Resection is the only therapy with curative intent for intrahepatic cholangiocarcinoma (ICC). Extended left hepatectomy is technically complex and demanding. Important factors for its success are adequate interpretation of preoperative images, identification of the section plane, and the prevention of biliary complications. We present herein the case of a female patient with inferior vena cava (IVC) malformation, who required extended left hepatectomy due to ICC.
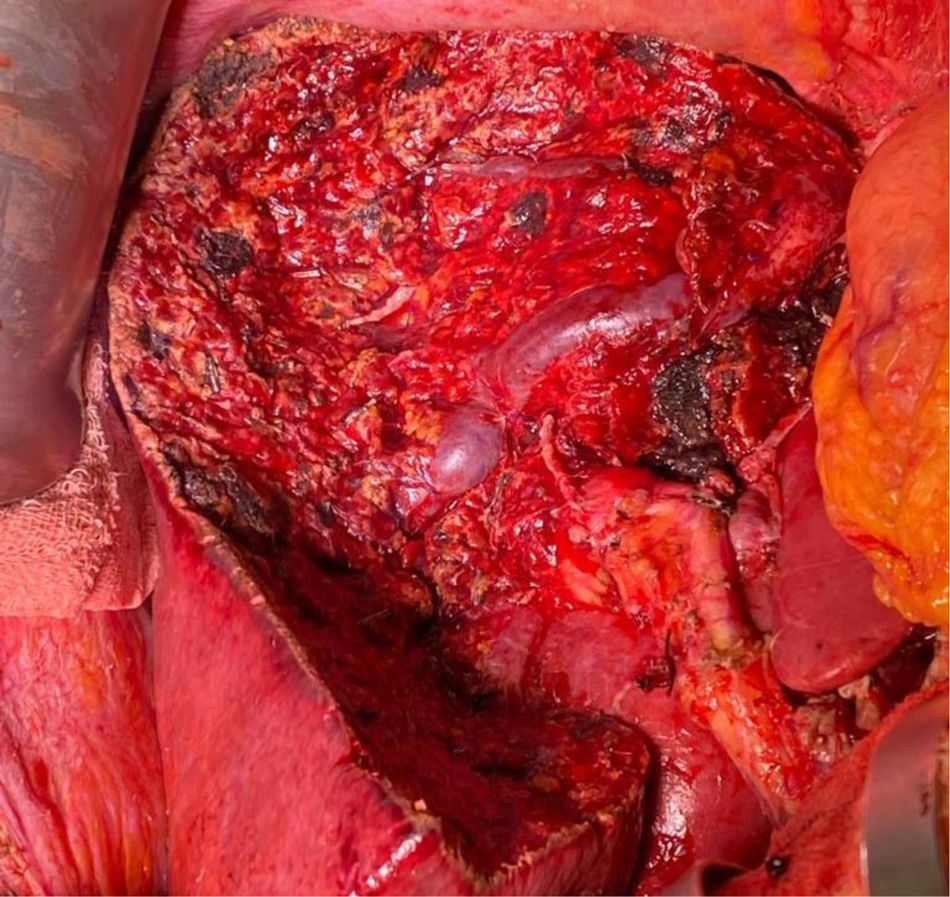
A 50-year-old woman presented with epigastric pain of 5-month progression. Surgical evaluation revealed a palpable liver lesion. Laboratory test results were normal, with a carbohydrate antigen (CA) 19-9 level of 84 IU. Images with contrast showed an 11cm lesion with peripheral enhancement (segments 3, 4, 5, 6, and 8), with a 2.8cm S8 nodule and a 1.5cm S4 nodule (Fig. 1). A double IVC with bilateral azygos continuation was identified and the absence of a retrohepatic segment was confirmed through venography (Fig. 2). Extended left hepatectomy was planned, respecting the two anomalous lateral branches of the right IVC, as well as S1. Abnormal affluents carried out liver drainage into the inferior phrenic veins (Fig. 3). The patient was discharged 10 days after the intervention with no complications (Fig. 4). The pathology study reported multifocal ICC with focal extension into the hilar fat, left portal blockage, microvascular and perineural invasion, negative lymph nodes (N0), and a positive microscopic vascular margin (R1v). The patient received adjuvant chemotherapy. Nine months after the surgery, she had intrahepatic and extrahepatic disease recurrence. Chemotherapy was started and the patient died 2 years later.
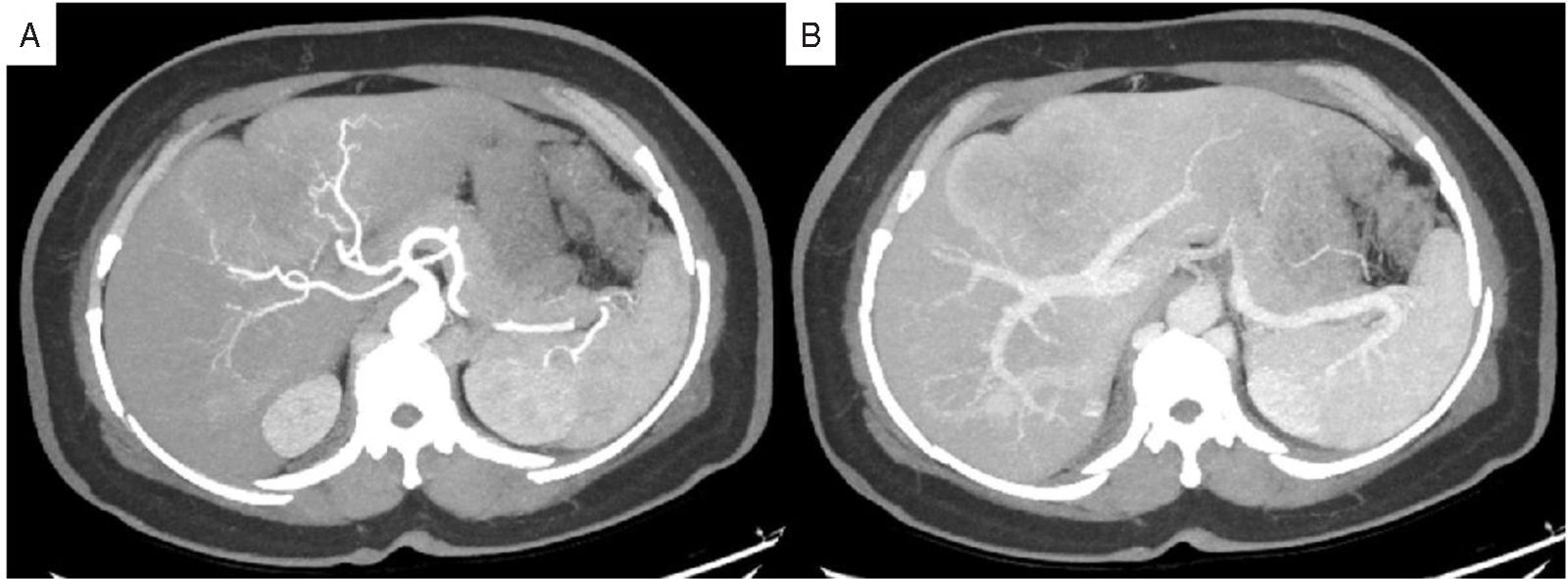
(A) Axial contrast-enhanced computed tomography maximum intensity projection images in the arterial phase, showing a large lesion with peripheral enhancement and a replaced right hepatic artery emerging from the superior mesenteric artery. An A3' artery emerged from the left gastric artery (not shown). (B) Axial contrast-enhanced computed tomography maximum intensity projection images in the portal phase, showing a lesion blocking the pars umbilicalis of the left portal vein.
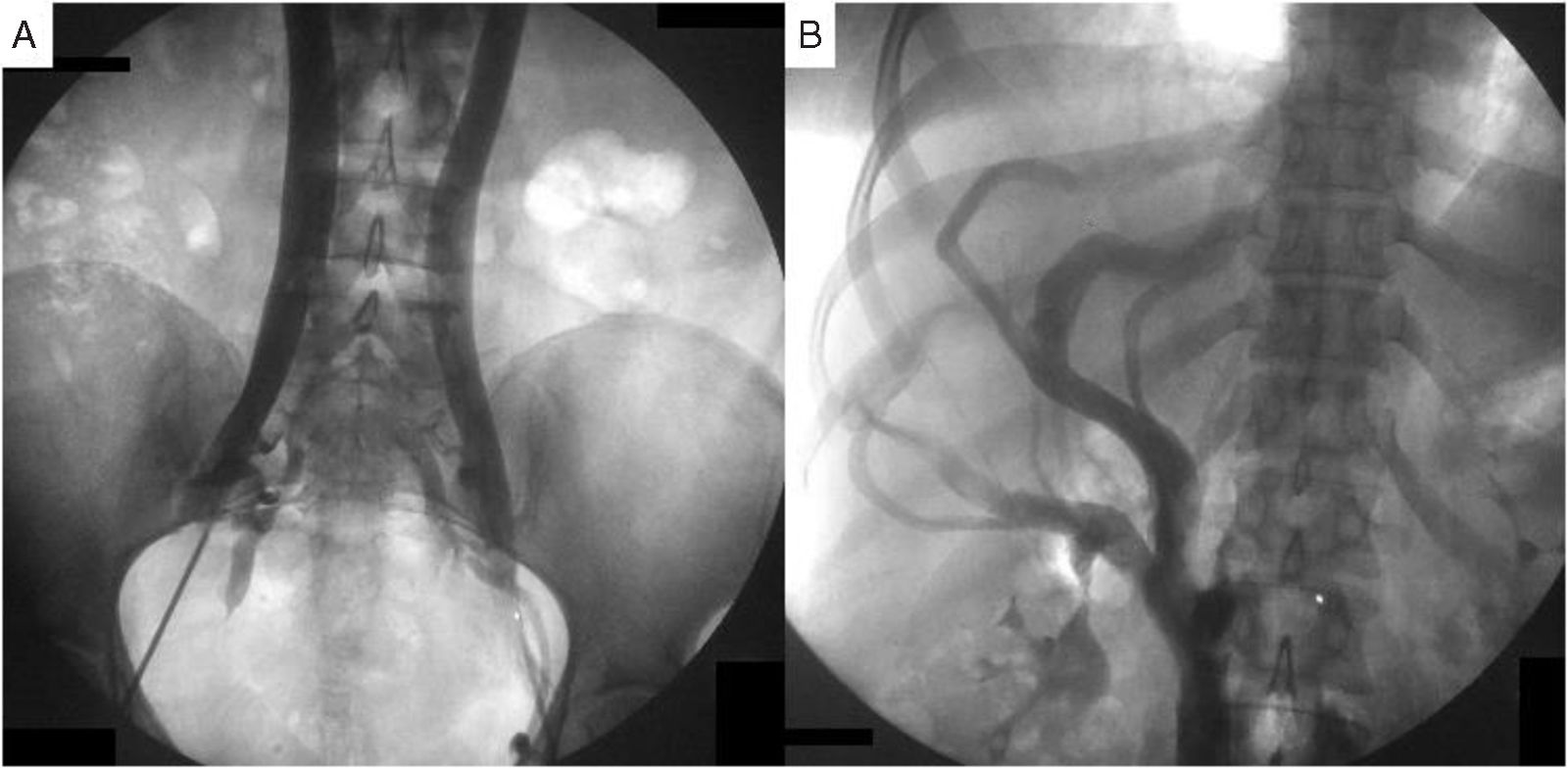
Cavography through bilateral femoral access, showing the completely duplicated inferior vena cava (IVC) (A) with bilateral azygos continuation and no retrohepatic segment. There were 3 branches of the right IVC (B). The 2 lateral branches crossed the liver and drained the right hepatic vein. The medial branch continued under the right pillars of the diaphragm, as the right azygos vein.
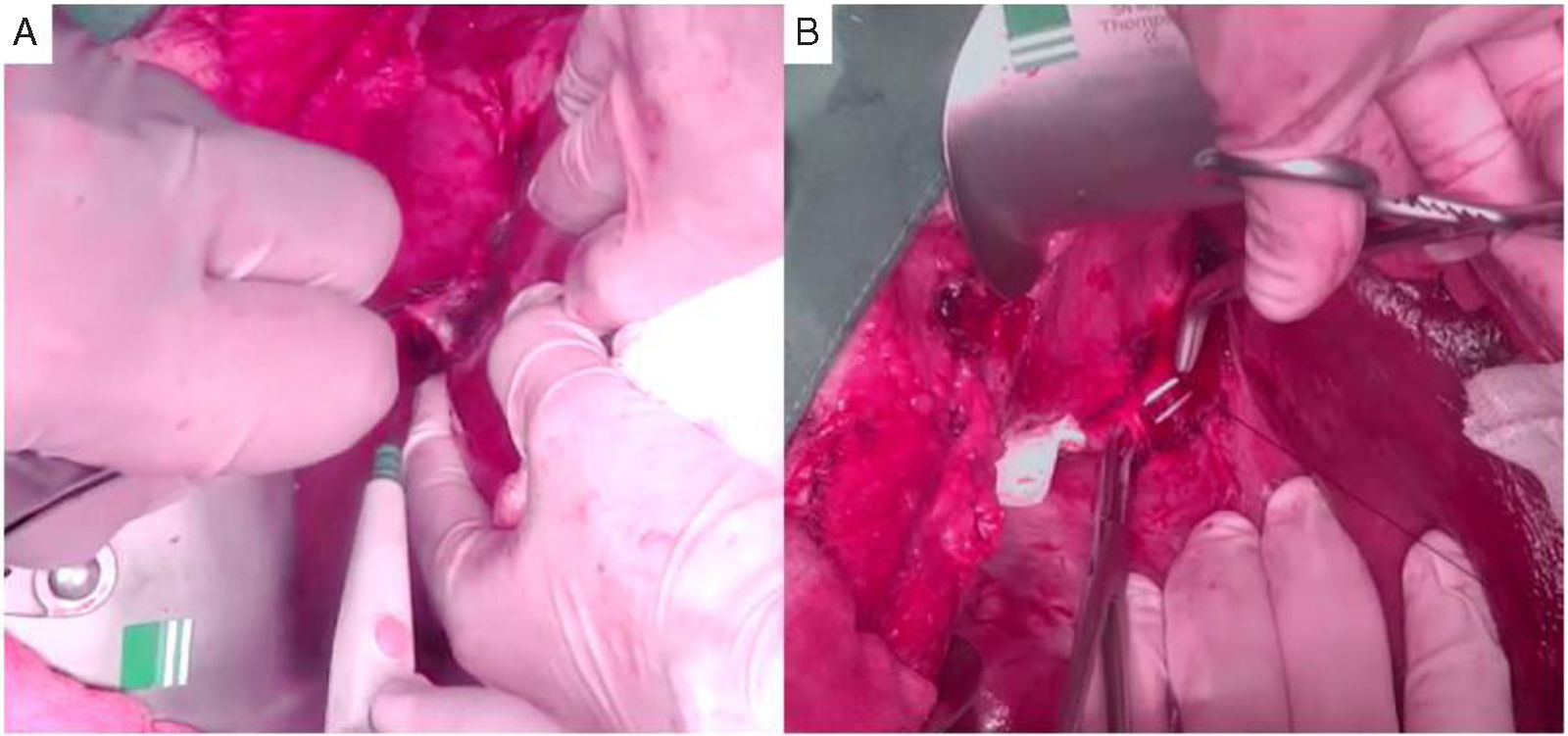
After removing the specimen, the abnormal right hepatic vein was completely skeletonized. Segments 1, 6, and 7 were preserved. The left bile duct was ligated (the stump of the left portal vein is seen behind it) and the right anterior hepatic duct was divided with a stapler. The intraoperative cholangiography (the left inferior small panel) shows the permeability of the right posterior hepatic duct.
The patient’s family signed a statement of informed consent for the anonymous publication of her case.
This work meets the current bioethical research regulations and was authorized by the ethics committee of the Centro Médico Naval for publication.
The authors declare that this article contains no personal information that could identify the patient.
Financial disclosureNo financial support was received in relation to this article.