A 27-year-old woman with an unremarkable past medical history was referred to us for an anorectal manometry study due to clinical symptoms characterized by chronic constipation since infancy that did not respond to treatments with laxatives or enemas. Symptoms had worsened in recent months, prompting her to seek the evaluation of a proctologist.
Physical examination revealed a mildly distended abdomen and no other relevant alterations. No abnormalities resulted from the rectal examination.
General laboratory tests were performed (complete blood count, blood chemistry, and TSH) and the results were within the normal ranges.
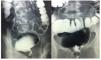
A barium enema study identified megarectum (fig. 1).
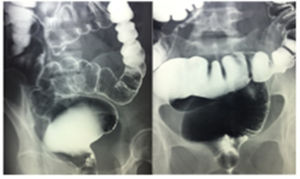
The anorectal manometry study revealed an anal canal with normal length, baseline and phasic canal pressures within normal values, adequate rectal sensitivity and capacity, the Valsalva maneuver with no escape, inhibitory rectoanal reflex absent up to the maximum tolerable rectal capacity (120 cc), and positive balloon expulsion maneuver. The results were consistent with Hirschsprung's disease (fig. 2).
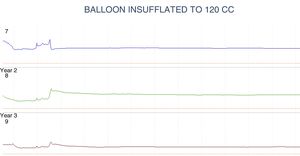
A full-thickness biopsy was taken from the wall of the rectum, with the following findings: absence of mature and immature ganglion cells in the submucosal plexus of the wall of the rectum and a marked reduction of interstitial cells of Cajal in the muscle wall.
Auerbach's myenteric plexus was not identified. Immunohistochemistry with: S-100 protein (detection of neuronal cells): positive in the plexuses.
Chromogranin (detection of neuroendocrine cells): negative.
Calretinin (detection of ganglion cells): negative.
Bcl-2 (detection of enteric neurons): negative.
CD117 (detection of interstitial cells of Cajal): positive in interstitial cells of Cajal that were reduced in number.
Wall of the rectum with aganglionosis consistent with Hirschsprung's disease (fig. 3).
Hirschsprung's disease was described in 1886, with the report of 20 cases of congenital megacolon in children. It was later related to the absence of ganglion cells. Surgical treatment for the disease was described in 1948.1
It is a rare condition that affects 1:5,000 births.
Based on the length of the affected segment, it is classified as: short-segment (not extending beyond the sigmoid colon), which is the most frequent presentation (80%); Ultrashort or juxta-anal segment (patients with that presentation are considered to have more probability of reaching adulthood undiagnosed), and long-segment when it is proximal to the sigmoid colon.2
It is a rare disease in adulthood, but its diagnosis should be considered in cases of constipation that is refractory to conventional medical therapy.3
The disease predominates in females in patients above 10 years of age with a ratio of 3:1. However, aganglionosis of the short-segment pathology is more frequent in males, with a mean age of 20 years at the time of medical consultation. It can cause symptoms of severe chronic constipation or frequent episodes of fecal impaction.4
Diagnosis is based on the combination of anorectal physiology studies (sensitivity 91%, specificity 94%) and the characteristic finding is absence of the inhibitory rectoanal reflex. Baritated imaging studies (sensitivity 70%, specificity 83%) can identify the so-called «transition zone» and inversion of the rectosigmoid index. It should be emphasized that the aganglionic segment is strictured. Full-thickness biopsies of the wall of the rectum are considered the gold standard (100% sensitivity and specificity), in which the absence of ganglion cells in the submucosa and the myenteric plexus is pathognomonic.5
The treatment of choice is surgical and aganglionic segment resection and anastomosis of the healthy colonic segment to the anal canal can be performed laparoscopically.6
In adults, the treatment of choice is the Duhamel operation, which results in reduced fecal impaction after the procedure.3
There are few reports on this disease in stages after infancy in the national and international literature.1,3–6
It is important to consider the presence of this rare pathologic process in young adult patients with treatment-refractory chronic constipation, in whom other more common diseases have been ruled out through easily accessed studies, such as imaging or anorectal physiology studies.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Alcocer-Sánchez E, Pérez y López N, Fernández-Álvarez J, Zárate-Osorno A. Enfermedad de Hirschsprung como causa rara de estreñimiento refractario en un paciente adulto. Revista de Gastroenterología de México. 2019;84:253–254.