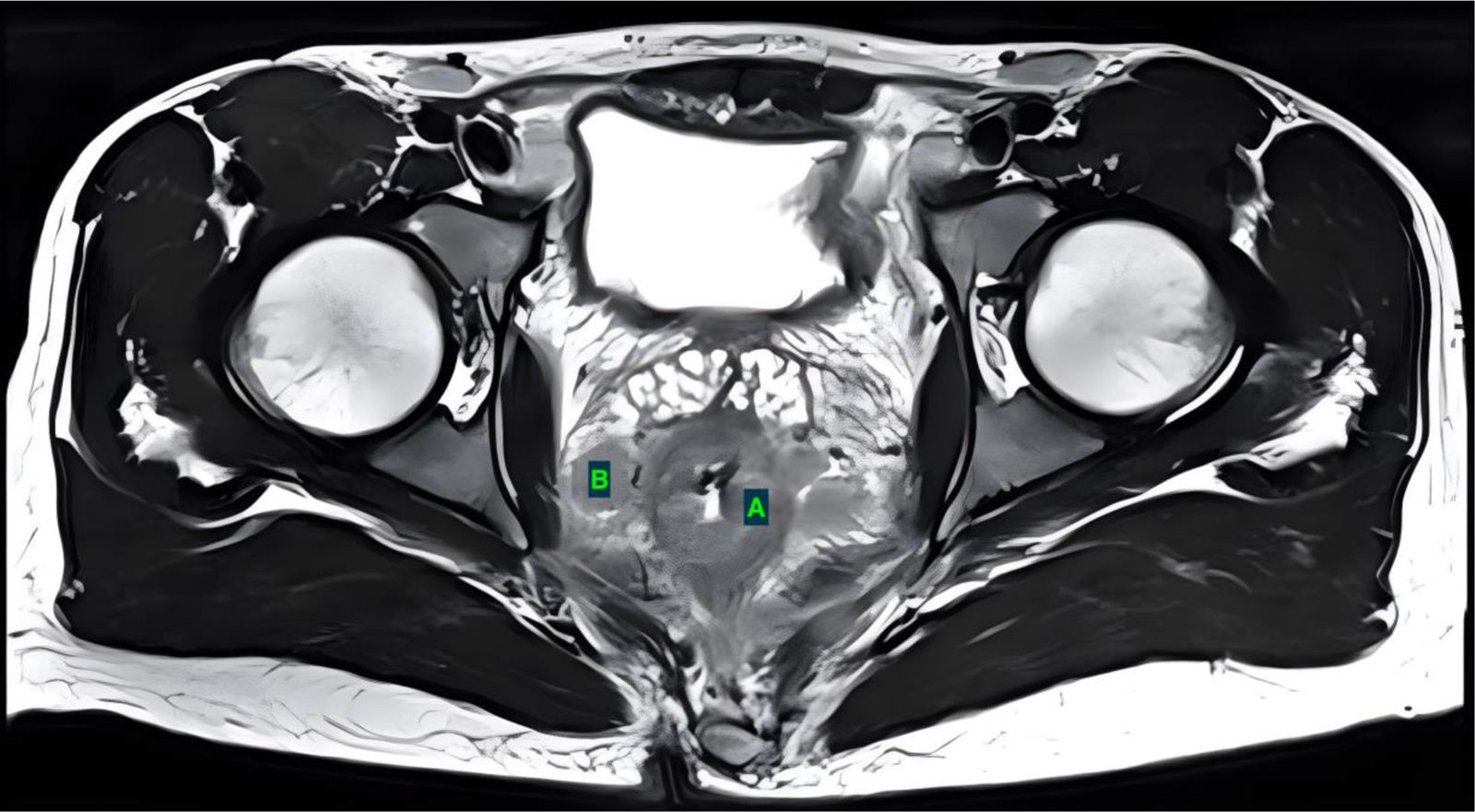
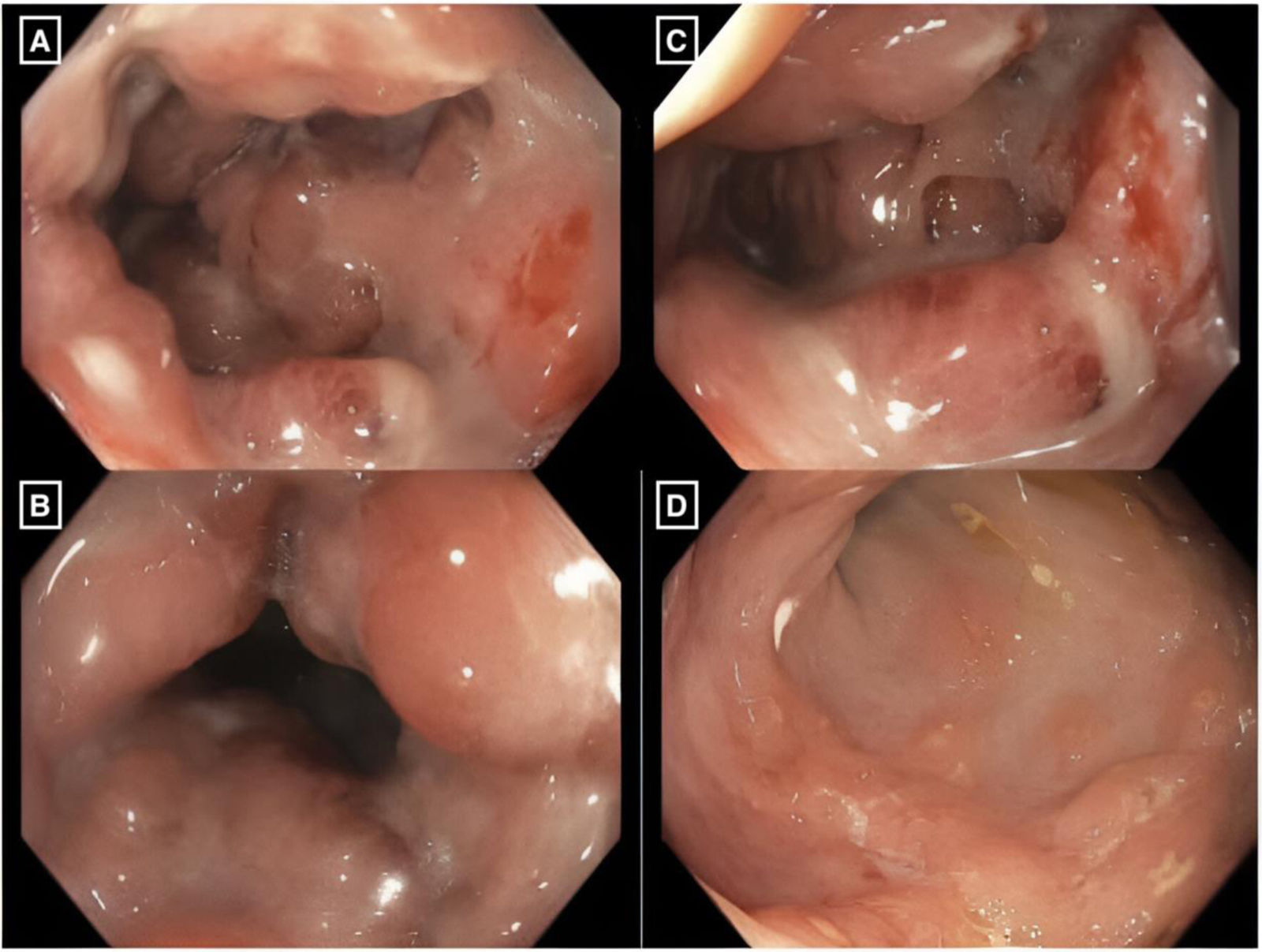
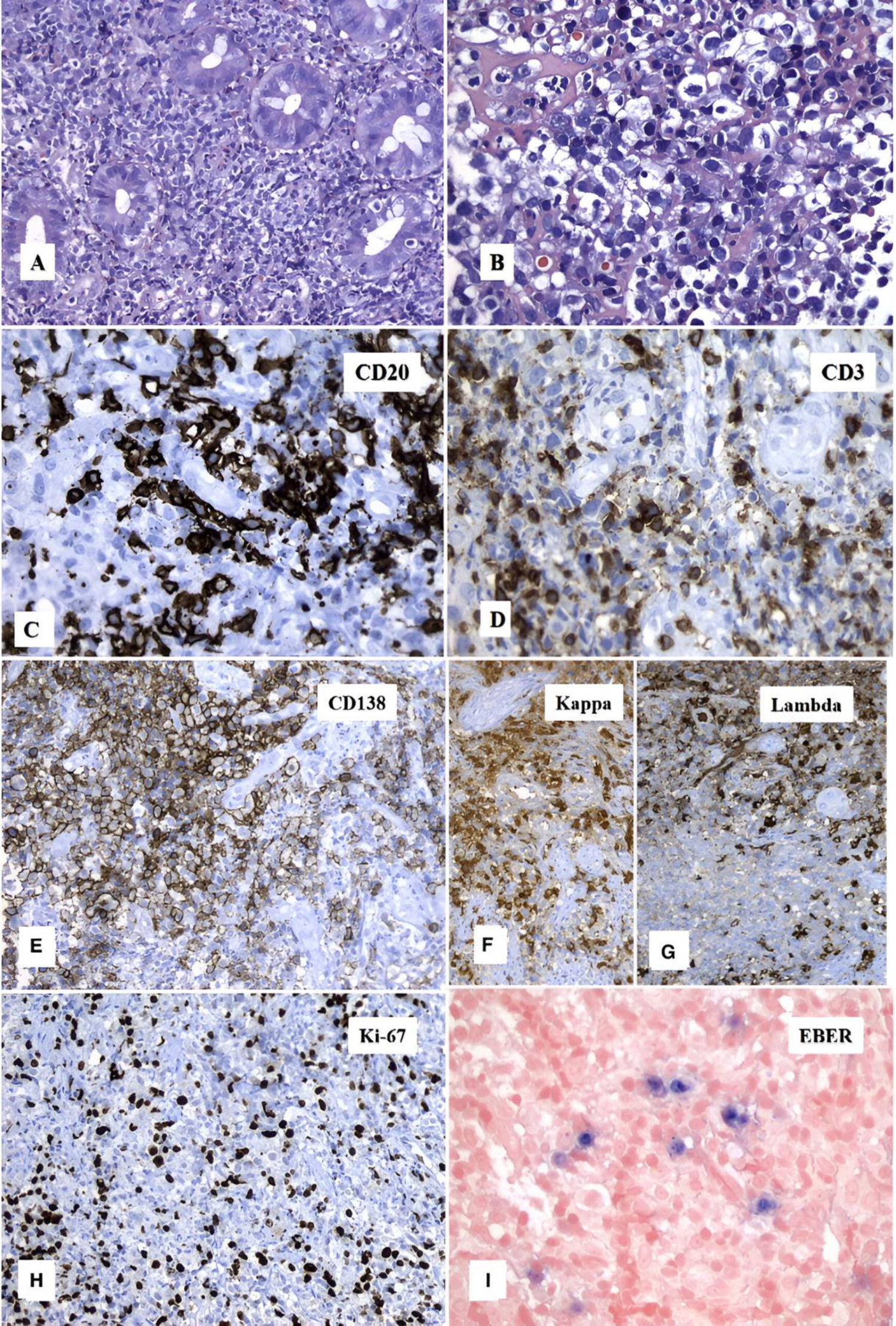
The Epstein-Barr virus (EBV) belongs to the herpes family and is also known as human herpesvirus 4. It is acquired in childhood and is generally asymptomatic but remains latent in 95% of adults. The spectrum of EBV infection is broad and ranges from local processes to lymphomas.1 Mucocutaneous ulcers have been described since 2010 as a lymphoproliferative process in persons with latent EBV infection and immunosuppression. They are considered rare and can be located in the oral mucosa (up to 41%), the gastrointestinal mucosa, and the skin. Lesions are typically single, albeit approximately 16% may be multiple. These ulcers are generally self-limited, requiring no systemic treatment.2 In 2017, the World Health Organization recognized them as a new clinical entity.3 Since the initial description of mucocutaneous ulcers, fewer than 200 cases have been reported. We present herein the case of a 30-year-old man, who had a past medical history of mild Clostridioides difficile infection and risky sexual practices but no important history of chronic degenerative diseases. He sought medical attention at the emergency service for symptoms of diffuse, colicky abdominal pain, fever, inflammatory diarrhea, proctitis, straining, and rectal tenesmus of approximately one-week progression. Digital rectal exam revealed no alterations and the laboratory work-up on admission reported: hemoglobin 11.6 g/dl, platelets 403 × 103/µl, leukocytes 9 × 103/µl, absolute lymphocytes 2.7 × 103/µl, C-reactive protein 77.4 mg/l, and erythrocyte sedimentation rate 87 mm/h. A rapid HIV antibody test was ordered and was positive, the viral load remained pending due to external circumstances, and serologic tests for Treponema pallidum, viral panel (A, B, and C), and cytomegalovirus were negative. A contrast-enhanced magnetic resonance imaging scan identified thickening of the anal canal, and more importantly, of the rectum, with a craniocaudal length of 113 mm from the anorectal junction. The thickening was circumferentially asymmetric, predominantly in the submucosa, conditioning a more than 50% reduction of the lumen (Fig. 1A). After contrast medium application, intense, diffuse, and heterogeneous enhancement, as well as multiple lymphadenopathies, were revealed (Fig. 1B). Colonoscopy was performed, and at approximately 5 cm from the anal margin, described ulcers and pseudopolyps in the mucosa, along with abundant mucus (Fig. 2A). The colonoscope was able to pass through the reduced lumen (Fig. 2B), revealing inflammatory and edematous mucosa, with signs of bleeding and fibrinopurulent material (Fig. 2C), and multiple ulcers smaller than 5 mm with well-defined 3−5 mm edges (Fig. 2D). Biopsy samples of the abovementioned tissues were taken. The histopathologic study found extensive, ulcerated, acute and chronic inflammation in the rectal mucosa, along with regenerative epithelial changes (Fig. 3A and B), positive CD20 (Fig. 3C), CD3 (Fig. 3D) and CD138 (Fig. 3E), and positive Kappa (Fig. 3F) and Lambda (Fig. 3G). Ki-67 (10–15%) was negative for dysplasia and neoplasia (Fig. 3H) and in situ hybridization (Epstein-Barr virus-encoded RNA [EBER]) was positive (Fig. 3I). Given those findings, serum EBV quantitative DNA viral load test was ordered, resulting in 25,572 copies/mL, log value of 4.41 log cp/mL. The patient received treatment with valganciclovir, and the start of antiretroviral treatment is pending.
Magnetic resonance imaging scan of the pelvis. (A) thickening of the wall of the anal canal and rectum, with a craniocaudal length of 113 mm from the anorectal union, can be observed. Said thickening is circumferentially asymmetric, predominantly in the submucosa, conditioning a reduction of more than 50% of the lumen, homogeneous and hypointense in T1 and T2, after the application of contrast medium with intense enhancement. (B) Multiple bilateral lymphadenopathies are identified in the mesorectal, obturator, presacral fat, as well as in the bilateral inguinal and common internal and external iliac fat, with oval-shaped morphology, some of which is lobulated. The lymph nodes have fatty hilum loss and there is restricted diffusion, along with contrast-medium enhancement.
Colonoscopy. (A) Ulcers and pseudopolyps in the mucosa are observed, along with abundant mucus. (B) The reduced lumen is passable and there is inflammation and edema of the mucosa. (C) Signs of bleeding and fibrinopurulent material can be observed. (D) Multiple ulcers smaller than 5 mm, with well-defined 3-5 mm edges, are shown.
Biopsy of the rectal lesion and immunohistochemistry. Periglandular lymphoid infiltrate (A and B) made up of a mixture of B lymphocytes positive for CD20 (C) and T lymphocytes positive for CD3 (D). The lymphoid infiltrate also presented with abundant plasma cells that were polyclonal (E) and expressed both Kappa (F) and Lamda (G) light chains. The proliferation index measured with Ki-67 was 10% (H) and there was multifocal positivity to the in situ hybridization for Epstein-Barr virus (Epstein-Barr encoding region [EBER]) (I).
Informed consent was requested to participate in the written research. Every individual who is admitted to the hospital as a patient signs a privacy notice authorizing the use of their personal data for research. The colonoscopy consent form also includes a section on the use of data for research purposes. This study complies with the current regulations on bioethical research, and in accordance with the regulations of the Ethics and Research Committee for Human Studies (CEIEH) of the Hospital Médica Sur, it is a case report, and so, need not be submitted. The authors declare that this article contains no information that could identify patients.
Financial disclosureNo type of financing plan was needed because only resources provided by the hospital, such as medical records, were used.
The authors declare that there is no conflict of interest.




![Biopsy of the rectal lesion and immunohistochemistry. Periglandular lymphoid infiltrate (A and B) made up of a mixture of B lymphocytes positive for CD20 (C) and T lymphocytes positive for CD3 (D). The lymphoid infiltrate also presented with abundant plasma cells that were polyclonal (E) and expressed both Kappa (F) and Lamda (G) light chains. The proliferation index measured with Ki-67 was 10% (H) and there was multifocal positivity to the in situ hybridization for Epstein-Barr virus (Epstein-Barr encoding region [EBER]) (I). Biopsy of the rectal lesion and immunohistochemistry. Periglandular lymphoid infiltrate (A and B) made up of a mixture of B lymphocytes positive for CD20 (C) and T lymphocytes positive for CD3 (D). The lymphoid infiltrate also presented with abundant plasma cells that were polyclonal (E) and expressed both Kappa (F) and Lamda (G) light chains. The proliferation index measured with Ki-67 was 10% (H) and there was multifocal positivity to the in situ hybridization for Epstein-Barr virus (Epstein-Barr encoding region [EBER]) (I).](https://static.elsevier.es/multimedia/2255534X/unassign/S2255534X25001380/v1_202511030449/en/main.assets/thumbnail/gr3.jpeg?xkr=ue/ImdikoIMrsJoerZ+w97o/wdEXW47bqlyT1CqG6R0=)

