Critically ill patients present with a broad spectrum of gastrointestinal motility disorders that affect the digestive tract. Our aim was to compare the effect of two prokinetic drugs on gastric electrical rhythm in critically ill septic patients, measured through surface electrogastrography (EGG).
Material and methodsA prospective triple-blinded randomized study was conducted on 36 patients admitted to the intensive care unit (ICU) with the diagnosis of septic shock. They were randomized to receive metoclopramide or domperidone. We assessed dominant frequency (DF), percentage distribution over time, and dominant power (DP), which represents the strength of contraction, before and after administration of the study drugs.
ResultsReliable electrogastrograms were achieved in all patients. In relation to the distribution of DF over time, 64% of patients had dysrhythmia, the mean baseline DF was 2.9 cpm, and the mean DP was 56.5μv After drug administration, 58% of the patients had dysrhythmia, the mean DF increased to 5.7 cpm (P<.05), and the DP did not change (57.4μv2). There were no significant differences between drugs. In the metoclopramide group, the baseline DF was 2.1 cpm and the baseline DP was 26.1μv2. The post-drug values increased to 5.4 cpm and 34.1μv2, respectively. In the domperidone group, the baseline DF was 3.7 cpm and the baseline DP was 86.9μv2. After drug administration, the DF increased to 6.1 cpm and the DP decreased to 83.5μv2.
ConclusionsBoth metoclopramide and domperidone similarly increased the DF of gastric pacemaker activity and improved gastric motility by restoring a normogastric pattern. Gastric dysmotility is frequent in septic patients.
Los pacientes críticos exhiben un amplio espectro de trastornos de motilidad gastrointestinal que afectan al tracto digestivo. Nuestro objetivo fue comparar el efecto de 2 fármacos procinéticos sobre el ritmo eléctrico gástrico en pacientes críticos sépticos mediante electrogastrografía de superficie.
Material y métodosSe realizó un estudio prospectivo, aleatorizado, triple ciego en 36 pacientes ingresados en la unidad de cuidados intensivos con diagnóstico de shock séptico y aleatorizados para recibir metoclopramida o domperidona. Se evalúo la frecuencia dominante (FD), distribución porcentual en el tiempo y potencia dominante (PD) que representa la fuerza de la contracción, antes y después de los fármacos del estudio.
ResultadosSe obtuvo electrogastrograma confiable en todos los pacientes. Según la distribución de FD en el tiempo el 64% de los pacientes tenían disritmia, la FD basal promedio fue 2.9cpm y la PD promedio fue 56.5μv. Posterior a la administración del fármaco el 58% tenía disritmia, la FD promedio aumentó a 5.7cpm (p<0.05), mientras que la PD no cambió (57.4μv2) para ambos fármacos. No hubo diferencias significativas entre los fármacos. En el grupo metoclopramida la FD basal fue 2.1cpm y la PD 26.1μv2. Posfármaco los valores fueron 5.4cpm y 34.1μv2. En el grupo domperidona los valores basales fueron FD 3.7cpm y PD 86.9μv2 y posfármaco 6.1cpm y 83.5μv2 respectivamente.
ConclusionesTanto la metoclopramida como la domperidona aumentan la FD del marcapasos gástrico de forma similar, y podrían mejorar la motilidad gástrica restableciendo el patrón normogástrico. La dismotilidad gástrica es frecuente en pacientes sépticos.
Critically ill patients present with a broad spectrum of gastrointestinal motility disorders that affect the digestive tract, from the esophagus to the rectum. Those disorders include lower frequency and amplitude of propulsive contractions in the esophagus, antral hypomotility, loss of antrum-pylorus-duodenum interaction, increased retrograde activity, and persistence of phase III of the motor migrating complex (MMC) in the small bowel. Dysmotility is likely due to multiple conditions, including surgical interventions, decreased splanchnic perfusion, bowel edema, and drug use, mainly sedatives and vasoactive agents. That issue has significant clinical relevance. Manifestations are regurgitation, gastroparesis, vomiting, ileus, and delayed defecation and are associated with adverse effects such as aspiration pneumonia and bacterial translocation.1,2
Little progress has been made over the last decades in the development of new promotility agents, making it necessary to optimize treatment with the old available drugs. Erythromycin, cisapride, metoclopramide, and domperidone have limitations in efficacy, as well as the potential to induce serious adverse events.3–5
In addition, gastrointestinal motility evaluation in the critical care setting is a challenge, given the instability of patients and the presence of multiple invasive devices. Plasma acetaminophen level determination is not a routine practice, and the relation between gastric residual volume to the success of enteral feeding and the risk of aspiration is inconsistent. Other methods, such as the breath test with radioisotopes or scintigraphy (considered the gold standard) are cumbersome, reducing their clinical usefulness.6–8
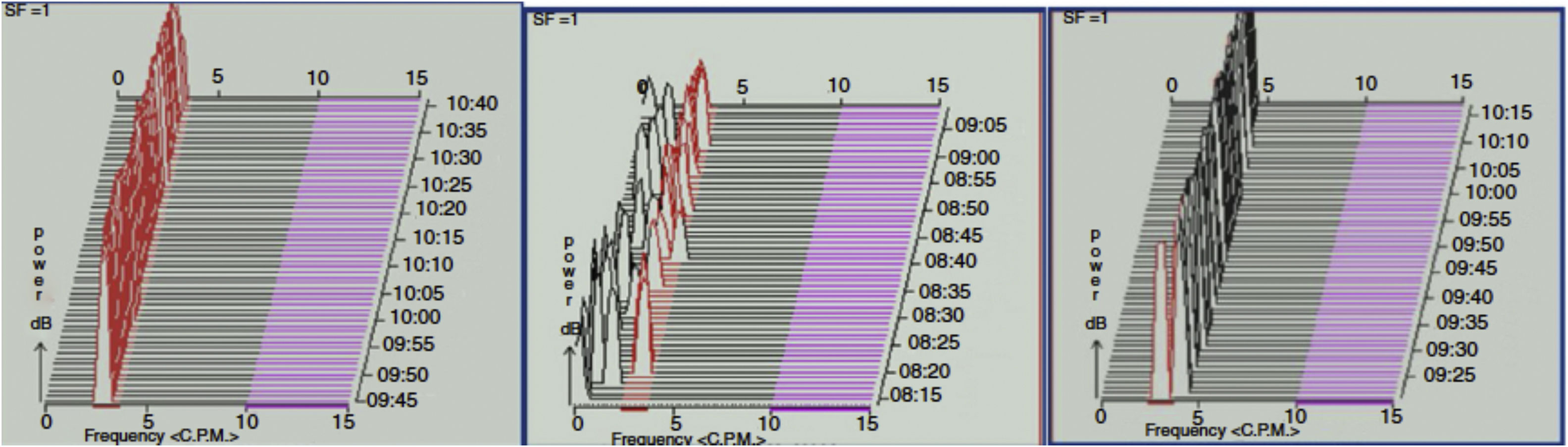
Surface electrogastrography (EGG) is a non-invasive method for measuring gastric electrical activity. Using cutaneous electrodes placed on the abdominal skin over the stomach, EGG records the slow waves generated by the interstitial cells of Cajal in the greater curvature of the corpus, which act as pacemakers. The slow waves are propagated to the antrum and followed by spike potentials, leading to gastric contractions. The normal frequency of gastric slow waves (dominant frequency) in humans is approximately 3 cycles per minute (cpm), with a range of 2.4-3.7. Bradygastria is defined by 0.5 to 2.3 cpm and tachygastria by 3.8 to 10 cpm (fig. 1). EGG recording has consistently proved to represent gastric slow waves, when compared with internal serosal recording. Likewise, EGG correlates with gastric emptying measured through scintigraphy in patients with functional dyspepsia, gastroesophageal reflux, and gastroparesis.9–11 EGG has not been tested in critically ill patients.
The aim of our study was to compare the effects of a single dose of intravenous metoclopramide or domperidone on gastric electrical rhythm in septic patients measured through EGG. The secondary aims were to investigate gastric motility in that group of patients and look for risk factors for dysmotility, assuming a positive correlation between electrical and mechanical activity.
Materials and methodsDesignWe designed a triple-blind randomized study at the intensive care unit (ICU) of the Hospital Clínico Universidad de Chile. Randomization was performed using a free web program (www.randomization.com). The allocation ratio was 1:1. Patients, care providers, and the gastroenterology team were blinded. All the electrogastrograms were performed by one operator (GL) and analyzed by the same gastroenterologist (AMM).
The Ethics Committee of the Hospital Clínico Universidad de Chile approved the study (Record No. 46, October 13, 2010). The patients’ families provided written statements of informed consent.
Participants and eligibility criteriaThe patients included in the study were over 18 years of age and had been admitted to the ICU with the diagnosis of septic shock, as defined in the 2001 Sepsis Definitions Conference report. They were in the post-resuscitative phase, locally defined as mean arterial blood pressure over 70mmHg, needing less than 0.15μg/kg/min of norepinephrine, and had normal clinical and laboratory perfusion state parameters (normal lactate level and central oxygen venous saturation).
We excluded patients that had a history of esophagogastric surgical resection. Other types of abdominal surgery were not an exclusion criterion. We also excluded patients diagnosed with autonomic neuropathy of any etiology, such as long-lasting diabetes. Diabetes mellitus itself and hypothyroidism were not an exclusion criterion. Patients with records of adverse reactions to the study drugs were excluded. In addition, electrocardiograms were performed on all patients to measure the QT interval and those with a prolonged QT were also excluded. A history of arrhythmia unrelated to long QT syndrome was not an exclusion criterion. Finally, we excluded patients who had received prokinetic drugs within the previous 48hours.
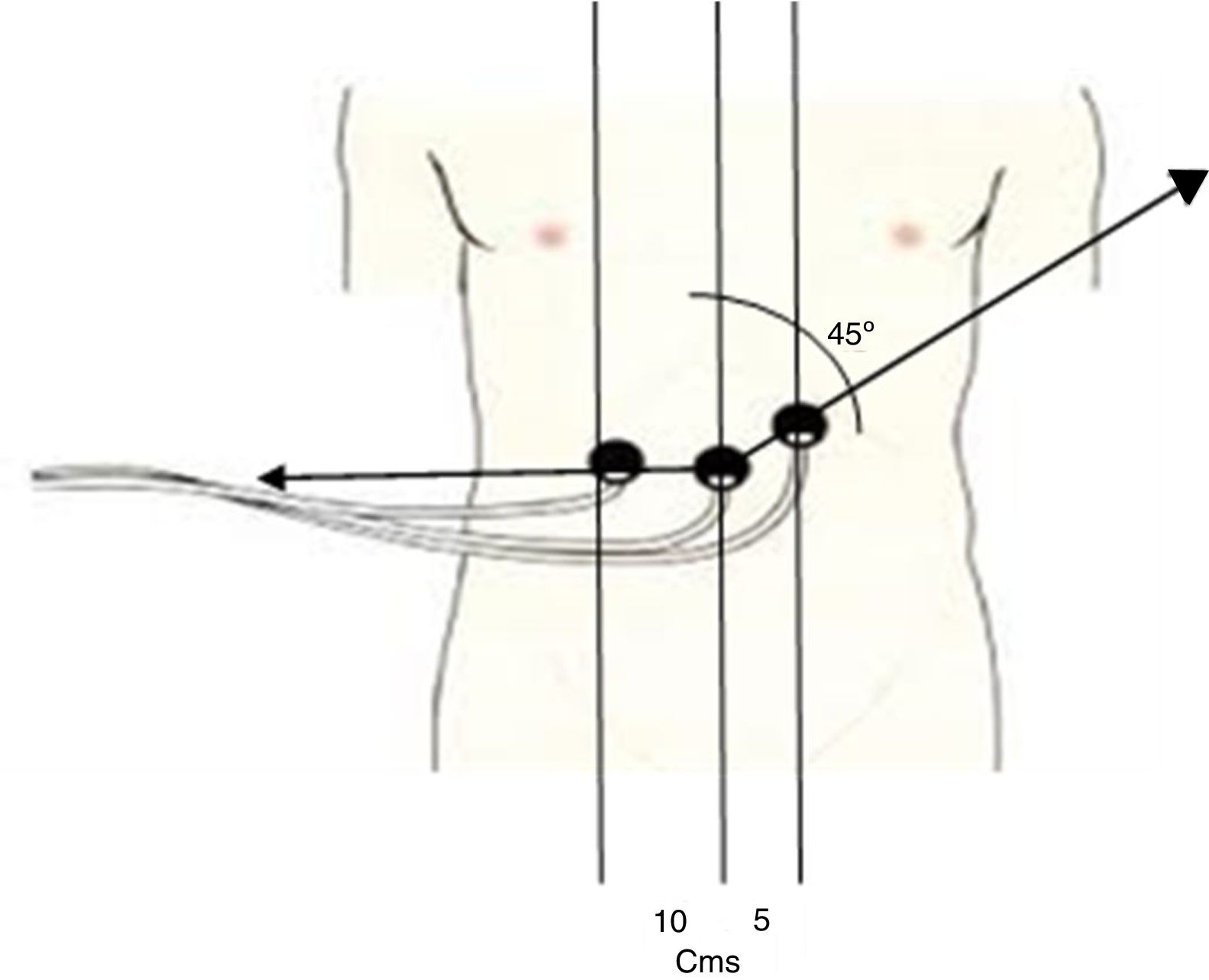
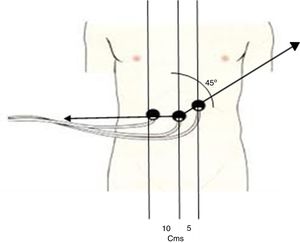
Interventions and measurementsGastric electrical activity was evaluated through EGG. We used a digital HR polygraph (Synectics Medtronic Medical, Sweden) connected to a computer with an analyzer program. The technique includes installation of two bipolar electrodes and one reference electrode. First, the skin is thoroughly cleaned and abraded, and then a conductive gel is applied. The first electrode is placed at the midpoint between the xiphoid process and the umbilicus. The second electrode is placed 5cm to the left of the first one at a 45° angle. The ground electrode is located 10cm to the right of the first electrode (fig. 2). Impedance between electrodes is measured with a tester. If it is over 10 kΩ, the skin is cleaned again.12
Placement of the 3 cutaneous electrodes to register gastric electrical activity. The first electrode is placed at the midpoint between the xiphoid process and the umbilicus. The second electrode is placed 5cm to the left of the first, at a 45° angle. The ground electrode is located 10cm to the right of the first electrode.
The baseline register was carried out with patients in a 45-min fasting state. Afterwards, in a randomized fashion, they received a single dose of 10mg of intravenous metoclopramide or 10mg of intravenous domperidone, diluted in 50ml of saline solution and infused over 20minutes. We registered a post-drug period of 60minutes. It is necessary for patients to be in a quiet state during the exam and not receive medication or nursing or respiratory therapy care, so that there is no interference with the register. Our patients were in the initial phase of septic shock and therefore were in a fasting state. Because our goal was to evaluate the effect of a prokinetic agent, the drug “replaced the meal”, which is standard practice in routine EGG.
As mentioned above, normal gastric slow wave frequency ranges from 2.4 to 3.7 cpm. A study is normal (normogastria) when ≥ 70% of the recording time is in the normal range. If more than 30% of the recording time is outside the normal interval, then the result is dysrhythmia, regardless of the predominance of bradygastria or tachygastria. Both of those abnormalities may lead to dysmotility, and tachygastria is associated with the poorest gastric emptying. Gastric contraction strength was inferred from the dominant power (DP), which is a measure of the amplitude of the slow wave, expressed in μν2. The power ratio (PR) is the relation between the pre-drug DP and the post-drug DP.
A PR > 1 is interpreted as an increase in the strength of contraction and represents the normal response expected after a meal.13
PR = post-drug DP / pre-drug DP
We evaluated dominant frequency (DF), the distribution in time percentage, DP, and PR. Because the data were obtained before and after administration of the study drug, each patient acted as his or her own control.
The aim was to compare the efficacy of metoclopramide and domperidone in improving gastric motility, understood as the ability to restore normogastria (> 70% between 2.4 to 3.7 cpm) or the capacity to increase PR. Secondary aims were to evaluate gastric motility in septic patients and to look for risk factors for impaired gastric emptying.
We collected the following clinical data: sex, age, the Acute Physiology and Chronic Health Evaluation II score (APACHE II), the Sequential Organ Failure Assessment score (SOFA), accumulated fluid balance, and hemodynamic status (norepinephrine requirements, lactate level, and central venous oxygen saturation) and respiratory function (PaO2/FIO2 ratio) parameters. We also evaluated the actual and accumulated dose of sedatives and correlated the data with the electrogastrographic results.
The local sedation protocol was based on the combined use of midazolam and fentanyl, targeted to daily goals of sedation and favoring the use of opiates over benzodiazepines.14 Data were collected upon admission and on the day of the protocol.
Statistical analysisBy estimating that 50% of the patients analyzed presented with gastric dysmotility, a sample size of 72 patients was needed to achieve a statistical power of 80% to detect a 25% positive effect of prokinetic drugs, with α = 0.05. As a pilot study we planned to enroll 50% (www.openEpi.com).
The descriptive data analysis was expressed as mean (SD), median (P25-P75), or percentage, as appropriate for data distribution according to the Kolmogorov-Smirnov test. To evaluate the association between the baseline electrogastrography and possible risk factors for dysmotility, we used the t test or the Mann-Whitney U test. The comparison of efficacy between metoclopramide and domperidone was made through the bilateral unpaired t-test for averages and Fisher's exact test for proportions. We used the paired t-test for the related samples and the McNemar's test for the categorical variables to compare the pre-drug and post-drug dominant frequency and dominant power. Statistical significance was set at a p < 0.05 for all analyses and the SPSS 21.0 software was used to analyze the data.
ResultsA total of 37 patients were enrolled in the study within the time frame of April 2011 to December 2012. One patient agreed to participate and signed a written statement of informed consents, but later refused, leaving a final total of 36 patients (18 males and 18 females). Mean age was 66 years (range 27 to 92 years). All the patients met the criteria for septic shock diagnosis. The site of infection was the abdomen in 24 patients, the lung in 8 patients, the skin in 2, urine in one patient, and the aorta in one patient. Before recruitment, 21 patients (58%) had abdominal surgery. In that group of patients, the exam was performed at a median time of 3 postoperative days.
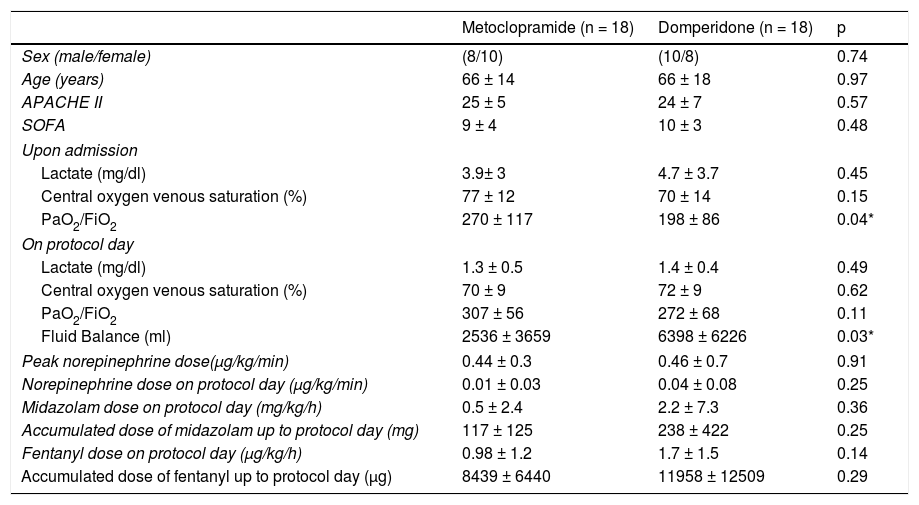
On average, EGG was carried out on the third day after ICU admission (range between 1 to 9 days) in the general group. None of the patients presented with a prolonged QT interval. At the time of EGG, 29 patients (80%) were on invasive mechanical ventilation and 31 patients (86%) had a nasogastric tube. Those facts did not produce an artifact in the registry. There were no problems in relation to the placement of electrodes, given that none of the patients had wounds at the installation site. Eighteen patients received metoclopramide and 18 received domperidone. The demographic and clinical data of both groups are presented in Table 1.
Baseline features of 36 patients with septic shock: 18 patients randomized to metoclopramide and 18 to domperidone.
| Metoclopramide (n = 18) | Domperidone (n = 18) | p | |
|---|---|---|---|
| Sex (male/female) | (8/10) | (10/8) | 0.74 |
| Age (years) | 66 ± 14 | 66 ± 18 | 0.97 |
| APACHE II | 25 ± 5 | 24 ± 7 | 0.57 |
| SOFA | 9 ± 4 | 10 ± 3 | 0.48 |
| Upon admission | |||
| Lactate (mg/dl) | 3.9± 3 | 4.7 ± 3.7 | 0.45 |
| Central oxygen venous saturation (%) | 77 ± 12 | 70 ± 14 | 0.15 |
| PaO2/FiO2 | 270 ± 117 | 198 ± 86 | 0.04* |
| On protocol day | |||
| Lactate (mg/dl) | 1.3 ± 0.5 | 1.4 ± 0.4 | 0.49 |
| Central oxygen venous saturation (%) | 70 ± 9 | 72 ± 9 | 0.62 |
| PaO2/FiO2 | 307 ± 56 | 272 ± 68 | 0.11 |
| Fluid Balance (ml) | 2536 ± 3659 | 6398 ± 6226 | 0.03* |
| Peak norepinephrine dose(μg/kg/min) | 0.44 ± 0.3 | 0.46 ± 0.7 | 0.91 |
| Norepinephrine dose on protocol day (μg/kg/min) | 0.01 ± 0.03 | 0.04 ± 0.08 | 0.25 |
| Midazolam dose on protocol day (mg/kg/h) | 0.5 ± 2.4 | 2.2 ± 7.3 | 0.36 |
| Accumulated dose of midazolam up to protocol day (mg) | 117 ± 125 | 238 ± 422 | 0.25 |
| Fentanyl dose on protocol day (μg/kg/h) | 0.98 ± 1.2 | 1.7 ± 1.5 | 0.14 |
| Accumulated dose of fentanyl up to protocol day (μg) | 8439 ± 6440 | 11958 ± 12509 | 0.29 |
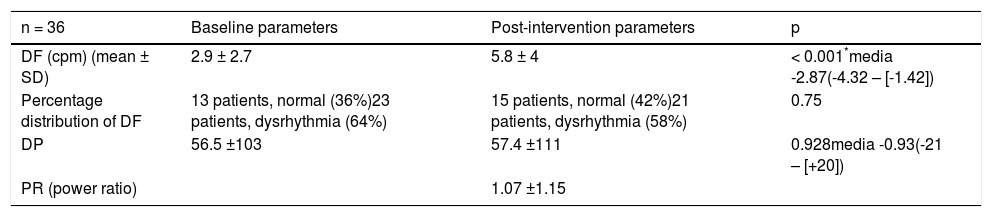
The electrogastrographic features of the total group are described in Table 2. The mean baseline DF was 2.9 cpm. Regarding DF distribution over time, 13 patients (36%) had normogastria and 23 patients (64%) had dysrhythmia. There was an increase in the mean DF to 5.7 cpm (p < 0.05) in the post-drug period, with 42% normogastria and 58% dysrhythmia. In the total group, the baseline mean DP was 56.5μν2 and the post-drug mean DP was 57.4μν2, with a PR of 1.07.
Electrogastrographic findings in the total group. Baseline and post-intervention parameters (infusion of 10mg intravenous metoclopramide/domperidone).
| n = 36 | Baseline parameters | Post-intervention parameters | p |
|---|---|---|---|
| DF (cpm) (mean ± SD) | 2.9 ± 2.7 | 5.8 ± 4 | < 0.001*media -2.87(-4.32 – [-1.42]) |
| Percentage distribution of DF | 13 patients, normal (36%)23 patients, dysrhythmia (64%) | 15 patients, normal (42%)21 patients, dysrhythmia (58%) | 0.75 |
| DP | 56.5 ±103 | 57.4 ±111 | 0.928media -0.93(-21 – [+20]) |
| PR (power ratio) | 1.07 ±1.15 |
DF: Dominant Frequency DP: dominant power
Percentage distribution of DF, defined as normal with > 70% of time between 2.4-3.7 cpm.
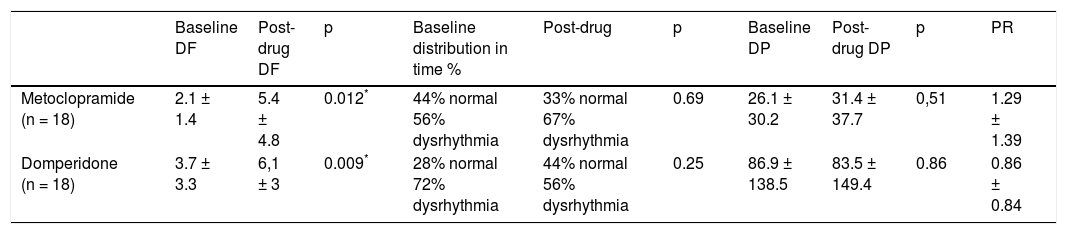
Comparing the efficacy of metoclopramide and domperidone, we found that both drugs significantly increased the DF. In the metoclopramide group, the baseline DF was 2.1 cpm and it increased to 5.4 cpm in the post-drug period. In the domperidone group, the baseline DF was 3.7 cpm and the post-drug DF increased to 6.1 cpm. Although not statistically significant, there was an increase in the proportion of normal studies from 28 to 44% with domperidone, whereas there was a slight decrease in that percentage from 44 to 33% with metoclopramide in the total group. When analyzing each patient as his or her own control, we found that in the metoclopramide group, 3 dysrhythmic patients became normogastric, whereas 4 normogastric patients progressed to dysrhythmia after drug infusion. In the domperidone group, 3 dysrhythmic patients became normogastric and none of normogastric patients became dysrhythmic.
Baseline DP was different in the 2 groups: 26.1μν2 for metoclopramide versus 86.9μν2 for domperidone (p = 0.047). In that scenario, the administration of metoclopramide resulted in a mild increase in the mean DP (34.1μv2) that was reflected in the PR relation (PR = 1.29), whereas domperidone slightly decreased the mean DP (83.5μv2; PR = 0.86) (Table 3).
Electrogastrography results in the metoclopramide and domperidone groups.
| Baseline DF | Post-drug DF | p | Baseline distribution in time % | Post-drug | p | Baseline DP | Post-drug DP | p | PR | |
|---|---|---|---|---|---|---|---|---|---|---|
| Metoclopramide (n = 18) | 2.1 ± 1.4 | 5.4 ± 4.8 | 0.012* | 44% normal 56% dysrhythmia | 33% normal 67% dysrhythmia | 0.69 | 26.1 ± 30.2 | 31.4 ± 37.7 | 0,51 | 1.29 ± 1.39 |
| Domperidone (n = 18) | 3.7 ± 3.3 | 6,1 ± 3 | 0.009* | 28% normal 72% dysrhythmia | 44% normal 56% dysrhythmia | 0.25 | 86.9 ± 138.5 | 83.5 ± 149.4 | 0.86 | 0.86 ± 0.84 |
DF: Dominant Frequency;DP: Dominant Power
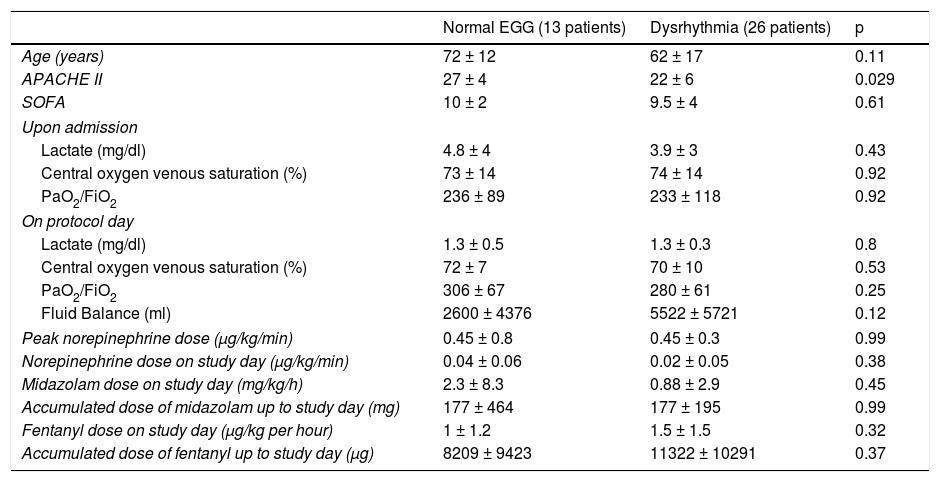
We found no significant correlation between the EGG findings and the baseline features that could be risk factors for dysmotility, although there was a trend to a higher fluid balance and an accumulated dose of fentanyl in patients with gastric dysrhythmia (Table 4).
Correlation between baseline features and EGG (normal or dysrhythmia).
| Normal EGG (13 patients) | Dysrhythmia (26 patients) | p | |
|---|---|---|---|
| Age (years) | 72 ± 12 | 62 ± 17 | 0.11 |
| APACHE II | 27 ± 4 | 22 ± 6 | 0.029 |
| SOFA | 10 ± 2 | 9.5 ± 4 | 0.61 |
| Upon admission | |||
| Lactate (mg/dl) | 4.8 ± 4 | 3.9 ± 3 | 0.43 |
| Central oxygen venous saturation (%) | 73 ± 14 | 74 ± 14 | 0.92 |
| PaO2/FiO2 | 236 ± 89 | 233 ± 118 | 0.92 |
| On protocol day | |||
| Lactate (mg/dl) | 1.3 ± 0.5 | 1.3 ± 0.3 | 0.8 |
| Central oxygen venous saturation (%) | 72 ± 7 | 70 ± 10 | 0.53 |
| PaO2/FiO2 | 306 ± 67 | 280 ± 61 | 0.25 |
| Fluid Balance (ml) | 2600 ± 4376 | 5522 ± 5721 | 0.12 |
| Peak norepinephrine dose (μg/kg/min) | 0.45 ± 0.8 | 0.45 ± 0.3 | 0.99 |
| Norepinephrine dose on study day (μg/kg/min) | 0.04 ± 0.06 | 0.02 ± 0.05 | 0.38 |
| Midazolam dose on study day (mg/kg/h) | 2.3 ± 8.3 | 0.88 ± 2.9 | 0.45 |
| Accumulated dose of midazolam up to study day (mg) | 177 ± 464 | 177 ± 195 | 0.99 |
| Fentanyl dose on study day (μg/kg per hour) | 1 ± 1.2 | 1.5 ± 1.5 | 0.32 |
| Accumulated dose of fentanyl up to study day (μg) | 8209 ± 9423 | 11322 ± 10291 | 0.37 |
We found that gastric dysmotility was prevalent in the group of critical septic patients studied. Sixty-four percent of the patients had abnormal studies, which was higher than that of the healthy volunteers and similar to the previously reported results in dyspeptic and diabetic patients at our hospital.15 Because those patients were already resuscitated in terms of general perfusion, it would be reasonable to speculate that in the active phase of shock the percentage of dysmotility could be even higher. Delayed gastric emptying is common in the ICU. It has been demonstrated by different techniques in about 50% of unselected patients.16,17 The elevated number of patients with impaired gastric motility in our study could also be related to the high percentage of abdominal surgery (58%).
Unlike other studies, we did not find risk factors for impaired gastric emptying among those frequently recognized. As mentioned earlier, our ICU favors the use of opiates for sedation. Opiates act by stimulating the μ receptors, thus diminishing gastrointestinal motility. All our patients received moderately high doses of fentanyl, but statistical significance was not reached, despite the fact that the group with gastric dysrhythmia had a higher accumulated dose of fentanyl than the normal group. In fact, some studies have shown that opiates decrease gastrointestinal motility in a dose-dependent manner, whereas others have not.18–20 Similar results were obtained when analyzing other potential risk factors, such as midazolam or norepinephrine doses. The inverse association found with the APACHE II lacked clinical significance (Table 3). However, the inability to find any relation between clinical risk factors and gastric hypomotility could be explained by the small sample size.
The effect of prokinetics in the ICU has been evaluated in only a few reports and most of them were conducted in the 1990s. Cisapride, metoclopramide, and erythromycin were shown to increase gastric emptying in mechanically ventilated patients.21–23 More recent studies have reported that erythromycin was superior to metoclopramide, and their combination was superior to metoclopramide alone.24–26 Metoclopramide combined with neostigmine decreased the gastric residual volume more efficiently than monotherapy, as well.27
In brief, a recent survey of 13 randomized control trials, involving more than 1,000 patients, concluded that prokinetics significantly improved food tolerance, reduced gastric residual volumes, and increased post-pyloric tube placement with no effects on the length of hospital stay or mortality.28
Domperidone was compared with oral metoclopramide in relation to diabetic gastroparesis in one study and to nausea control associated with chemotherapy in another, demonstrating similar and effective performances.29,30 The only report on critical patients comparing domperidone and metoclopramide showed that both similarly improved the post-pyloric placement of nasojejunal tubes and were superior to placebo.31
However, the mechanism of action of all prokinetic agents is complex. The precise manner in which that type of drug produces the clinical effect on gastric motion is not well understood. Tachygastria can induce gastroparesis in the same way that atrial fibrillation deteriorates atrial contraction. In fact, in patients with dyspepsia associated with reduced gastric emptying, a predominance of tachygastria in the pre and post-prandial phases was found.32
In our investigation, both metoclopramide and domperidone increased the dominant frequency of gastric pacemaker activity. Domperidone demonstrated a slight advantage over metoclopramide, increasing the number of normogastric exams. That finding could be relevant, considering the potential to deteriorate gastric emptying by inducing tachygastria. A bigger sample size could possibly clarify that observation. Changes in the DP in both groups were slight, and most likely without clinical relevance. Nevertheless, the minimal increase in PR is a reflection of severe gastric dysmotility, probably not modifiable by single doses of the drugs analyzed.
The strength of the present study lies in its originality. To the best of our knowledge, this is the first study testing EGG in critical patients, given that the exam is usually prescribed to evaluate outpatients with dyspeptic symptoms. The main advantage of EGG is its non-invasive nature. Moreover, it can be performed bedside, avoiding all difficulties related to patient transfer. One of the major concerns about EGG interpretation is its sensitivity to motion artifacts or electrical interferences. Even though mechanical ventilation and electronic monitoring devices could be sources of interference in the signal, the fact that we obtained a reliable electrogastrogram in all the patients studied, 80% of whom were on invasive mechanical ventilation, demonstrates the feasibility of performing EGG. It is possible that sedation contributed to the high performance of the test, by preventing patient movements.
Considering that ours was an initial experience, once we established the feasibility of performing the exam, we decided to evaluate a simple fact: the effect of a single dose of two prokinetic drugs and their comparison. Intravenous use of domperidone has been approved in Chile for many years and the Public Health Institute registers adverse events. We chose metoclopramide and domperidone because they are routinely used in clinical practice and have a positive safety profile, another novel aspect of our study, given that those two drugs have rarely been analyzed in the intensive care setting. We showed that both drugs had an effect that was clearly demonstrable through EGG, which could be a starting point for more elaborate studies to evaluate clinical outcomes, the effect of multiple doses, or the correlation with gastric emptying. As mentioned above, an increase in dominant frequency does not necessarily mean an improvement in gastric emptying. EGG could help to understand the physiologic phenomenon that underlies the effect of a given drug.33
Flaws of the present study include its small sample size, the lack of a clinical outcome measure, and of course, the persistent question as to the real correlation between EGG and gastric emptying. The correlation between the cutaneous and serosal recording of gastric electrical activity has been well demonstrated. On the other hand, the validity of the exam to represent gastric emptying or reflect a specific disease is still a matter of controversy. Initial studies showed no relation between EGG findings and antral motility measured through manometry or ultrasound.34,35 Most available information comes from studies on dyspepsia and diabetic gastroparesis. In a group of diabetic patients with symptoms of gastroparesis, none of them had a normal EGG pattern, which correlated with abnormal gastric emptying, and an improved post-treatment period with domperidone.36 In a recent study there was a negative correlation between the percentage of normogastria in EGG and gastric retention parameters in SPECT, suggesting that impaired gastric myoelectrical activity could be responsible for the delayed gastric emptying in patients with functional dyspepsia.37 In patients with functional gastroparesis, EGG showed a bradygastric pattern different from patients with mechanical obstruction that presented with a predominant high-amplitude 3-cpm pattern.38 At any rate, a normal EGG does not guarantee normal gastric emptying, but an abnormal pattern can predict anomalous gastric emptying and correlates with symptoms.
ConclusionIn summary, we evaluated the physiologic effect of two prokinetic drugs on gastric electrical activity in the present study and found that metoclopramide and domperidone similarly increased the dominant frequency of gastric pacemaker activity. Because surface electrogastrography is not a direct measure of gastric emptying, the translation of that finding into clinical effects has yet to be determined. It is possible that domperidone exerts an additional beneficial effect by improving the pattern of gastric slow waves, increasing normogastric time. Neither of the drugs had a significant effect on the strength of contraction. Reanimated septic patients have an elevated proportion of gastric motility impairment that does not seem to be associated with the severity of hemodynamic or respiratory impairment or with sedative dosage. EGG is a feasible exam in critically ill, ventilated patients and its results are abnormal in most of those patients.
Ethical disclosuresProtection of persons and animalsThe authors declare that the procedures followed conformed to the ethical standards of the responsible committee on human experimentation and were in accordance with the World Medical Association and the Declaration of Helsinki.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Financial disclosureThis project received funding from the Internal Office for Clinical Investigation of the Clinical Hospital, Universidad de Chile, OAIC Project 426/10.
Conflict of interestAll the authors declare that there are no conflicts of interest.
The authors wish to thank Jorge Ordenes, electrical engineer at the Faculty of Medicine of the Universidad de Chile and José Matus (†) for their invaluable help in carrying out the exams.
Please cite this article as: Mancilla Asencio C, Gálvez-Arévalo LR, Tobar Almonacid E, Landskron-Ramos G, Madrid-Silva AM. Evaluación de motilidad gástrica mediante electrogastrografía de superficie en pacientes críticos sépticos. Comparación de los efectos de metoclopramida y domperidona: un ensayo clínicopiloto aleatorizado. Revista de Gastroenterología de México. 2019;84:149–157.