Lichen planus is an inflammatory disease of unknown etiology that affects the squamous epithelium of the skin and mucosae and less frequently involves the esophagus.1 Oral cavity compromise supposes a risk factor for the development of squamous cell carcinoma, but there is less information on the potential malignancy from esophageal involvement.
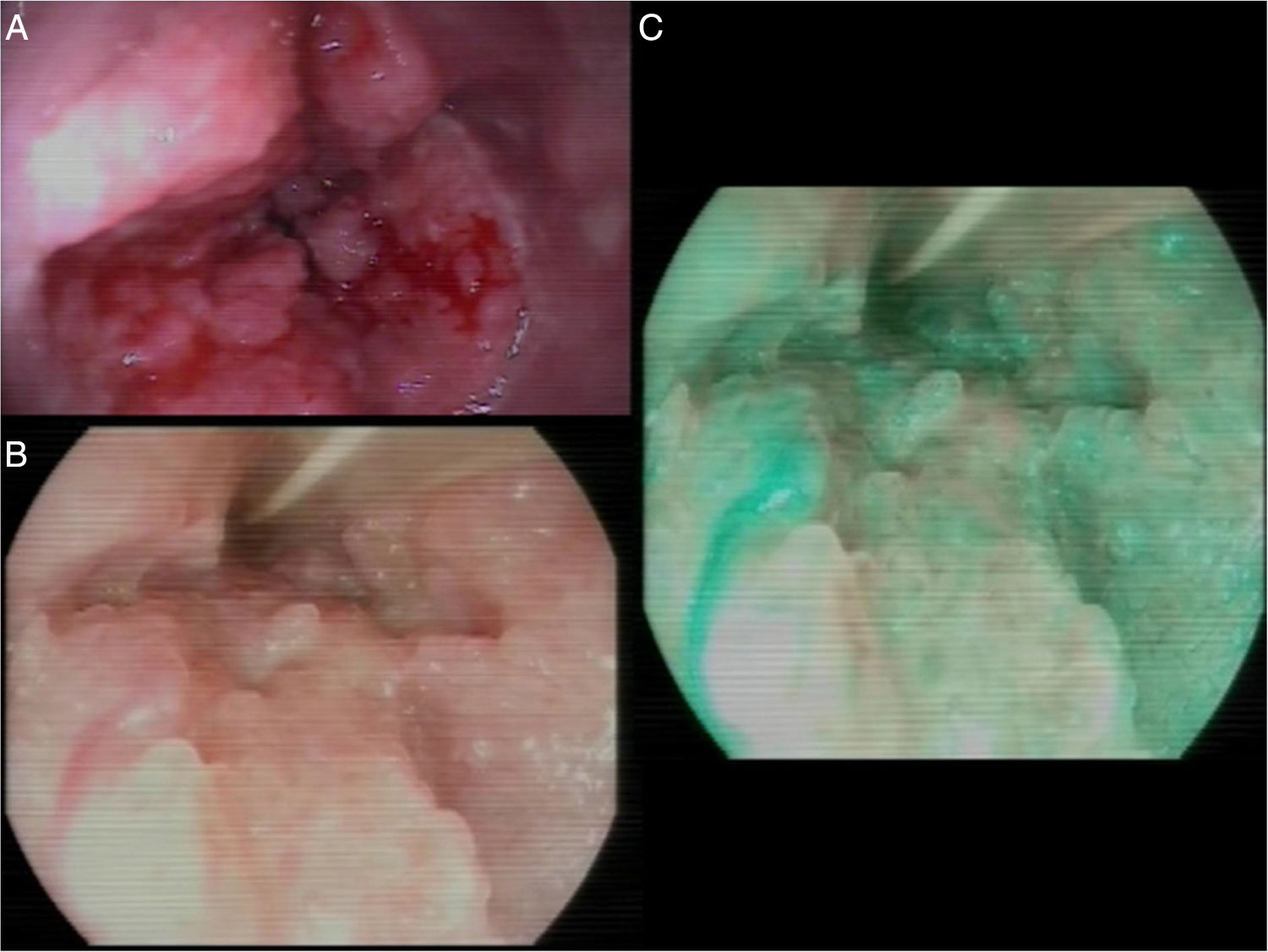
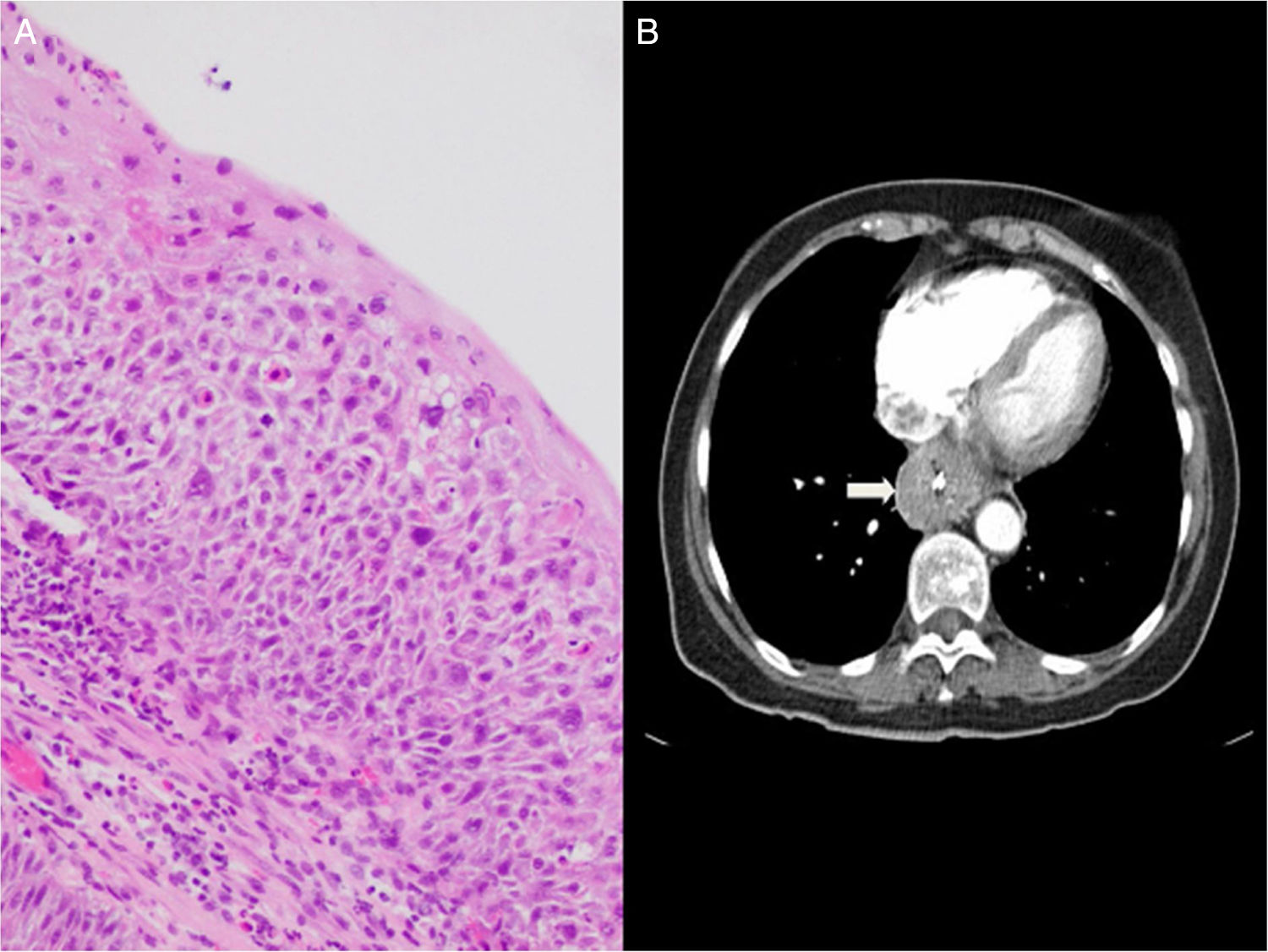
A 69-year-old woman, nonsmoker, nondrinker, sought medical attention for dysphagia. She had been diagnosed with lichen planus at different mucosal locations and presented with secondary urethral stricture that required intervention. Several years earlier, under dysphagia follow-up at another center, she presented with various esophageal strictures secondary to lichen planus that required successive endoscopic dilations. Treatment with corticoids was begun, but was suspended due to intolerance, and so the patient only had endoscopic follow-up. During the control endoscopies, the presence of squamous cell papillomas was observed in the distal third of the esophagus. They were resected endoscopically, and argon plasma therapy was carried out. The patient suspended follow-up and came to our center six months later due to dysphagia to both solids and liquids. Endoscopy was performed, revealing a mamillated neoformation of increased consistency, 30cm from the dental arcade, that caused stricture at the lumen and impeded the passage of the endoscope (fig. 1. A-C). Several biopsies were taken that were diagnosed as papillary squamous cell lesions, with areas of severe dysplasia/intraepithelial squamous cell carcinoma (fig. 2A). The biopsy samples underwent PCR testing to detect human papillomavirus (HPV) and were negative. Evaluation was completed with a CT scan of the chest and abdomen that identified thickening of the distal esophageal walls and gastric fundus, with no other remarkable alterations (fig. 2B). Given those findings, the multidisciplinary committee decided to administer neoadjuvant treatment with chemoradiotherapy and then surgical treatment through esophagectomy. There were no signs suggestive of malignancy in the anatomopathologic specimen.
The appearance of esophageal lichen planus is usually associated with cutaneous or oral involvement, but its presentation can be isolated.2 The majority of patients with lichen planus of the esophagus are middle-aged women. Fox et al. studied 72 patients with esophageal lichen planus, 87% of whom were women, with a mean age of 61.9 years.1 Dysphagia is the predominant symptom in the majority of patients.3 Medical treatment can include corticoids, as well as other immunosuppressants, albeit their use is not well-standardized. At endoscopy, involvement can be in the proximal esophagus, which is the most frequent, as well as in the distal portion.1 In the case presented herein, the patient was a woman with oral and cutaneous lichen planus of long evolution whose initial symptom was dysphagia, but the stricture was located in the distal esophagus. Endoscopic findings can include friable mucosa, whitish papules, erosions, and single or multiple strictures.4 If strictures are found, as in our case, endoscopic treatment with dilations may be necessary. The potential for malignancy of lichen planus at other locations, such as the oral cavity, has been well-known for several years,5 but few cases of malignant transformation of lichen planus with esophageal involvement have been reported.6 The presence of esophageal papillomatosis is a rare endoscopic finding, the origin of which is the presence of gastroesophageal reflux, human papillomavirus (HPV), or continuous aggressions to the mucosa. In our patient, human papillomavirus (HPV) was ruled out, and compromise due to lichen planus could be considered a chronically irritating agent that predisposed to the development of esophageal papillomatosis, but there are no similar reports in the literature. Endoscopic treatment of papillomas is controversial, but the extirpation of isolated lesions through customary endoscopic techniques (biopsy forceps, polypectomy snare, fulguration) is accepted.7 Nevertheless, the treatment of multiple lesions is not well-established, with some authors employing radiofrequency.8 Once papillomas are extirpated, their recurrence is low,9 but they recurred in our patient despite several previous extirpations attempts. In cases of squamous cell carcinoma of the esophagus, causal factors such as smoking, alcohol, and HPV infection should be considered.10 The only recognizable etiologic factor in our patient was the presence of lichen planus. Endoscopy could play a role in the follow-up of those patients for the early detection of squamous cell carcinoma, utilizing both chromoendoscopy and magnification endoscopy. Dysplasia in samples of the mucosa with a lichenoid infiltrate may not be detected in all cases, but in our patient, areas of severe dysplasia/intraepithelial squamous cell carcinoma were clearly identified. The patient began neoadjuvant treatment with chemoradiotherapy, which could explain the absence of dysplastic/intraepithelial squamous cell carcinoma in the specimen studied after esophagectomy.
In conclusion, lichen planus with esophageal involvement is a rare entity that should be suspected in middle-aged women with dysphagia and a history of lichen planus at other sites. Although it is an uncommon pathology, it is potentially malignant, as in the case presented herein and the few other published cases, which could justify endoscopic follow-up.
Ethical considerationsThe patient signed a statement of informed consent before the present article was sent to be considered for publication.
The work meets current bioethical regulations. It was not reviewed by an ethics committee, given that the patient was informed as to the anonymous use of clinical data, as well as endoscopic and radiologic images, in which she could not be identified. In addition, she signed a corresponding statement of informed consent.
The authors declare that the present article contains no personal information that could identify the patient.
Financial disclosureNo financial support was received in relation to the present article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Honrubia-López R, Manceñido-Marcos N, Pajares-Villarroya R, Muñoz-Fernández de Legaria M, Comas-Redondo C. Liquen plano con afectación esofágica. Revista de Gastroenterología de México. 2020;85:97–99.