Nonalcoholic fatty liver disease (NAFLD), or metabolic dysfunction-associated fatty liver disease (MAFLD), according to a new consensus-driven nomenclature proposed by a group of experts1, has an estimated prevalence of 25 to 30% in the adult population and is the most frequent cause of abnormal liver function tests (LFTs) seen in the primary healthcare setting in Europe and North America2.
The pathophysiology of NAFLD is complex but appears to be a continuum of entities, ranging from obesity to metabolic syndrome and diabetes. Environmental factors can affect the genetic expression, causing weight gain. When the expansion capacity of the subcutaneous tissue is reached, it produces an increase in free fatty acid (FFA) mobilization, resulting in visceral and ectopic fat deposition. The increase in FFA deposition promotes insulin resistance (IR), inhibiting insulin-mediated glucose uptake. Thus, adipose tissue IR facilitates lipolysis and increases the flow of FFAs to the liver, inducing hepatic IR and enhancing glucose production, hepatic de novo lipogenesis, and atherogenic dyslipidemia3.
Those pathogenic mechanisms are reflected in the prevalence of NAFLD, in parallel with the prevalence of obesity, metabolic syndrome, and diabetes. The prevalence of obesity in patients with NAFLD is 51%, the prevalence of obesity in patients with nonalcoholic steatohepatitis (NASH) is 81%, and the prevalence of NAFLD in patients with obesity varies from 60 to 95%4–6.
NAFLD has a broad clinical spectrum, ranging from simple steatosis with fatty infiltration of ≥ 5% of the liver parenchyma and no ballooning degeneration or inflammation, to NASH, with necroinflammation and hepatocellular damage (ballooning degeneration of hepatocytes, Mallory bodies, or megamitochondria), and finally to the development of cirrhosis and a greater risk for hepatocellular carcinoma7.
End-stage liver disease secondary to NAFLD is currently the main indication for liver transplantation8.
Importantly, only a small number of patients with NAFLD (approximately 5%) develop clinically significant liver disease during follow-up, and the severity of liver fibrosis is the main factor determining outcome in those patients.
Unfortunately, normal aminotransferase (ALT/AST) levels do not rule out progressive disease in NAFLD, and patients with normal ALT can develop progressive liver disease9. In addition, ALT can be normal in > 50% of patients with NASH and up to 80% of patients with NAFLD. ALT levels are neither indicative nor predictive of NASH or fibrosis stage.
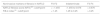
The advantage of the noninvasive fibrosis tests, such as the FIB-4 index and the NAFLD fibrosis score (NFS), is their capacity to rule out advanced liver disease (F3-F4 fibrosis stages) but they are less accurate in identifying intermediate stages of fibrosis10. Those scores are frequently used in clinical practice due to their accessibility. However, neither the FIB-4 score nor the NFS has a sufficiently adequate positive predictive value (PPV) to enable them to be used on their own, for predicting NASH and fibrosis11 (Table 1).
Liver ultrasound (US) is the most widely used imaging method for diagnosing hepatic steatosis. The advantages of liver US are its consistent availability and the fact that it is well established, easily tolerated, and relatively inexpensive. A meta-analysis that included more than 2,800 patients showed that liver US could distinguish the presence of moderate-to-severe fatty liver, with 85% (80-89%) sensitivity and 93% (87-97%) specificity. In clinical practice, liver US detects steatosis when the fat content of the liver is greater than 10 to 20%. Nevertheless, its diagnostic accuracy for liver steatosis decreases, in patients with coexisting obesity and kidney disease, and it is not appropriate for evaluating fibrosis12,13.
One of the most reliable noninvasive tools for ruling out advanced fibrosis is liver elastography, whether shear wave elastography (SWE) or vibration-controlled transitory elastography (VCTE), given that its negative predictive value (NPV) is better than its PPV. For example, when utilizing VCTE, fibrosis is unlikely, with a value < 6 kilopascals (kPa) whereas higher values increase the probability of more severe fibrosis, which predicts the risk for decompensation. However, fibrosis can be overestimated in cases of cholestasis, obesity, hepatitis, and hepatic congestion. Likewise, values > 14 kPa are predictive of cirrhosis and values > 20 kPa correlate well with clinically significant portal hypertension14,15.
In the present issue of the Revista Mexicana de Gastroenterología, Marciano et al.16 conducted a multicenter study on adult patients with NAFLD, followed by hepatologists, in which they calculated the FIB-4 index and NFS, and the patients with at least one score indicative of indeterminate or high risk for fibrosis, were to undergo elastography studies for fibrosis staging. Of the 238 patients evaluated, 54% had at least one noninvasive score that suggested indeterminate or high risk for fibrosis, and of those patients only 56% underwent the later studies for fibrosis staging. The main limitation to ordering those studies was related to medical insurance coverage and the cost of the elastography tests.
In their study, Marciano et al.16 emphasize that a high percentage of the patients with NAFLD, evaluated using the noninvasive scores, had an indeterminate risk or a high risk for fibrosis. However, less than half of those patients underwent further diagnostic testing, demonstrating poor adherence to the currently proposed algorithms, on the part of the hepatologists.
Some advisory comments are in order. The study discussed herein was designed before the two-step algorithms for fibrosis evaluation were widely accepted. Furthermore, the value of those algorithms continues to be challenged by a heterogeneous disease with no approved drug treatment, in which lifestyle changes are the basis for all treatment plans and weight loss (≥ 3 to 10%) is associated with histologic improvement.
In addition, it is difficult for those algorithms to be adopted by the different healthcare systems, given the wide variety of evaluation methods and costs involved. That situation is reflected in the study discussed herein, in which half of the physicians stated that the main obstacle for further diagnostic study of the patients was the lack of medical insurance and problems related to costs. Despite those limitations, the findings of Marciano et al. are important, both adding valuable information to the growing evidence of the problem NAFLD represents for Latin American healthcare systems and underlining the need for standardizing the diagnostic algorithms in patients with NAFLD.
Adequate use of the noninvasive tests can aid in improving risk stratification in patients with NAFLD, as well as in satisfactorily detecting the patients in F2/F3 stages of fibrosis. Thus, current guidelines propose the use of noninvasive tools for evaluating fibrosis and recommend a two-step algorithm for simplifying the clinical management of patients with NAFLD7. Previous studies have also shown that improving the referral pattern at the primary healthcare level, for patients with NAFLD, could reduce the number of unnecessary referrals to specialists by more than 80%17.
The study by Marciano et al.16 emphasizes the fact that NAFLD is common and affects more than one-fourth of the population. Noninvasive tests are needed to identify which patients with NAFLD require closer follow-up. Aminotransferase level quantification and liver US are not sensitive for detecting patients with fibrosis. In addition, the isolated use of the FIB-4 index and NFS, as well as elastography studies, lacks sufficient PPV for predicting NASH and liver fibrosis. Their combined use is a better option (e.g., FIB-4 plus VCTE). This is an essential area of research, especially because there is preliminary evidence from ongoing research that the use of drugs that improve steatosis leads to the resolution of NASH, as well as fibrosis.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Montaño-Loza AJ. Evaluación de la fibrosis en pacientes con enfermedad de hígado graso no alcohólico. Rev Gastroenterol Méx. 2022;87:1–3.