Approximately 20% of patients with acute pancreatitis will have a serious or severe episode. Pancreatic necrosis is the complication with the highest mortality rate of up to 17%, and it reaches 19.8% in patients with infected necrosis and organ failure.1
“Step-up” management is standardized for encapsulated pancreatic necrosis, in which the minimally invasive approach is ideal because of its efficacy and validation.2
The surgical approach depends on the site of the peripancreatic collections, and can be endoscopic transgastric drainage, percutaneous drainage, or video-assisted retroperitoneal debridement (VARD). The decision to start minimally invasive management allows more aggressive interventions to be delayed, enabling the necrotic collection to mature, and in some cases, be reversed, consequently reducing complications.3
VARD is a minimally invasive procedure, with direct visualization of the collection, but with a narrow surgical manipulation field. Its main complication is vascular injury and the development of pancreatic fistulas.4
Indocyanine green is a fluorescent dye that is visible with near-infrared light. It is detected by special cameras that transmit a signal to a monitor, where the structures taking up the dye are visualized. It is used in oncologic surgery with fluorescent markers, in lymphatic drainage identification, bile duct visualization, or tissue dissection.5 In pancreatic necrosis, coadjuvant use of indocyanine green during VARD is suggested, to guide the debridement.6
A 32-year-old man was admitted to the hospital due to painful abdominal symptoms. At admission, the laboratory work-up reported triglycerides of 5,020 mg/dl, cholesterol of 417 mg/dl, serum amylase of 930 U/l, and serum lipase of 3,357 U/l, and a tomography scan revealed acute edematous pancreatitis. The patient then presented with clinical deterioration, compartment syndrome, and multiple organ failure. Three laparotomies were performed. The first was carried out due to compartment syndrome and the second because of the patient’s clinical deterioration, during which necrosis of the tail of the pancreas was found intraoperatively, resulting in the performance of open necrosectomy. In the third laparotomy, partial omentectomy secondary to infarction was carried out. A postoperative grade C distal pancreatic fistula secondary to the necrosectomy was diagnosed and treated with a somatostatin analogue. A control tomography scan identified fluid collections along the left parietocolic gutter extending to the pelvic excavation, for which a three-week regimen of antibiotics was started. Afterwards, percutaneous drainage was performed, following the “step-up” management of pancreatic necrosis, placing two pigtail catheters in said collections.
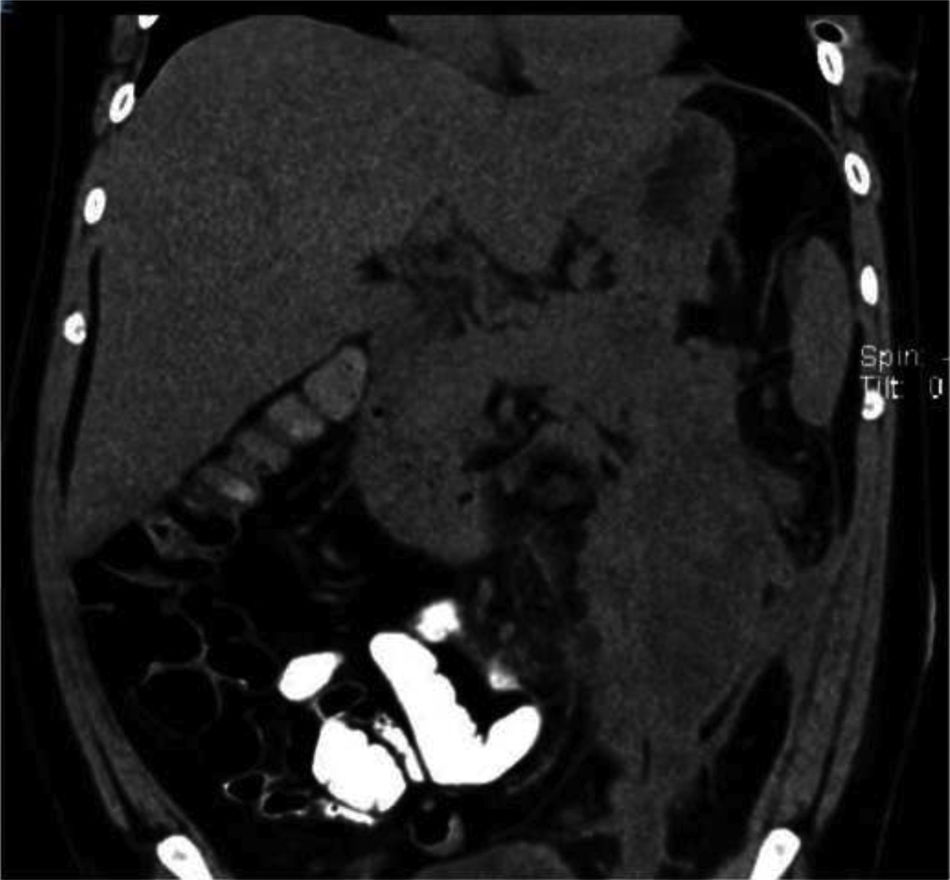
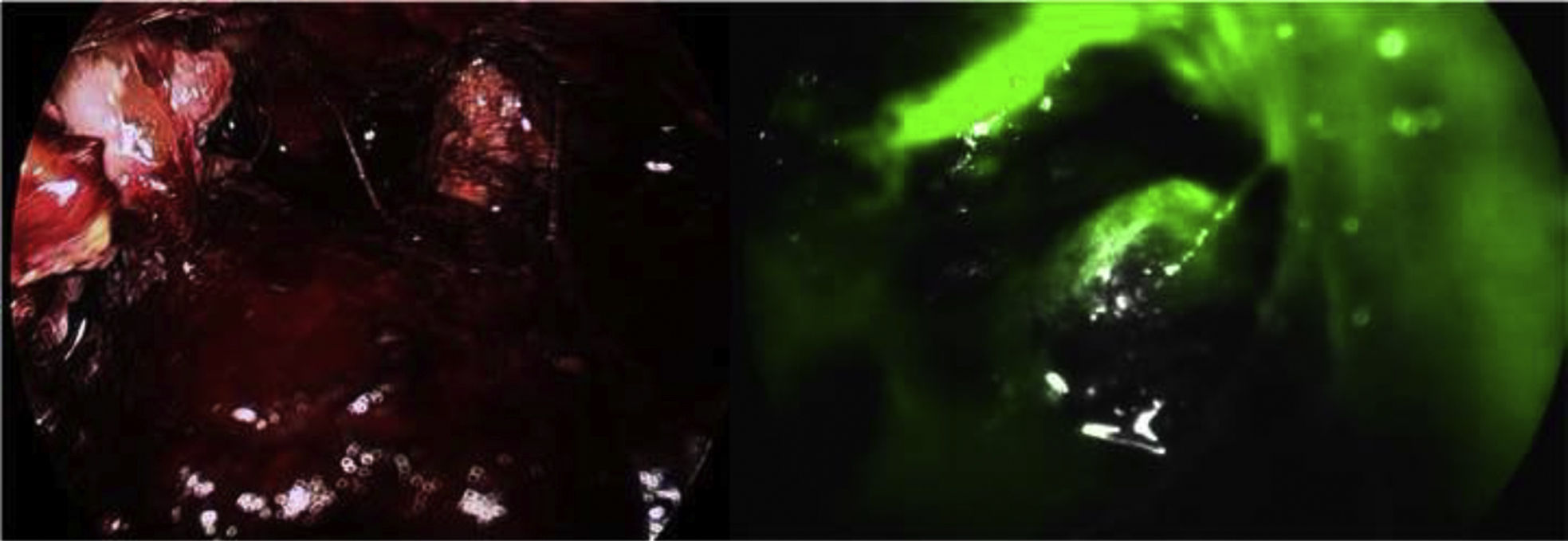
Fifteen days later, the patient’s torpid progression persisted. A control tomography scan revealed an encapsulated collection at the level of the tail of the pancreas and the left parietocolic gutter (Fig. 1). The decision to carry out VARD was made. Forty-five minutes before the surgery, 2.5 ml of indocyanine green was administered, diluted in 5 cc of saline solution. A pigtail catheter was placed at the left mid-axillary line 5 cm above the anterior superior iliac spine to introduce a 12 mm trocar. CO2 insufflation up to 12 mmHg was carried out, and a 5 mm trocar was placed under direct vision. The necrotic fluid was aspirated, obtaining 600 cc of purulent fluid. Aided by the indocyanine green, the devitalized tissue was debrided, avoiding injury to the vascular structures and the main pancreatic duct. The cavity was washed with physiologic serum and the pigtail catheter was removed, placing a 25 F closed Blake drain (Fig. 2).
Tomography scans performed three days after the procedure identified a decrease in the pancreatic collection, measuring 60 cc. The patient’s clinical progression was satisfactory, and the catheters were removed, given the drainage reduction and pancreatic fistula resolution, after almost 4 months of hospitalization.
Encapsulated pancreatic necrosis is defined as mature peripancreatic collections with well-defined limits, 4 weeks after their initial presentation. Postoperative pancreatic fistula is a complication in the management of severe pancreatic necrosis, presenting with clinical deterioration and a high risk of death. Several medications have been suggested for its management, and somatostatin analogues have achieved a decrease in fistula output and closure time.7
We opted for VARD with the aid of indocyanine green, given the clinical deterioration of the patient and the location of the collections, thus reducing the possibility of vascular injury and damage to the nonnecrotized inflammatory tissue. Improvement was rapid after this procedure. These results are relevant, given the scant experience there is with the concomitant use of VARD and indocyanine green and the lack of articles on such cases in the literature.8
The combination of minimally invasive surgery and visualization techniques, such as indocyanine green, can be initially used in these types of cases to prevent future reinterventions, shorten the length of hospital stay, and reduce complications, compared with open necrosectomy.9 VARD and indocyanine green are proposed to be safe and easy-to-apply in pancreatic necrosectomy.10
CRediT authorship contribution statementThe authors declare that prior to the surgical procedure, a written statement of informed consent was requested of the patient, his family member, for this research. Because this is a case report, authorization by an ethics committee was not requested. The authors declare that this article contains no information that could identify the patient.
Financial disclosureNo financial support was received in relation to this article.