Neuroendocrine tumors make up a group of heterogeneous lesions originating from cells located in the neuroendocrine system, with properties similar to those of nerve (the presence of dense granules that contain monoamines) and endocrine (the ability to synthetize and secrete said substances) tissues.1,2
At the level of the small bowel, most are non-functioning tumors, but up to 20% of patients may present with liver metastases and carcinoid syndrome. Those types of tumors are usually larger than 2 cm, presenting external muscle layer invasion and lymph node disease at diagnosis, and 40% of patients present with multiple synchronous lesions. There may also be symptoms of abdominal pain, bowel obstruction, diarrhea, weight loss, or gastrointestinal bleeding.3,4
A 64-year-old man with an unremarkable past medical history was referred to the general and digestive surgery service due to chronic abdominal pain of two-year progression and progressive weight loss of 15 kg. The patient was symptomatic when evaluated, stating that the pain had intensified within approximately 24 h and that he presented with vomiting and was unable to retain food.
A computed tomography scan with intravenous and oral contrast revealed multiple air-fluid levels, with the presence of gas in the distal colon, and a transition zone in the area of the ileum-ileocecal valve, with thickening of that segment, intestinal pneumatosis, and thickening in the region of the mesentery (Fig. 1).
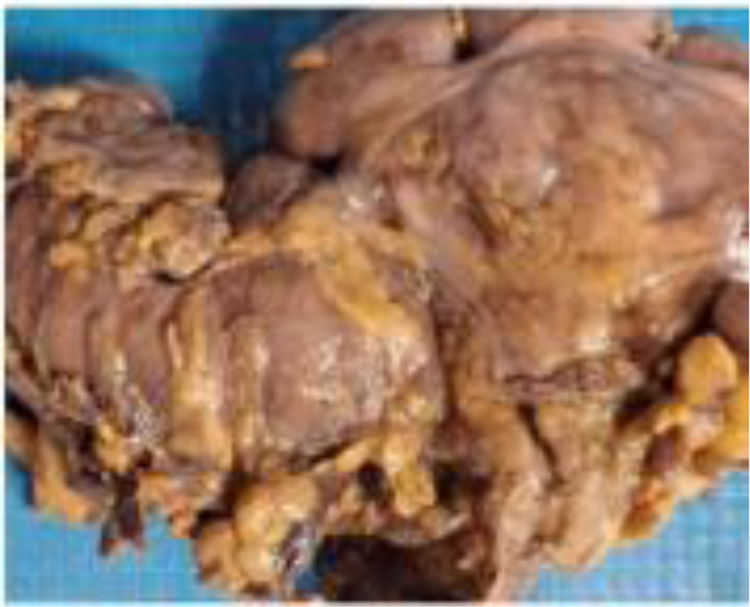
The patient received medical treatment with intravenous solutions, bowel rest, and nasogastric tube placement. Given that he did not improve, an exploratory laparotomy was performed, revealing a strictured lesion measuring approximately 4 cm in the terminal ileum at 65 cm from the ileocecal valve, multiple adenopathies measuring 3 cm in the mesentery at the level of the mesenteric blood vessels, and irregular, hardened nodular lesions at the level of the liver. Bowel resection, the Hartmann procedure, and ileostomy were performed, taking biopsy samples from the mesentery and intestinal segment, and the surgical specimen was sent to the clinical-surgical pathology department (Fig. 2).
Surgical specimen of the ileum showing tissue from the terminal ileum, ileocecal valve, cecal appendix, and cecum (colon). A strictured zone is located at 5.0 cm from the proximal limit and 6.0 cm from the distal limit, located at the junctional zone of the terminal ileum and ileocecal valve, measuring 3.0 × 2.0 cm, and causing obstruction of 95% of the lumen.
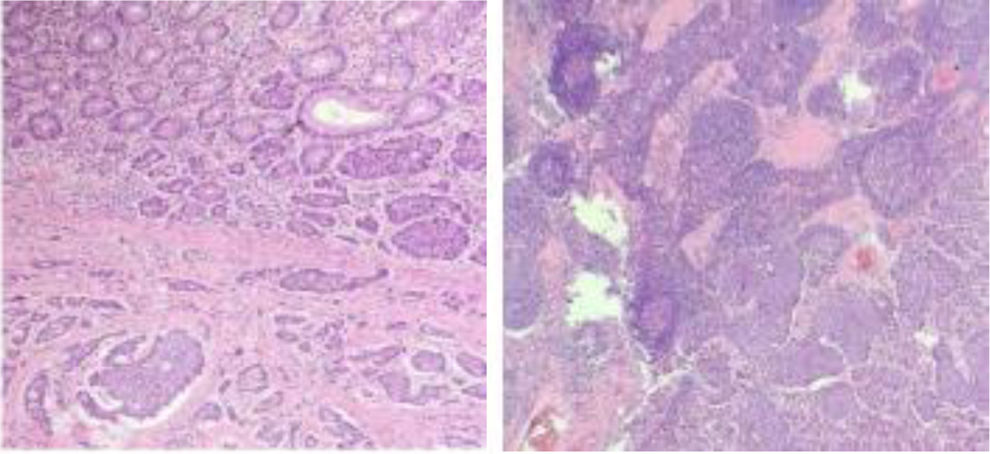
The histology study reported carcinoma with a moderately differentiated neuroendocrine tumor, measuring 3.0 × 2.0 cm, with 95% obstruction of the lumen, a disease-free distal limit located 6.0 cm from the tumor and disease-free proximal limit located 5.0 cm from the tumor, with 5/13 metastatic lymph nodes, and confirmatory immunohistochemical tests (Fig. 3).
A new computed axial tomography scan with intravenous and oral contrast revealed an absence of distant metastasis, and the patient was referred to the oncology department.
In cases of small bowel neuroendocrine tumors, curative surgical treatment is recommended in asymptomatic patients, following oncologic principles. When the disease is in advanced stages, the surgical approach is difficult, or nearly impossible. For patients with metastatic disease, curative surgical treatment (resection of the primary tumor, regional lymph nodes, and liver metastases) is achieved in 20% of cases. At advanced disease stages, the goal of palliative surgery is to treat complications, such as bowel obstruction, and those secondary to the primary tumor, focusing on the therapeutic measures to be taken for the metastatic disease, resulting in increased patient survival.5–7
In the case described herein, the emergency approach was carried out due to the presence of symptoms of bowel occlusion with acute abdomen. It entailed resection under the oncologic protocol, with a diversion procedure evaluated by the clinical oncology service. This is one of the clinical presentations of small bowel tumors. The general surgeon must have the differential diagnosis in a patient with chronic abdominal pain, occlusion, and acute abdomen. Diagnostic expertise for resolving the intraoperative findings is essential, maintaining oncologic resection standards at all times.
Ethical considerationsThe authors declare that for this research, prior to the surgical intervention, the patient and a relative signed a written statement of informed consent. Because this is a case report, authorization by the ethics committee was not requested. This article contains no data that can identify the patient.
Financial disclosureNo financial support was received in relation to this article.
The authors declare that there is no conflict of interest.