Rumination syndrome is a condition characterized by repetitive, effortless regurgitation into the mouth of recently ingested food, followed by rechewing and swallowing or expulsion of the food bolus.1
Rumination episodes are produced in the immediate postprandial period and are due to a deliberate increase in intragastric pressure resulting from the contraction of the abdominal wall musculature. This increased pressure surpasses that of the lower esophageal sphincter, facilitating the passage of gastric content into the esophagus. Once the gastric content reaches the esophagus, upper esophageal sphincter relaxation is produced, enabling the later passage of the gastric content into the pharynx and mouth, where it can be newly chewed and swallowed.2
The current diagnosis of rumination syndrome is clinical and based on the Rome IV criteria. However, distinguishing this syndrome from gastroesophageal reflux disease (GERD) can be challenging.1 High-resolution esophageal manometry with impedance monitoring, followed by a solid food challenge, can confirm the diagnosis.2–4 This intervention is particularly useful in patients in whom the differential diagnosis with GERD is needed or in those with poor acceptance of the diagnosis.
We report herein the manometric findings of an 18-year-old female patient with a history of anorexia nervosa at 14 years of age and clinical symptoms of six-month progression characterized by heartburn, regurgitation, swallowing the regurgitated content, and occasional vomiting of the food content, all occurring exclusively in the postprandial period. Treatment with metoclopramide, omeprazole, and magaldrate did not improve her symptoms. Upper gastrointestinal endoscopy identified no alterations in the esophageal lumen or the esophagogastric junction.
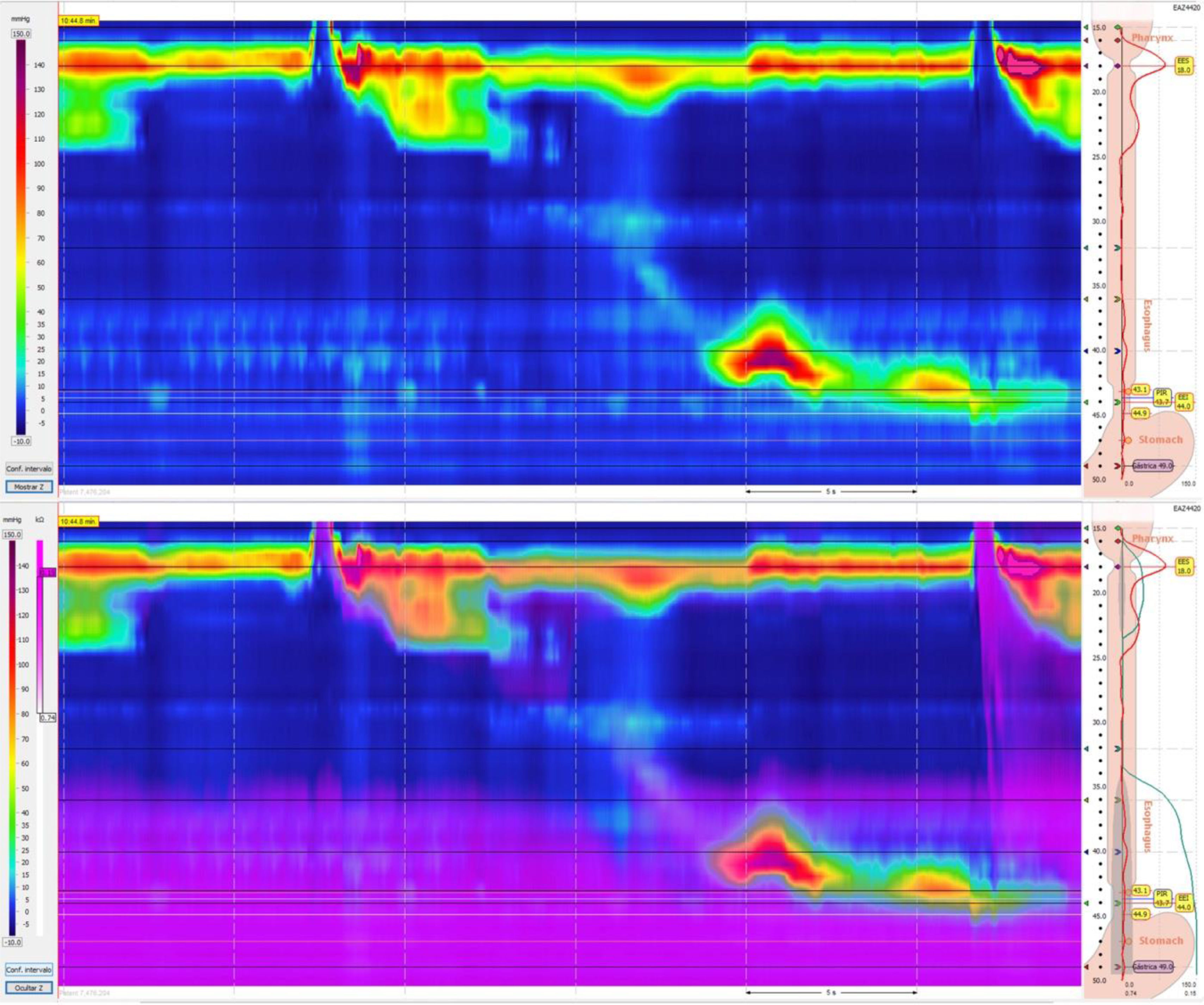
In high-resolution esophageal manometry with impedance monitoring (Fig. 1), ineffective motility, in the context of the Chicago classification 4.0 protocol, was observed, as well as no increase in intragastric pressure or retrograde flow of food content into the esophagus or pharynx.
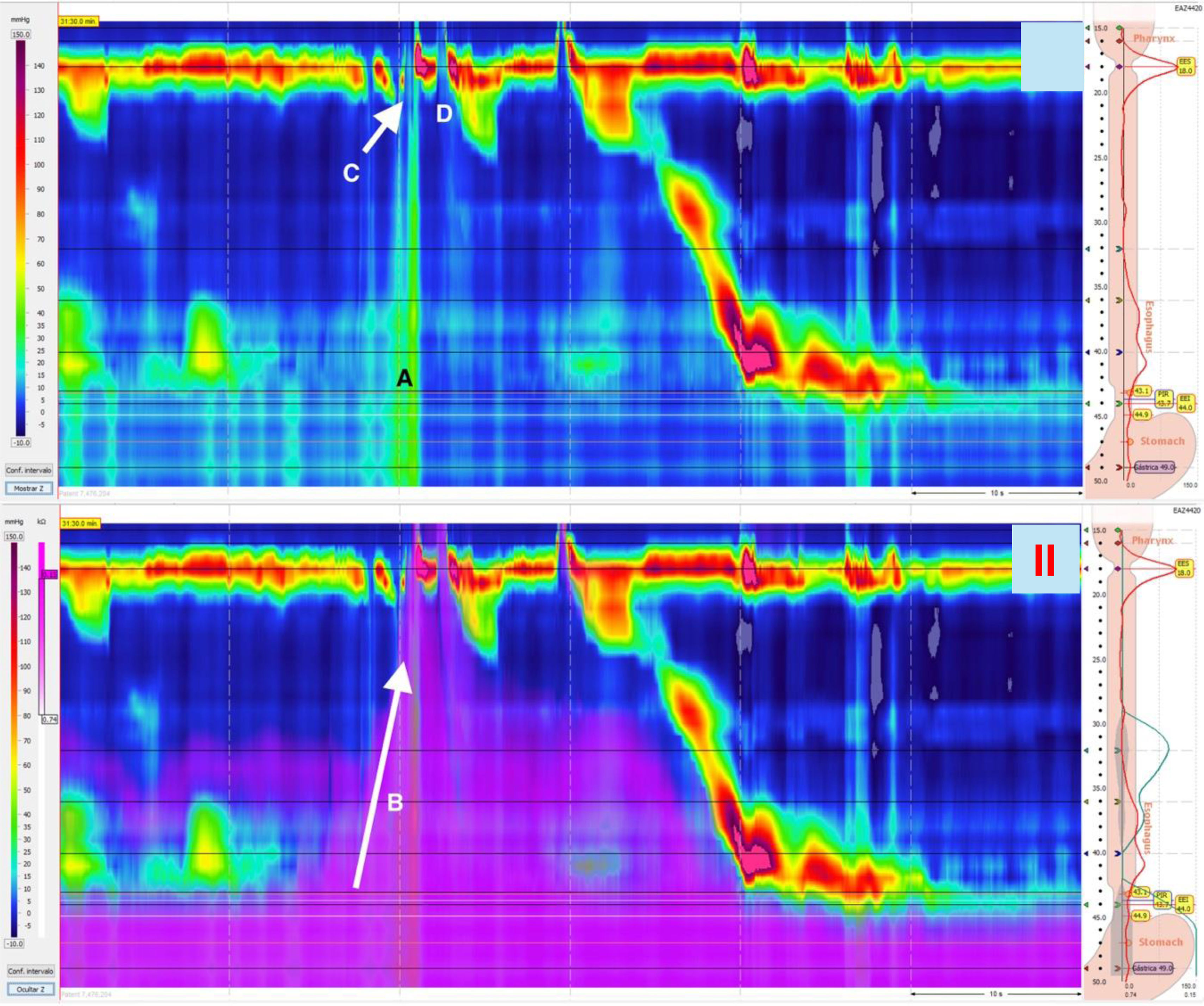
As part of the diagnostic evaluation, a diet consisting of a sandwich and apple juice (250 ml) was provided, enabling us to document several episodes of an increase above 30 mmHg in the intragastric baseline pressure and relaxation of the upper and lower esophageal sphincters, with the passage of gastric content into the pharynx, and subsequent swallows with complete clearance of the bolus, demonstrated by the decrease in impedance (Fig. 2).
A rumination episode in high-resolution manometry/impedance. Image I shows an elevation in intragastric pressure (A) that precedes the retrograde flow of the bolus into the esophagus (B), the simultaneous opening of the upper esophageal sphincter (C), and subsequent swallowing (D). Image II shows the retrograde movement through impedance during the rumination episode.
Thus, we reinforce the need to carry out provocative maneuvers directed at diagnostic suspicion, during high-resolution esophageal manometry. With respect to rumination syndrome, the administration of a solid and liquid food that the patient says causes his/her symptoms5,6 and monitoring beyond the complete Chicago 4.0 protocol have been shown to aid in making the differential diagnosis with regurgitation episodes in GERD and belching associated with regurgitation.3,4
Ethical considerationsThe present work meets the current research and bioethics regulations of the Research and Ethics Committee of the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, and given the nature of the publication, did not require its authorization. In addition, the authors declare that this article contains no personal information that could identify the patient.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.