In the early 1900s, contrast media began to be utilized in radiologic studies to evaluate soft tissues. Bismuth, iron, lead, and strontium were media that were not adequately regulated and so were discontinued.1 In 1902, Walter Cannon pioneered the use of barium as a contrast medium, after which it replaced bismuth, which was needed by the war industry.2 Barium sulfate is the most widely utilized agent in radiologic studies of the digestive tract and has become an essential tool because it is exact, efficient, cost-effective, and very low-risk.1 However, adverse reactions associated with its use have been described, most of which are self-limited, although there are reports of case fatalities.3 Among the complications are anaphylaxis, at 1 in 2.5 million cases,3 intoxication with neurologic symptoms,4 granuloma (first described in 1954),5 barium extravasation, venous intravasation, accidental aspiration, and barium impaction.1 Therefore, in addition to barium contrast, water-soluble contrast may be used for radiologic visualization of the gastrointestinal tract. The water-soluble medium does not cover the mucosa, as barium does, but passively fills the intestinal lumen and is indicated when there is suspected perforation or communication with the peritoneal cavity. Nevertheless, certain small perforations can only be visualized with barium, depending on their location. Water-soluble contrast use is also suggested in postoperative patients, in whom the peristalsis produced by barium is to be avoided.6 A barolith is defined as the concretion of barium sulphate and feces in the intestine after the performance of a radiologic procedure with a barium contrast agent.7 First described by Valladares in 1950,8 there are only isolated cases appearing in the literature, along with one systematic review on articles describing a total of 31 cases published within the time frame of 1950 and 2006. Obstruction due to a barolith is reported as a late presentation, associated with a low-residue diet, dehydration, colonic dysmotility, fluid and electrolyte imbalance, diabetic enteropathy, and Parkinson’s disease.8 In 1978, the use of the water-soluble contrast medium, Gastrografin® (diatrizoate), was described as a therapeutic method. Four cases had successful results, given that the medium stimulates peristalsis and its high osmolarity dissolves the impaction, its transit is adequate, despite the presence of ileus, and it does not aggravate bowel obstruction. Nevertheless, no medical associations have made any recommendations, and there have been no subsequent studies.9
The symptoms associated with baroliths are abdominal pain, nausea, vomiting, constipation, obstruction, peritonitis due to barium, and intestinal perforation. The severe complications of megarectum and abdominal compartment syndrome may present. In 2019, Pathan et al. recommended that patients with risk factors for impaction, who underwent a barium study, have x-rays taken 2–3 days after the study and receive laxatives as a preventive measure.10
We present herein a case of complete bowel occlusion secondary to baroliths. The patient was initially treated conservatively, after which he underwent successful endoscopic disimpaction. This article aims to inform its readers about the potential complications associated with barium studies, which are infrequent and rarely described in the scientific literature.
An 80-year-old man had a medical history of cognitive decline, under treatment with memantine, donepezil, and quetiapine; hyperuricemia; squamous cell cancer of the left lung, stage IIIa, undergoing treatment with 5 sessions of chemotherapy and 30 sessions of radiotherapy; and dysphagia associated with secondary mucositis, seen in a previous hospitalization by the otorhinolaryngology service, assessing swallowing dynamics that required the placement of a gastrostomy tube 6 days prior to his current illness.
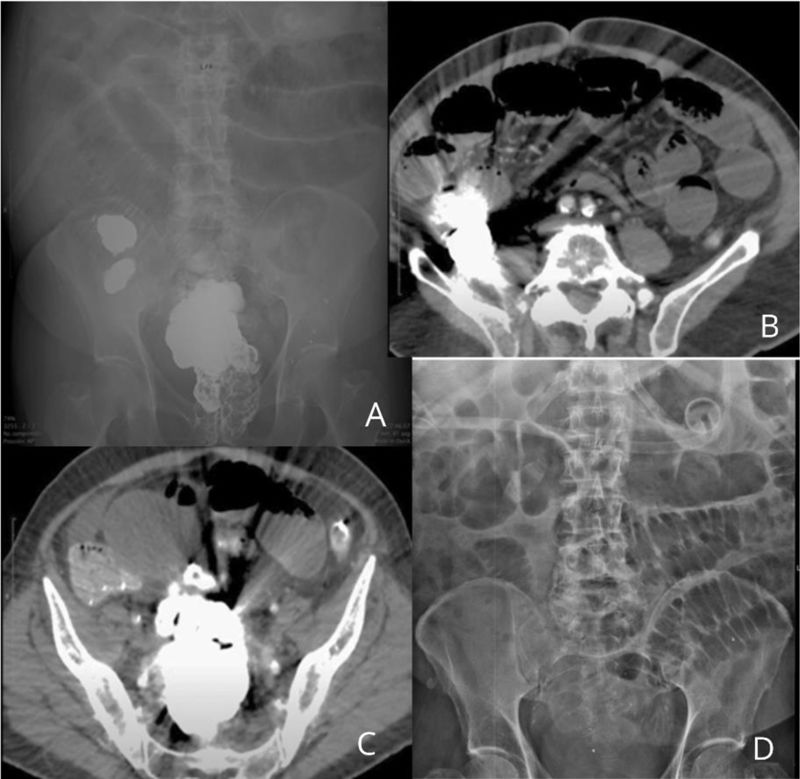
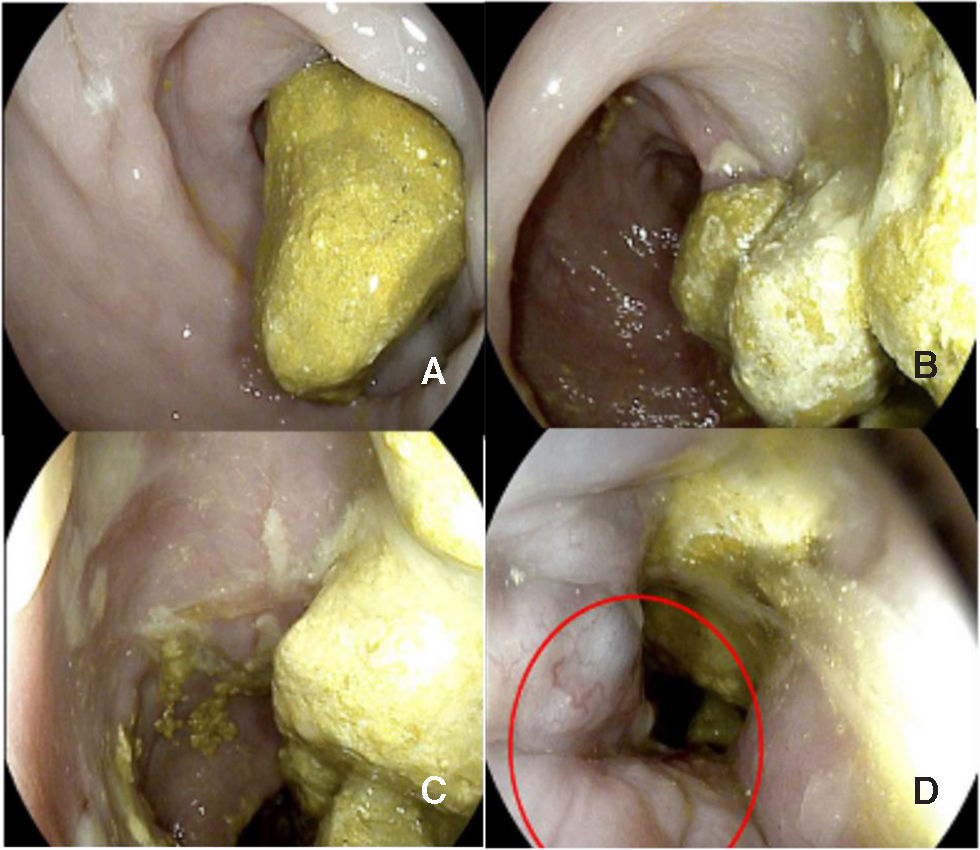
He sought medical attention at the emergency service due to inability to eat, feculent vomiting, increased abdominal perimeter, generalized colicky abdominal pain, and failure to pass gas or defecate, 4 days earlier. He was admitted to the hospital for endovenous hydration. The general laboratory work-up showed azotemia and fluid and electrolyte imbalance. Plain abdominal x-ray in two positions identified dilation of small bowel segments and the gastric chamber secondary to impaction of contrast material in the ascending colon, sigmoid colon, and rectum (Fig. 1A). An abdominal computed tomography scan revealed lower intestinal occlusion, with no evidence of a transition zone, and the presence of baroliths in the ileocecal valve and rectum (Fig. 1B and C). Manual disimpaction and oil enemas were unsuccessful due to pain and lack of cooperation. Evaluation under sedation was programmed. Fragmentation was carried out using a 25 mm Dormia basket, with the area irrigated with 2 liters of saline solution via an infusion pump. The fragments were then extracted using the basket, and the remaining residue was digitally removed, achieving total disimpaction under direct vision with flexible colonoscopy. This procedure identified stercoraceous ulcers in the rectum (Fig. 2A–D). Osmotic laxatives were administered to mobilize the barium from the ileocecal valve and facilitate its spontaneous evacuation (Fig. 1D). The patient tolerated oral diet and was discharged to his home with no complications.
Baroliths. (A) X-ray at admission showing contrast material in the ileocecal valve and rectum, along with dilation of small bowel segments and the gastric chamber. (B and C) Abdominal tomography scan showing baroliths in the ileocecal valve and rectum, with the characteristic artifact effect of barium contrast medium. (D) X-ray showing the absence of the baroliths in the colon.
This scientific letter rigorously meets the ethical conditions required for bioethical research and has obtained the necessary authorization from the corresponding ethics committee. It should be noted that, to protect patient privacy, informed consent was not obtained, as no personally identifiable information was included in the article.
Financial disclosureNo financial support was received in relation to this article.
The authors declare that there is no conflict of interest.