopy prior to DBE and intestinal ulcers were the most frequent finding. Video capsule endoscopy is the initial study of choice, according to different international guideline recommendations.13 In a Mexican study, only 21% of patients had a previous video capsule endoscopy due to its low availability at that center.7 In the study by Chen et al. published in 2016, 39.76% of the patients underwent video capsule endoscopy either before or after DBE, and in the 2014 study by Akarsu et al. it appears that video capsule endoscopy was not performed in any of the 513 patients that underwent DBE.9 In the medical literature, the overall correlation between video capsule endoscopy and DBE is 41.5%. That correlation was much lower in our study, which could be related to the type of indications for DBE in our cases.14
As mentioned above, gastrointestinal bleeding, either overt or occult, was the most frequent indication for DBE in the present study. Diagnostic efficacy in that subgroup was 47.82%, which is lower than the 54 to 88% reported in other studies.8,9,12 The most frequent lesions found were ulcers, concurring with that reported in Asian studies (53%), compared with Western studies in which angioectasia was the most frequent finding.5,7
Of the patients with overt bleeding, only 6 cases underwent enteroscopy within the first 10 days of its clinical presentation. In the rest of the cases, the procedure was performed after 10 days because those patients were referred from other hospital centers. That explains the low diagnostic yield in our case series, which was also directly related to the lower percentage of therapeutic procedures.
Of the 15 patients indicated for DBE to study chronic diarrhea, the second most frequent indication in our study, diagnostic efficacy was 20%, which is low, especially when compared with Asian studies in which efficacy is under 50%. In Latin American studies, diagnostic efficacy varies from 0 to 84%, signifying a wide variability in its usefulness regarding that indication.
Tumors were found in the enteroscopies of 8.6% of the patients in the present study, which is within the 3.6 to 14% of cases reported in the literature.15 The type of pathology was determined in only 4 of our patients and included 2 GISTs and 2 neuroendocrine tumors. The other 4 tumors (subepithelial lesions with no biopsy) were not operated on at our hospital, so follow-up was not possible, and consequently, the type of pathology was unknown. That is one of the shortcomings of the present study, given that no follow-up was carried out to determine the type of pathology and disease progression.
No DBE-related complications were reported in 95.7% of the cases in our study. Complications were described in 4.3% of the patients, which is within the expected percentage, when compared with the 0.8% in diagnostic DBEs and 4.3% in therapeutic procedures reported in the international literature.5,7,12 None of the complications reported in the present study were major and they were all treated medically with no later repercussions. Contained microperforation presented in one case and was defined in an abdominal CAT scan by the presence of a limited and localized inflammatory process in a distal segment of the jejunum, with the presence of a small air bubble adjacent to the intestinal wall and no pneumoperitoneum. We believe it was a complication secondary to the tattooing carried out.
At present, ours is the largest study published in Colombia. A previous study collected information on 29 patients within the time frame of 2008 to 2009. Forty-one enteroscopies were performed and the diagnostic yield was 81%.16
In conclusion, DBE is a highly complex endoscopic procedure that was satisfactorily performed at our gastroenterology unit for diagnostic and therapeutic purposes, with no severe complications. It is the longest experience with enteroscopy reported in the Colombian population and correlates with indications for the procedure worldwide, with obscure gastrointestinal bleeding as the primary cause. The most frequent insertion route was oral, with its performance percentage very close to that of the anal route, similar to results reported in European studies. The depth reached employing oral access was also similar to that reported in European and Asian studies.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Rey AM, Reyes GA, Sierra F, Patarroyo OJ, Ardila AF, Prada LP. Enteroscopia de doble balón: experiencia de una técnica endoscópica innovadora en el Hospital Universitario de la Fundación Santa Fe de Bogotá. Revista de Gastroenterología de México. 2020;85:25–31.