There are cases of biliary strictures that are difficult to manage through conventional methods. Intraluminal radiofrequency ablation (RFA) is a novel treatment modality that has been used in cases of malignant biliary strictures and in some cases of benign biliary strictures.1
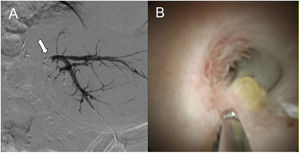
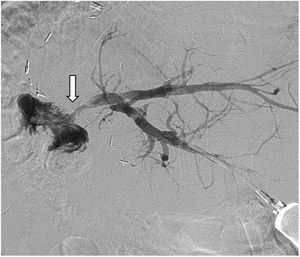
A 69-year-old man had a past medical history of perihilar cholangiocarcinoma (Bismuth IIIa classification) and underwent extensive right hepatectomy with segmental resection of the portal vein and biliary reconstruction through Roux-en-Y hepaticojejunal anastomosis. One year after the procedure, he presented with the complication of biliary-enteric anastomotic stricture, manifesting as episodes of recurrent cholangitis. The patient was first managed through multiple sessions of percutaneous transhepatic balloon dilation and the placement of percutaneous biliary drains. Despite the initial success of those interventions, biliary-enteric anastomotic stricture continued to recur. After discussing the case with a multidisciplinary team, intraluminal RFA was considered a management alternative for said refractory stricture. Under anesthesia with orotracheal intubation, percutaneous transhepatic cholangiography was performed to locate the stricture site and percutaneous transhepatic cholangioscopy was carried out, using SpyGlass™ DS, which was advanced under direct vision, taking biopsies, to rule out neoplastic recurrence (Fig. 1A and B). The biliary drainage catheter the patient previously had was a 12 Fr catheter and did not require dilations. In the same procedure time, a 0.035”/260 cm hydrophilic guidewire was advanced until reaching the stricture. An 8 Fr Habib™ EndoHPB catheter, with two distally placed electrodes, was then advanced over the guidewire. Once the correct position of the electrodes over the stricture site was corroborated through fluoroscopy, RFA was carried out, with no complications. The energy configuration in the generator was 10 watts, with a duration of 90 s. The patient was already receiving antibiotics due to suspected acute cholangitis. The histopathologic result of the biopsies reported only chronic inflammatory changes. In a later control cholangiography, a patent anastomosis was observed, and so the percutaneous biliary drain was removed (Fig. 2). At 10 months from management, the patient has had no recurrences of biliary-enteric anastomotic stricture.
(A) Percutaneous transhepatic cholangiography prior to intraluminal RFA, in which no passage of the contrast agent to the intestinal segment, through the biliary-enteric anastomotic stricture, is observed (arrow). (B) Spyglass™ image of the biliary-enteric anastomotic stricture, with biopsies taken with SpyBite™.
Biliary-enteric anastomoses are performed to re-establish bile duct continuity with the small bowel in surgeries, such as pancreatoduodenectomies, liver transplants, and biliary repair surgeries. Stricture of the biliary-enteric anastomosis is considered an uncommon complication of the procedure and is reported to occur in 2%–11.9% of cases. Those strictures are mainly caused by fibrotic changes in the anastomosis or by tumor recurrence, and can lead to episodes of cholangitis, choledocholithiasis, and cirrhosis.2–4 Due to the complexity of those cases, they should be evaluated in conjunction with a multidisciplinary team. Bile duct reconstruction surgeries for managing biliary-enteric anastomotic strictures are very complex, thus other treatment alternatives should first be considered. Endoscopic management is regarded as a first-line option because it is less invasive. However, it has a lower success rate in biliary-enteric anastomotic stricture, compared with other types of bile duct strictures because of the difficulty in accessing the site of the anastomosis due to anatomic modifications resulting from the surgery and the fact that said strictures tend to be very narrow.4–6 When performed by experienced personnel, the success of endoscopic retrograde cholangiopancreatography (ERCP) through enteroscopy is comparable to that of percutaneous biliary drain placement.7 Endoscopic ultrasound-guided biliary drainage through the creation of a hepaticogastrostomy is another treatment modality, but there is little experience with that approach.8 Due to the disadvantages of the abovementioned treatments, interventional radiology tends to be employed to treat biliary-enteric anastomotic strictures, carrying out balloon dilations through a percutaneous access point and percutaneous biliary drain placement.9
RFA utilizes thermal coagulation to achieve tissue destruction, by applying the energy through a bipolar electrode. RFA is used in various gastroenterology procedures, including biliary strictures. There is still little available evidence of its efficacy in biliary-enteric anastomotic stricture. In a study that involved patients with biliary-enteric anastomotic strictures that were refractory to conventional management, percutaneous biliary drain removal was possible in all the cases that had RFA.1 The application of RFA on normal bile duct tissue increases the risk for perforation and bleeding, which is why cholangioscopy can help us prevent those complications by accurately identifying the affected segment6; in our patient, it also helped rule out tumor recurrence. The procedure is costly and not yet widely available, and experience in ERCP and cholangioscopy is also required.
In conclusion, biliary-enteric anastomotic strictures can sometimes be refractory to first-line treatments. Fortunately, we have numerous types of interventions that can be considered in such cases, and the novel modality of intraluminal RFA is one of them.
Ethical considerationsThe authors declare that they followed the bioethical protocols of their work center, regarding patient data publication. Given the type of article, evaluation by an ethics committee was not required. The authors declare this article contains no personal patient information, informed consent was obtained from the patient for this publication.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Valdez-Hernández P, Ylhuicatzi-Durán M, Guerrero-Hernández M, Alvarado-Bachmann R, Angulo-Molina D. Manejo de una estenosis de la anastomosis bilioentérica con ablación por radiofrecuencia intraluminal. Rev Gastroenterol Mex. 2023;88:439–440.