Turner syndrome (TS) is a genetic disorder that affects females and can present with various medical conditions.
A 42-year-old woman with TS had a history of anemia and episodes of gastrointestinal (GI) bleeding, starting at 3 years of age. In one episode of GI bleeding during infancy, the patient underwent exploratory laparotomy that revealed multiple dilated vessels that appeared to be capillaries, in the mesentery and small bowel serosa, impeding any attempt at resection. Her anemia was managed with vitamin supplements. TS was diagnosed later, and hormonal therapy was started when she was 11 years old. Celiac disease was diagnosed when the patient was 37 years old.
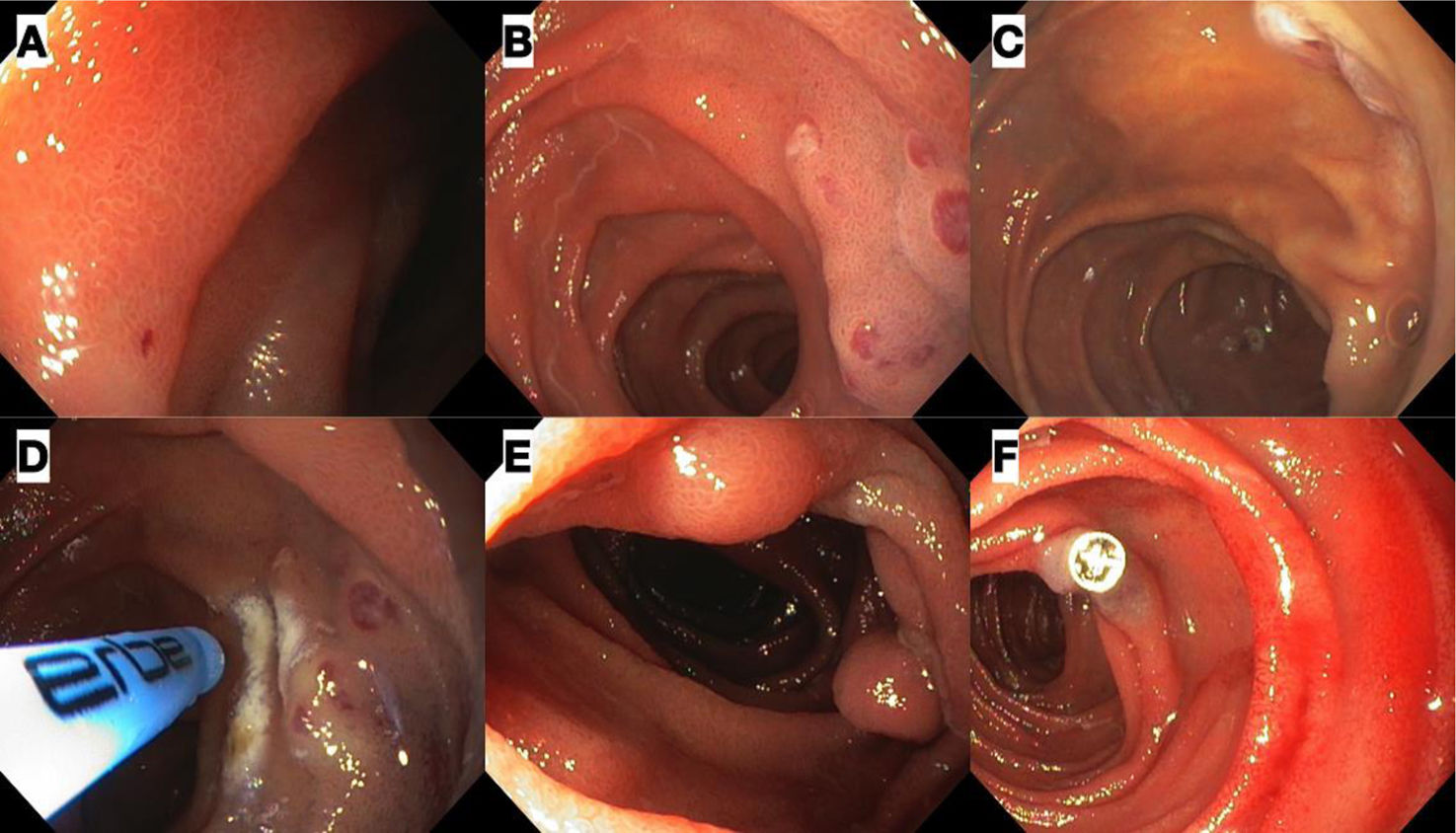
She was admitted to the emergency service with profuse melena and severe microcytic-hypochromic anemia, with a hemoglobin level of 3.5 g/dl. Liver function tests were normal and anti-tissue transglutaminase testing was negative. The patient rejected the use of blood products and so was managed with intravenous iron (1,000 mg of ferric carboxymaltose) plus subcutaneous epoetin alfa (4,000 IU/day for 10 days). Neither esophagogastroduodenoscopy (EGD) nor initial colonoscopy revealed the origin of the bleeding. The endoscopies were repeated at our center, identifying a prominent submucosal vascular network in the duodenum, terminal ileum, and colon, with no active bleeding (Fig. 1A-E). Computed tomography (CT) angiography was normal. Video capsule endoscopy (VCE) revealed multiple small bowel angiodysplasias and phlebectasias (Fig. 1F). Anterograde deep enteroscopy with a single balloon showed distal angiodysplasias and phlebectasias, with red dots, in the jejunum, that were treated using argon plasma coagulation (APC) (Fig. 2A-D). Endoscopic clips were installed in one of the dilated vessels due to bleeding (Fig. 2E and F). Patient progression was favorable, with no new bleeding episodes. Upon her discharge, the patient’s hemoglobin level was 8.5 mg/dl; it was 13.5 mg/dl at the follow-up at three months.
Esophagogastroduodenoscopy, colonoscopy, and video capsule endoscopy (VCE) images showing vascular abnormalities. (A) Prominent submucosal vascular network in the duodenal bulb. (B) Phlebectasias in the second part of the duodenum. (C) Prominent submucosal vascular network in the terminal ileum. D) Phlebectasias in the transverse colon. (E) Prominent submucosal vascular network in the colon. F) The VCE image shows a small angiodysplasia with no active bleeding.
Single balloon-assisted anterograde deep enteroscopy images. (A) Small angiodysplasia in the duodenum. (B) Phlebectasias in the distal jejunum. C) Phlebectasia in the jejunum. (D) Therapy with argon plasma coagulation. E) Multiple subepithelial lesions throughout the jejunum, corresponding to phlebectasias. (F) During the procedure, one of the lesions described began to have active bleeding, which was successfully stopped with the placement of a clip.
TS is a chromosomal anomaly that affects 1/2,000 live-born female neonates and diagnosis is made at a mean age of 15 years.1 The syndrome is characterized by a partial or complete absence of the second X chromosome, causing several clinical manifestations, such as short stature, infertility and congenital malformations, lymphedema, ovarian insufficiency, and cardiovascular, digital, and renal anomalies, among others.2,3
Regarding GI manifestations, patients with TS experience alterations in liver function, reported in 50-80% of cases, celiac disease (8%), and inflammatory bowel disease (IBD) (2-3%).3 Risk for anemia is three times higher than in the general population, mainly because of iron deficiency due to low intake, malabsorption, or GI bleeding.1 The presence of anemia and visible GI bleeding leads to the suspicion of IBD as a first possibility, given that patients with TS have a 30-times higher risk for ulcerative colitis and a 16-times higher risk for Crohn’s disease.4
GI bleeding due to vascular anomalies in TS has not been widely studied and is mainly described in case reports. Such patients can experience GI bleeding episodes in their first years of life, most likely due to low estrogen levels. Hormone therapy and vitamin supplements can help, but in severe cases, there can be massive bleeding and even death. Patients with TS have a 3.1-times higher mortality rate due to GI bleeding.1 A review of GI vascular malformations in TS showed a variable clinical course, ranging from asymptomatic patients (9%) to patients with visible bleeding, presenting as hematochezia (40%) and melena (38%), along with the common finding of iron-deficiency anemia (87.5%). Vascular abnormalities can appear along the entire intestine and in the mesentery, with a preference for the small bowel.5 Estrogen deficiency is presumed to be involved in the vascular malformations by potentiating blood clotting with ectasia in the microcirculation, as well as directly damaging the endothelium of the anomalous vessels.6 It should be mentioned that the majority of published reports are from before the year 2000, when the diagnosis was made mainly through laparotomy.5
The development of techniques for examining the small bowel allows us to locate and effectively treat bleeding sites. The initial evaluation should include EGD and colonoscopy. If their results are negative, VCE is suggested for hemodynamically stable patients. CT enterography and/or magnetic resonance imaging should be performed when the possibility of capsule retention is suspected. Depending on the VCE findings, deep enteroscopy can be carried out.7,8 CT angiography is recommended in hemodynamically unstable patients, to attempt to locate the origin of the bleeding and eventually guide the embolization through angiography.7–9
The medical management of bleeding due to GI vascular lesions in TS corresponds to estrogen use.10 Somatostatin analogs, thalidomide, tranexamic acid, and vascular endothelial growth factor-neutralizing antibodies are other alternatives, but significant evidence of their efficacy is lacking.11
Endoscopic therapy with APC is the most widely employed treatment in angiodysplastic lesions. Sclerotherapy and clips have also been shown to be beneficial in such cases.12 However, no long-term follow-up of patients who underwent endoscopic therapy is reported in the literature. The efficacy of APC in the small bowel is controversial in the general population, given that, according to a meta-analysis on the subject, the estimated pooled rebleeding rate was 43% in patients with small bowel angioectasias after endoscopic treatment.12 Surgery with or without intraoperative enteroscopy is considered in cases of refractory bleeding or when endoscopic access is not possible.13
Our patient had multiple vascular anomalies in the mucosa, mesentery, and serosa that were successfully treated through emergency endoscopy and iron and estrogen support. Such patients have a higher risk for morbidity and mortality and require targeted study to minimize unnecessary procedures and maximize therapeutic yield.
Author contributionsFC: research and original draft-writing; LG: concept and supervision; PG: original original draft-writing; PT: performance of the endoscopic procedures and photos, and validation and supervision of the manuscript; PM: concept and supervision.
All the authors participated in the manuscript’s final writing, review, and editing.
Financial disclosureNo financial support was received in relation to this article.
The authors wish to thank all of our medical students at the Hospital Clínico de la Universidad de Chile.