Infectious gastroenteritis can result in unnecessary emergency room consultations. Instruments are needed to detect the risks for unfavorable progression.
AimTo develop and validate a comprehensive severity scale for acute gastroenteritis in children.
Materials and methodsData associated with complications (probable items) were determined through a MeSH search. The EsVida scale was developed with 4 theoretic domains: personal history (3 items), social problems (2 items), risks for severe gastroenteritis (4 items), and signs of fluid and electrolyte imbalance (4 items). The items were evaluated as present (one point) or absent (zero points) on a 0 to 13-point scale. To validate the instrument, an observational study was conducted at the emergency service on children from one to 13 years of age with acute gastroenteritis. The scale was re-developed utilizing the risks calculated by logistic regression analysis.
ResultsNinety-seven pediatric patients were evaluated using the EsVida scale (theoretic development). Its initial version showed an area under the ROC curve of 0.69 (95% CI of 0.6 to 0.79). After risk adjustment, it was simplified to a total of 5 items, with a score of 0 to 42.5. The new scale produced an area under the ROC curve of 0.85 (95% CI of 0.75 to 0.90). At a cutoff value of 12 points, the scale had 69.8% sensitivity and 70.5% specificity. A score below 6 indicated that patients could be managed at home at no risk.
ConclusionsThe modified EsVida scale could be used as an aid in deciding on at-home management in cases of acute infectious gastroenteritis.
La gastroenteritis infecciosa genera consultas innecesarias a urgencias. Se necesitan instrumentos para detectar los riesgos de una evolución desfavorable.
ObjetivosConstruir y validar una escala integral para la gravedad de una gastroenteritis aguda en niños.
Material y métodosA través de una búsqueda de MeSH, se determinaron datos asociados con complicaciones (probables ítems). Se construyó una escala (EsVida) con 4 dominios teóricos: antecedentes personales (3 ítems), problemas sociales (2 ítems), riesgos de gastroenteritis severa (4 ítems) y signos de compromiso hidroelectrolítico (4 ítems), evaluados como presencia (un punto) o ausencia (cero puntos), escala de 0 a 13 puntos. Para su validación se realizó un estudio observacional en urgencias, en niños de uno a 13 años con gastroenteritis aguda. La escala fue reconstruida con los riesgos calculados por análisis de regresión logística.
ResultadosNoventa y siete pacientes pediátricos fueron evaluados con la escala EsVida (construcción teórica). En su versión inicial mostró un área bajo la curva ROC de 0.69 (IC 95% de 0.6 a 0.79). Con el ajuste por riesgos, se simplificó a 5 ítems, con 0 a 42.5 puntos; esta nueva escala evidenció un área bajo la curva ROC de 0.85 (IC 95% de 0.75 a 0.90). Con un nivel de corte de 12 puntos, presentó una sensibilidad del 69.8% y una especificidad del 70.5%. Un puntaje inferior a 6 indicaría manejo en domicilio sin riesgo.
ConclusionesLa escala modificada EsVida puede ser usada para apoyar la decisión de un manejo domiciliario en casos de gastroenteritis aguda infecciosa.
Acute infectious gastroenteritis (AIG) is a transitory disorder caused by an enteric infection, characterized by the sudden onset of diarrhea, with or without vomiting, and lasting fewer than 14 days.1 It is one of the main reasons for primary healthcare consultation in emergency rooms,2 especially when the patient presents with fever, altered level of consciousness, vomiting, and important pain.3 Even though the usual progression is toward self-limitation, severe episodes can lead to patient death. In Mexico, a governmental study conducted in 2003 reported 4556 deaths caused by intestinal infections.2
The cornerstone of AIG management is the prevention of dehydration, or if already present, opportune rehydration.4 However, the additional factors of very young age, previous malnutrition, comorbidities, an important medical history (prematurity, vaccination status), grade of enteral damage (presence of blood), and unfavorable socioeconomic environments, among others, can be conducive to unfavorable outcome.3,5,6
In the majority of episodes, mild and even moderate AIG can be managed at home, with previous training and constant communication, to avoid the risk of hospital-acquired infections inherent in hospitalization. The therapeutic decisions made in the emergency room should be carried out quickly. Thus, there is a need for instruments that can rapidly and comprehensively detect the risk for unfavorable progression. At present, there are no guidelines, and the pediatric patient is evaluated through an extensive interview with a family member.
Aims: to develop and validate a scale for the comprehensive evaluation of AIG severity in a minor, to prevent unnecessary hospitalizations.
Materials and methodsThe present study was approved by the research and ethics committee of the Hospital Español.
Development and validation of the EsVida scaleReview of the literatureA MeSH search was conducted utilizing the following keywords
guidelines, infectious gastroenteritis, pediatrics, dehydration, scale, dehydration scale. The most frequently reported data from the articles found were analyzed to create a list of probable items or indicators for developing the scale. The selected items were those that were the easiest to detect, the most important for clinicians, obtainable in fewer than 15s, and those that were not laboratory test data. The proposal was agreed upon by a panel of pediatricians from the Hospital Español, producing a 15-question scale (Table 1).
The “Es Vida” scale evaluation for the management of children 0 to 13 years of age with acute diarrhea.
| Personal history | 0 points | 1 point |
|---|---|---|
| Presents with malnutrition | No | Yes |
| Has a chronic disease (underlying treatment) | No | Yes |
| Has complete rotavirus vaccination regimen | Yes | No |
| Social problems | ||
|---|---|---|
| Educational level of the mother or primary guardian | Professional level | Middle or lower level |
| Age of the patient | >5 years | ≤5 years |
| Disease-related criteria | ||
|---|---|---|
| Number of bowel movements in the past 24h | ≤5 | >5 |
| Number of episodes of vomiting in the past 24h | ≤2 | >2 |
| Presence of mucus, blood, or both, in any stools | No | Yes |
| Fever above 38°C | No | Yes |
| Clinical signs of fluid and electrolyte imbalance | ||
|---|---|---|
| Sunken anterior fontanel or cold extremities | No | Yes |
| Capillary refill time | ≤2s | >2s |
| Tearless crying or sunken eyes | No | Yes |
| Altered level of consciousness (somnolence, irritability, or variations) | No | Yes |
| Score |
The initial scale was developed, focusing on 4 important areas: the personal history of risk for severe acute gastroenteritis, social management problems, severe gastroenteritis criteria, and clinical signs of dehydration.
Each item had 2 options (presence/absence) to achieve application simplicity. Each item had a numerical value of one, if it presented a condition of risk, and of zero, if it did not (Fig. 1). The final scale had a range of 0 to 13 points. Each item was defined as follows:
Malnutrition: weight for age and sex in the third percentile, or a body mass index below the third percentile for age and sex.7
Comorbidity: chronic underlying disease reported by the parents with evidence of its medical management; a history of prematurity is particularly taken into account.
Educational level of the mother: selected as a social problem related to infant care, obtained through interview, and grouped into high school level or lower as a risk factor versus professional level.
Age of the patient: children under 5 years of age are considered at greater risk for dehydration and the development of complications.
Previous rotavirus vaccination: children are at higher risk if not vaccinated; vaccination against rotavirus is considered complete, if the family member has the official vaccination record showing its application.
Bowel movements: a higher risk is assumed if the patient has had 5 or more bowel movements within 24h, with an extra point if the stools contained mucus and/or blood.
Mucus or blood in stools: reported by the parents or physician during emergency room stay.
Vomiting: indicates risk with 2 or more episodes within the previous 24h.
Fever: axillary body temperature above 38°C during emergency room stay.
Dehydration: determined in children under 2 years of age, by the presence of a sunken anterior fontanel, and in older children, by reduced temperature in the upper and lower limbs (if hands and feet are cold to the touch)3,4 and mucosal dryness.8
Capillary refill time: measured by tissue reperfusion after pressing a fingernail; considered prolonged when blood takes longer than 2s to return to the tissue.8
Altered level of consciousness: presence of somnolence or irritability.8
Tearless crying or sunken eyes: parents are asked about the condition, and the emergency room physician examines the child.
ValidationFor the validation phase, an observational study was conducted at the pediatric emergency service at a hospital in Mexico City, located in the northwestern zone of the Miguel Hidalgo municipality. We included children from one to 13 years of age, of either sex, that came to the emergency room due to having clinical signs of acute gastroenteritis, for fewer than 7 days. Patients with chronic diarrhea or intestinal diversions were excluded, as were immunocompromised patients.
After patient evaluation, an invitation to participate in the study was extended to the primary caretaker or guardian of the child. Once participation was accepted, a direct interview was carried out to obtain the information covered in the first 3 domains of the EsVida scale. The last domain (clinical signs of dehydration) was evaluated by the head physician of the emergency service, for a period not longer than 5min. The treatment of the patient was provided by the treating physician, with no intervention.
The decision for hospitalization was made by the treating physician. However, for the safety of minors, the recommendation established at our institution is to hospitalize all children presenting with a total carbon dioxide (tCO2) level below or equal to 22mmol/L.9,10
Statistical analysisThe patients were grouped as inpatients or outpatients, depending on the emergency room evaluation. The qualitative variables were expressed as simple or relative percentages through the chi-square test and the quantitative variables were expressed as means plus standard deviation or medians with quartile values, depending on their distribution, determined through the Kolmogorov–Smirnov test. The Student's t test for independent groups was employed for the cases of normal distribution and the nonparametric Mann–Whitney U test for the cases of abnormal distribution. A receiver operating characteristic (ROC) curve and its area under the curve were plotted to determine the validity of the scale. Likewise, the ROC curve was utilized to establish the better performing cutoff points, determining sensitivity and specificity, as well as the positive and negative likelihood ratios. A point value and 95% confidence interval were given for each calculation. Finally, to optimize and simplify the scale, a stepwise logistic regression analysis was performed on the items considered to be independent factors, and on hospitalization as the outcome variable.
The Pearson's test was utilized to determine the correlation between the points on the scale and the tCO2 values. The analyses were performed with the SPSS version 22, Prims 2, and JASP2 programs. Statistical significance was set at a p<0.05.
Ethical considerationsThe authors declare that no personal information that could identify patients was used in the present study, nor did it represent a risk, given that only the medical notes from the pediatric emergency service were reviewed and no intervention was included in the treatment. The parents or guardians of the children signed written statements of informed consent.
ResultsA total of 97 pediatric patients were included. According to the hospitalization criterion of moderate-to-severe dehydration (tCO2≤22mosmol/L), 53 (54.6%) of the patients were admitted to the hospital and the remaining 45.3% were treated as outpatients. As shown in Table 2, male sex predominated in the two groups, but with no statistical significance. With respect to age, the hospitalized children's group was one year older (p<0.001). The vaccination regimen could not be corroborated in the outpatients, given that the parents did not have the official vaccination record with them at the emergency room. Therefore, we were not able to demonstrate differences regarding the application of the rotavirus vaccine. Regarding risk factors for complications, we found greater malnutrition and comorbidities in the hospitalized group, with statistically significant differences (p<0.05). Finally, the educational level of the mothers was similar in the two groups.
Patient characteristics according to hospitalization decision (n=97).
| Hospitalized (n=53) | (Not hospitalized) n=44 | p | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Sex | |||||
| Male | 30 | 56.6 | 30 | 68.2 | 0.24a |
| Female | 23 | 43.4 | 14 | 31.8 | |
| Age in years | |||||
| Median | 3 | 4 | <0.01b | ||
| 25th percentile | 1 | 3 | |||
| 75th percentile | 5 | 6 | |||
| Min-max | 1–12 | 1–13 | |||
| Vaccinated against rotavirus | |||||
| No (or not known) | 4 | 7.5 | 44 | 100 | <0.001a |
| Complete regimen | 49 | 92.4 | 0 | 0 | |
| Presence of malnutrition | |||||
| Yes | 21 | 39.6 | 5 | 11.4 | <0.0001a |
| No | 32 | 60.4 | 39 | 88.6 | |
| Comorbidityc | |||||
| Yes | 15 | 28.3 | 4 | 9.1 | 0.02a |
| No | 38 | 71.7 | 40 | 90.9 | |
| Mother's educational level | |||||
| Middle or lower level | 49 | 92.4 | 41 | 93.2 | 0.89a |
| Professional level | 4 | 7.6 | 3 | 6.8 | |
| Clinical data | |||||
| >2 episodes of vomiting vs. ≤2 | 43 | 81.1 | 28 | 63.6 | 0.05a |
| >5 bowel movements vs. ≤5 | 28 | 52.8 | 10 | 22.7 | <0.001a |
| Mucus/blood vs. no mucus/blood | 13 | 24.5 | 4 | 0.1 | 0.05a |
| Fever vs. no fever | 23 | 43.4 | 16 | 36.4 | 0.48 |
| Examination data | |||||
| Cold extremities and/or sunken fontanel | 3 | 5.6 | 0 | – | 0.11a |
| Capillary refill time>2s | 34 | 64.1 | 16 | 36.4 | 0.001a |
| Tearless crying or sunken eyes | 11 | 20.7 | 4 | 9.1 | 0.11a |
| Dry mucous membranes | 42 | 79.2 | 26 | 59.1 | 0.03a |
| Pallor | 44 | 83.0 | 28 | 63.3 | 0.03a |
| Altered level of consciousness | 7 | 13.2 | 1 | 2.2 | 0.05a |
| Total CO2mmol/mEq | |||||
| Mean±1 SD | 17.8 | ±3 | 19.7 | ±1.9 | <0.001d |
SD: standard deviation.
Regarding diarrhea-related illness, a higher number of patients in the group admitted to the hospital had more frequent vomiting, more bowel movements during the last 24h, and more episodes of stools with mucus, with or without blood. The history of fever was similar in the inpatient and outpatient groups (Table 2).
Physical examination revealed a higher number of patients with slow capillary refill, dryness of the mucous membranes, pallor, and altered level of consciousness, in the inpatient group (p<0.05). Hypotensive or sunken fontanel, with or without cold extremities, as well as tearless crying or sunken eyes, were more common in the inpatient group, albeit the differences were not statistically significant (Table 2). Likewise, as expected from our classification criterion, tCO2 levels were lower in the hospitalized patients.
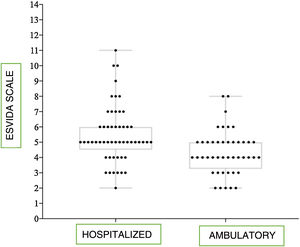
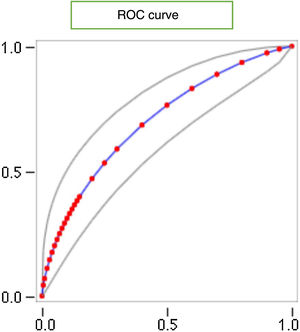
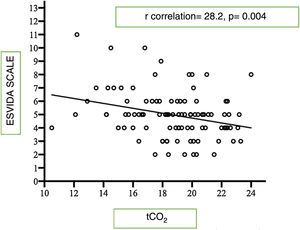
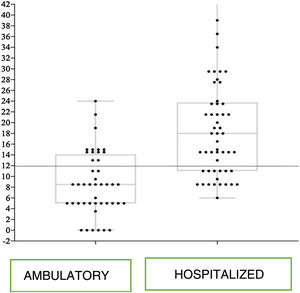
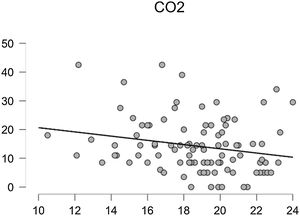
EsVida scale resultsIn evaluating the scores of the EsVida scale, according to its theoretic development, we found higher scores for the inpatient children versus those treated as outpatients (median [min–max] of 5 [2–11] vs. 4 [2–8], Mann–Whitney U test, p<0.001) (Fig. 1). When the validity of the scale was analyzed through the ROC curve (Fig. 2), performance was regular, with an area under the curve of 0.69. With that curve, 2 possible cutoff points for hospitalization risk were determined: 5 or more and 6 or more. Table 3 shows the sensitivity, specificity, and likelihood ratios calculated for each cutoff level. According to the data, the cutoff point criterion of 6 or more was more sensitive and specific than 5 or more. Only 3 hospitalized patients had scores above 9 on the scale. The rest of the scores were shared between the two groups and the lowest score in both groups was 2. Likewise, there was a statistically significant low correlation between the tCO2 values and the EsVida scale (r=−0.28).
EsVida scale validity, according to cutoff point.
| Cutoff point | Sensitivity | Specificity | Positive likelihood ratio | Negative likelihood ratio |
|---|---|---|---|---|
| Original scale | ||||
| ≥6 vs. <6 | 39.6 (27.6–53.1) | 84.1 (70.6–92.1) | 2.4 (1.2–5.3) | 0.7 (0.6–0.9) |
| ≥5 vs. <5 | 75.5 (62.4–85.1) | 56.8 (42.2–70.3) | 1.7 (1.3–2.5) | 0.4 (0.2–0.7) |
| New scale | ||||
| ≥ 12 vs. <12 | 69.8 (54.3–80) | 70.5 (54.6–82.7) | 2.3 (1.4–3.7) | 0.4 (0.3–0.6) |
Data are expressed as estimates (95% confidence interval).
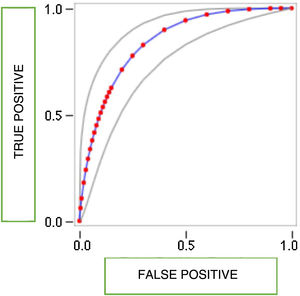
According to the logistic regression analysis, the factors of the scale most associated with hospitalization were: having a comorbidity, malnutrition, having had 5 or more bowel movements, pallor, and a capillary refill time of more than 2s. Those data produced a pseudo-R2 of 0.54. A new, simpler scale was developed with those factors, with the calculated odds ratios as the scores. The scoring range of the modified EsVida scale (Table 4) was from 0 to 42.5 points and the mean differential values between the two groups were maintained (median [min-max] 18 [6–42.5] hospitalized patients vs. 8.5 [0–24] outpatients, Mann–Whitney U test, p<0.001). Validity measured with the ROC curve (Fig. 3) showed better performance, with an area under the curve of 0.84. Likewise, a score equal to or above 12 points was a better cutoff value, resulting in sensitivity and specificity of around 70% (Table 3). With the modified scale, none of the outpatients vs. 9 (17%) of the hospitalized patients had a score above 26, and none of the hospitalized patients vs. 19 (43%) outpatients had a score below 6. Finally, the modified scale also showed a low negative correlation with the tCO2 levels (Figs. 4–6).
The need to predict which children with AIG will require hospitalization motivated us to develop and validate the EsVida scale. Our aim was to make the scale available to primary healthcare personnel, as a support measure in managing emergency service arrivals. The prediction validity of the first version of the scale, which was sustained by previously published evidence and supported by the experience of pediatricians, was moderate. It was easy to apply but had a varying sensitivity and specificity, depending on the cutoff value. It was more sensitive with a cutoff point of 5 and more specific with a cutoff point of 6 but its discrimination between the two groups was low. Therefore, we re-analyzed the items, according to their weight (OR), which allowed us to simplify and improve the scale's predictive validity. The modified scale only required 5 items to evaluate possible hospitalization and it provided better discrimination between groups.
The decision to hospitalize children for the management of AIG is multifactorial. It is primarily related to the clinical condition of the child, but the presence of risk factors associated with complications must also be taken into account, as well as sociodemographic and emotional factors.1,3–6,11,12 Our initial scale included those areas, but in the modified scale, the first 2 factors appear to be more important for deciding on surveillance and hospital management.
With respect to AIG management, the ESPGHAN guidelines,5 the Latin American guidelines,11,12 the Mexican clinical practice guidelines,1 and more recent reviews, such as the emergency action guidelines from the clinic of the Universidad de Navarra,13,14 state that shock, severe dehydration with body weight loss of 9%, failure of oral rehydration therapy, and a suspected surgical condition are criteria for hospitalization, with age below 6 months, more than 8 bowel movements or more than 4 episodes of vomiting in 24h, neurologic alterations, or social problems (parents not able to manage the child's condition at home), as risk factors.
The EsVida scale takes those criteria into account but our aim was the opportune diagnosis and prevention of shock to favor patient outcome, which was why we proposed the identification of risk factors, as well as the clinical data, that could favor complications.
The circulation of the modified EsVida scale could have the advantage of informing both healthcare personnel and mothers about specific points to be aware of during an episode of AIG. We believe that the data to be asked or observed are easy to record and the final score is tallied by simply adding up the points. Pallor is a subjective item in our scale's clinical evaluation, whose interpretation could vary, depending on the examiner. Nevertheless, it is a datum that is commonly referred to by parents when they arrive at the emergency room. On the modified scale, a score above12 should be an alerting signal for emergency care, whereas a score below 6 can calm the parents, indicating at-home management. Importantly, the progression of diarrheic episodes should always be supervised by a physician after his/her evaluation of the child.
As with all scales, the EsVida scale should be externally validated through its use under conditions different from ours. Other studies are needed, if an analysis of its usefulness in populations with low educational levels is to be performed.
In conclusion, the modified version of the EsVida scale appears to be valid and useful as an aid for making the decision between hospital or at-home management in cases of AIG. Its use could reduce unnecessary hospitalizations.
Financial disclosureThe present work was financed by the authors themselves.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Fernández-Garrido CL, Bernárdez-Zapata I, Iglesias-Leboreiro J, Rendón-Macías ME. Construcción y validación de la escala EsVida para la valoración del requerimiento de manejo en urgencias de una gastroenteritis infecciosa. Revista de Gastroenterología de México. 2021;86:145–152.