Ascites is a common reason for consultation in hepatology and can be the first manifestation of cirrhosis of the liver, its most common etiology.1 There are other less frequent causes of ascites due to portal hypertension, and so the correct differential diagnosis is essential. Malignant infiltration of the liver is one of those causes. It is a rare situation that can cause portal hypertension syndrome complications due to tumor involvement of the small intrahepatic portal branches. An accurate diagnosis must be made to ensure the correct therapeutic approach.1
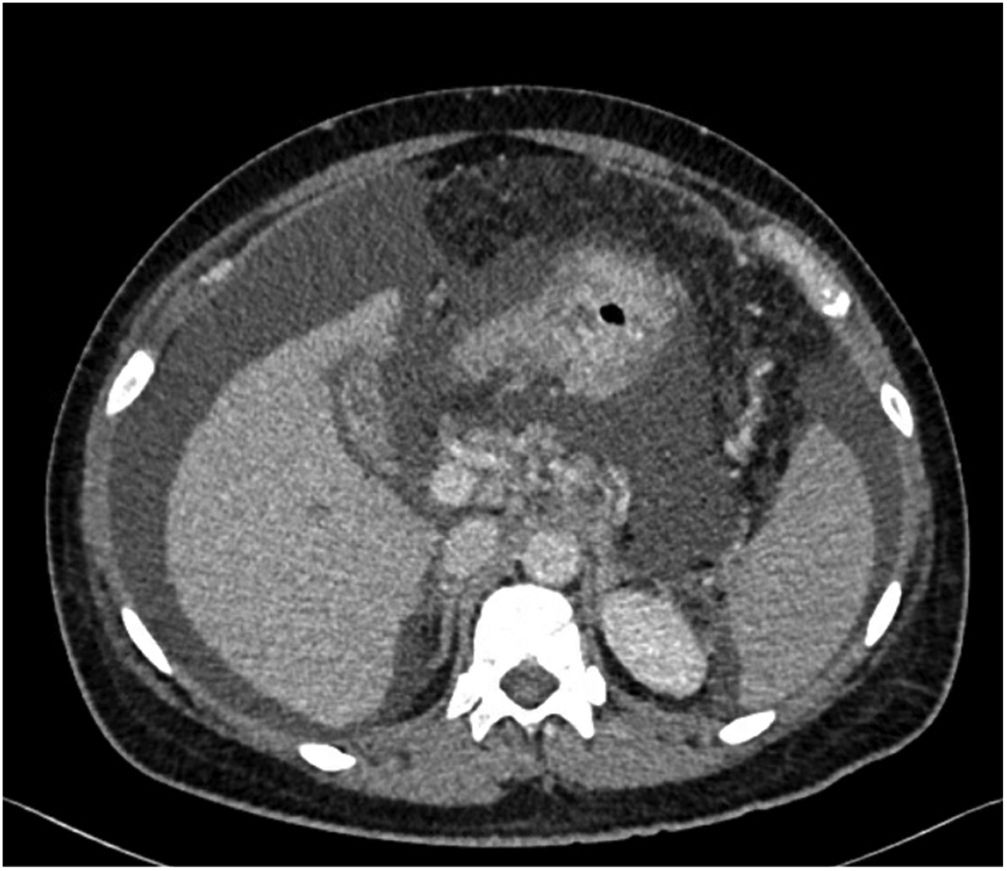
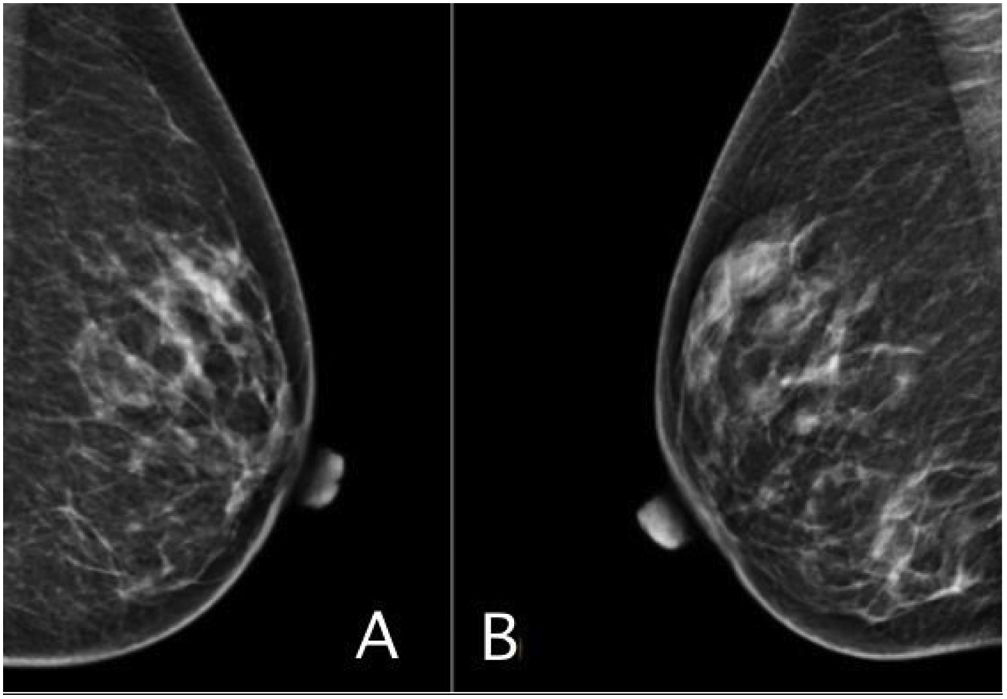
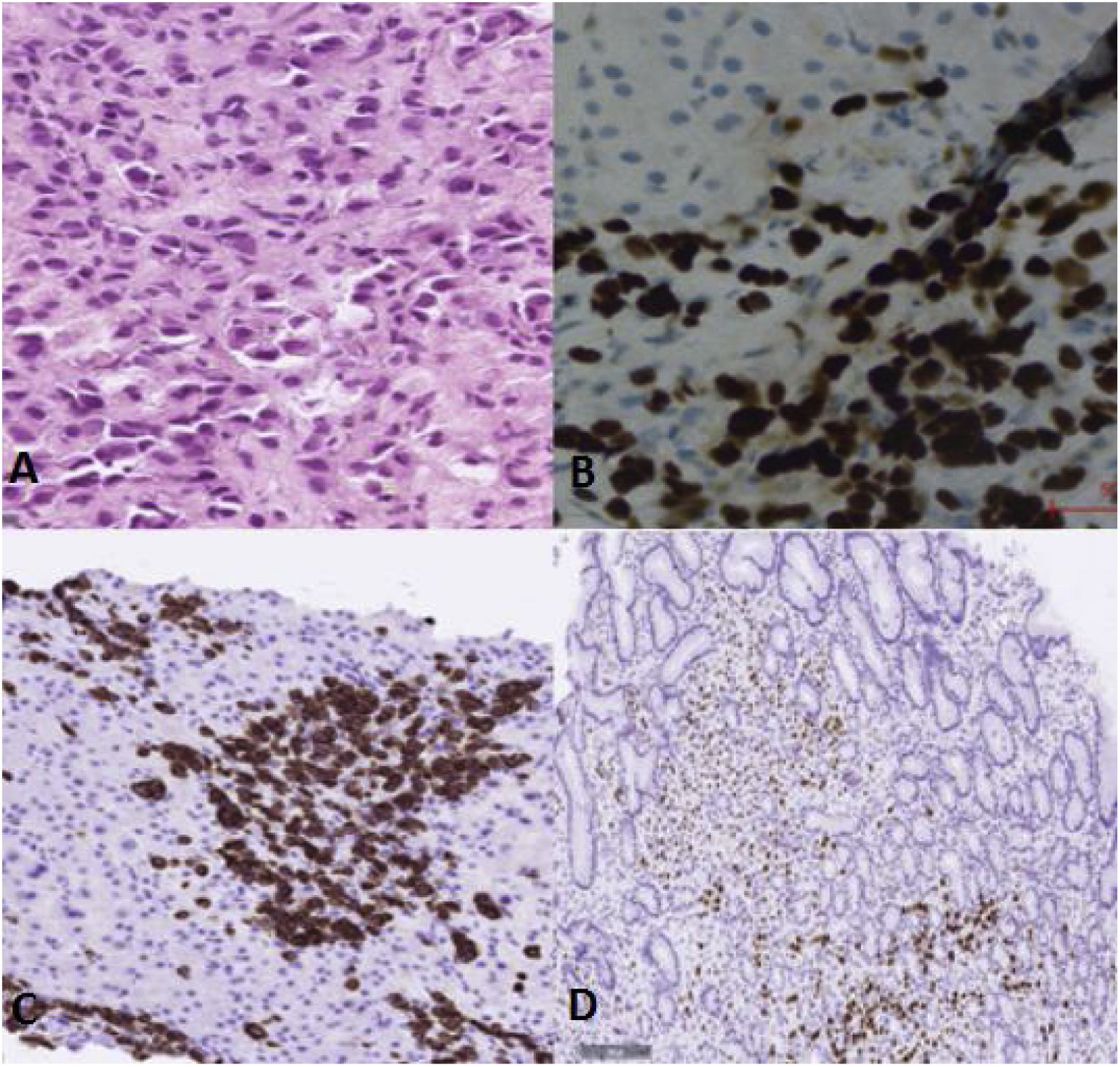
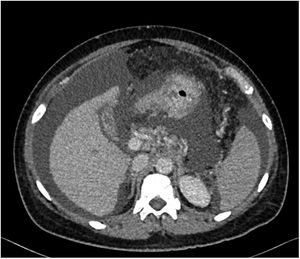
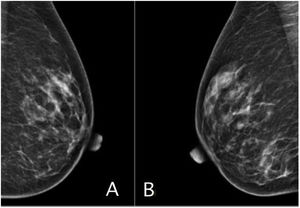
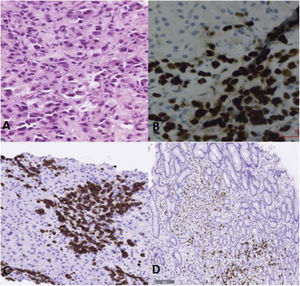
A 56-year-old woman with no relevant toxic habits or pathologic medical history was admitted to our service due to a first episode of ascites. Ascitic fluid analysis showed a cell count of 271 predominantly mononuclear cells (61% lymphocytes, 37% macrophages), with a serum-ascites-albumin gradient (SAAG) of 2.4. Liver function tests revealed a mixed pattern (ALP 304U/l, GGT 220U/l, ALT 169U/l, AST 401U/l, bilirubin 3.2mg/dl, and direct bilirubin 1.7mg/dl), a prothrombin rate of 55%, and 94,000 platelets. The remaining biochemical tests were normal. Hepatopathy analyses were negative for hepatotropic viruses and autoimmune liver disease, and alpha-1-antitrypsin and ceruloplasmin were normal. Gastroscopy revealed the presence of a small esophageal varix at the distal level and important thickening of gastric folds, which were then biopsied. An abdominal computed tomography (CT) scan identified marked signs of portal hypertension (splenomegaly, collateral circulation, abundant free fluid), with no alterations at the level of the liver parenchyma, but with diffuse bone involvement based on multiple punctiform sclerotic lesions (Fig. 1). A PET–CT scan showed no hyperenhanced peritoneal nodules. Tumor markers were elevated, especially CA 15-3 (17,900), suggesting breast disease. A mammogram was carried out and was normal (BI-RADS 1) (Fig. 2A and B). Given the discordant findings between liver disease and tumor pathology, a bone marrow biopsy and transjugular liver biopsy, with hemodynamic analysis, were carried out, obtaining a hepatic venous pressure gradient of 34mmHg. The pathologic anatomy reports of the liver, gastric, and bone marrow biopsies stated diffuse infiltration by neoplastic epithelial cells that were immunohistochemically positive for GATA-3, estrogen receptors, and cytokeratin 7, consistent with metastasis due to invasive lobular carcinoma (Fig. 3A–D). In the liver biopsy, the parenchymal architecture was preserved but there was marked invasion of the portal vein and periportal sinusoid spaces by those tumor cells. While waiting for the oncologic evaluation, to start systemic treatment, the patient had a seizure, followed by cardiorespiratory arrest, from which she recovered with intensive care unit support. An emergency head CT scan showed increased soft tissue in both intraconal spaces, suggestive of tumor infiltration. The patient died within a few hours.
Axial abdominal CT image with intravenous contrast enhancement. Indirect signs of portal hypertension can be seen (collateral circulation with perisplenic and perigastric varices, mild splenomegaly, important hydropic decompensation, with abundant ascites in all compartments), with a homogeneous liver parenchyma showing no signs of advanced chronic liver disease or focal lesions.
Histologic images of the liver and stomach biopsies (×20). (A) Liver biopsy slide with hematoxylin and eosin stain, showing a diffuse infiltrate of neoplastic cells at the level of the portal vein and periportal sinusoid spaces. (B) Liver biopsy slide with immunohistochemistry techniques, showing infiltration into the liver parenchyma by tumor cells positive for GATA-3. (C) Liver biopsy slide with immunohistochemistry techniques, showing infiltration into the liver parenchyma by tumor cells positive for cytokeratin 7. (D) Stomach biopsy slide with immunohistochemistry techniques, showing infiltration into the gastric mucosa by tumor cells positive for estrogen receptors.
Invasion of the liver sinusoids by the hematogenic dissemination of solid tumors, such as breast cancer, accounts for a small percentage of cases of malignant ascites, typically presenting a SAAG>1.1 and negative cytology. Even though the metastatic pattern of said tumors are usually made up of intraparenchymal nodules, diffuse vascular invasion is possible. That type of invasion causes the increase in portal pressure, with consequent complications, such as that of ascites.2,3 Unlike the habitual patterns of liver metastases shown by radiologic studies, this type of diffuse metastatic invasion is not typically detected, resulting in the need for histologic study, to make the correct diagnosis.
In the lobular subtype of breast cancer, there is frequently no macroscopic solid lesion in the breast; it is the neoplastic cells that infiltrate other organs, disseminating through the blood stream, thus hindering their detection.4 Immunohistochemistry carried out on distant lesion acquires special relevance in those cases, enabling the tumor line and primary location of tumors of unknown origin to be defined, which is an essential aspect for providing specific treatment.5
Our case is exceptional because it describes ascites due to portal hypertension associated with diffuse infiltration of the liver, the first manifestation of an unknown lobular breast cancer, normal mammogram, no evidence of peritoneal involvement, and diffuse infiltration to several organs. To the best of our knowledge, this report is the first such case described in the literature, and thus, can contribute to the differential diagnosis of ascites.
Ethical considerationsInformed consent was not requested for the publication of this case because the present article contains no personal data that can identify the patient.
The authors declare that this article contains no personal information that can identify the patient.
Authorization by the ethics committee of our hospital was not required, given that this is a clinical case that involved no research study, and the same therapeutic plan was carried out at all times, with no modifications.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Muíño-Domínguez D, Martín-Sanz J, Celada-Sendino M, Meijide-Santos G, Álvarez-Navascués C. Infiltración hepática por carcinoma lobulillar de mama. Una causa infrecuente de ascitis por hipertensión portal. Rev Gastroenterol Mex. 2023;88:441–443.