The liver parenchyma and its vascularization are fragile structures that are commonly injured in blunt abdominal trauma. Isolated liver injury management has undergone important modifications and is constantly evolving. While surgical examination remained the gold standard during the past century and beginnings of the present, the current tendency is nonoperative management or selective liver resections. Imaging study findings or the volume of the hemoperitoneum no longer determine the choice of management of those injuries,1,2 whereas hemodynamic stability, coagulopathy grade, hypothermia, and acidosis are parameters that more reliably reflect the clinical status of the patient.3 Presented herein is the clinical case of a high-grade liver injury and its successful nonoperative management.
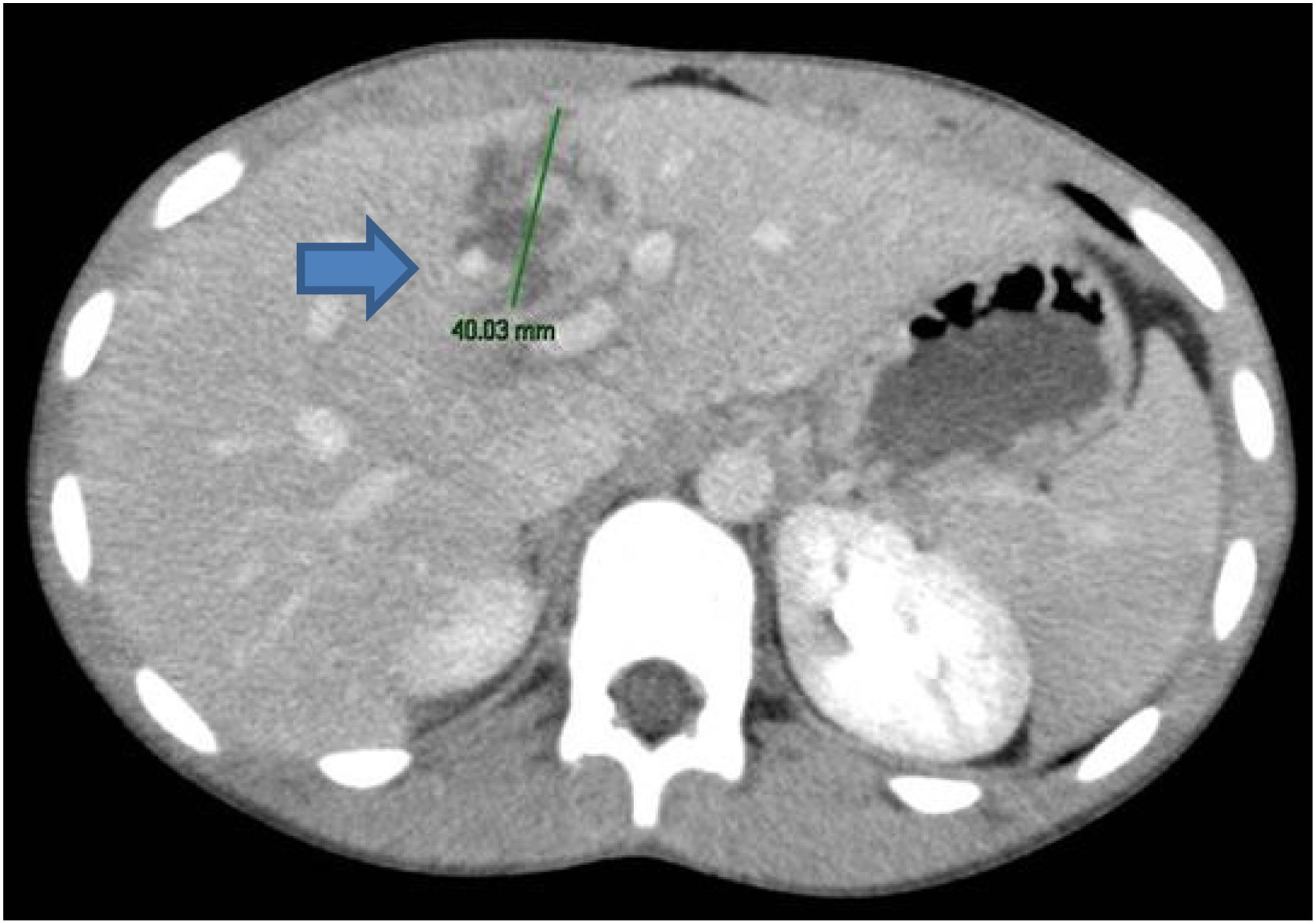
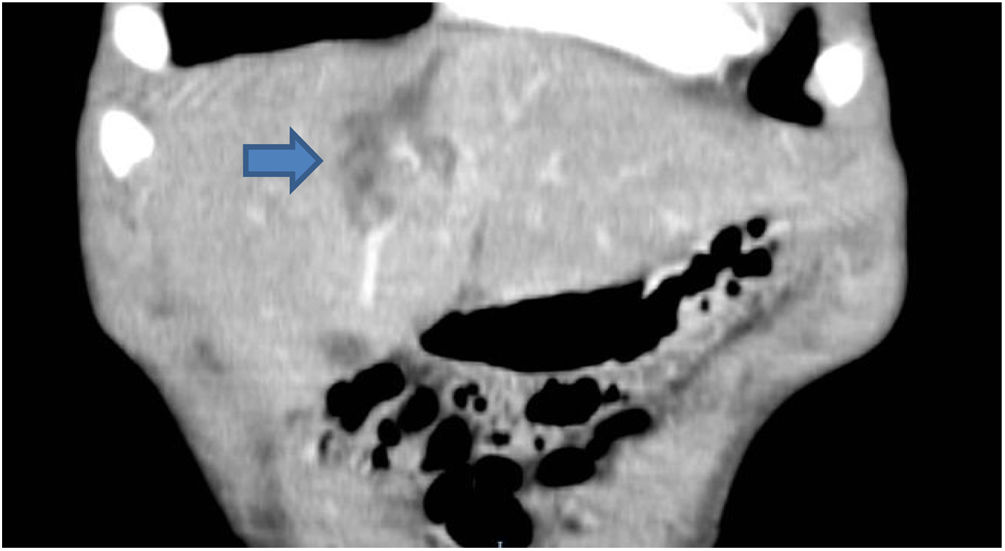
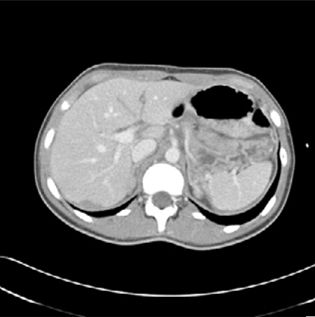
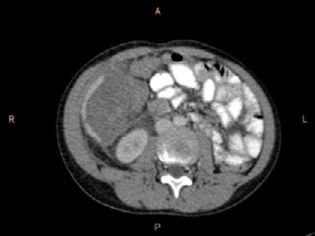
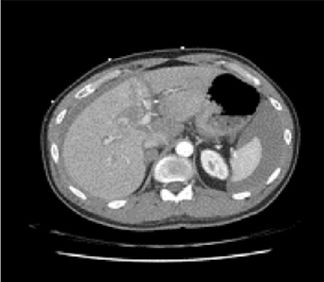
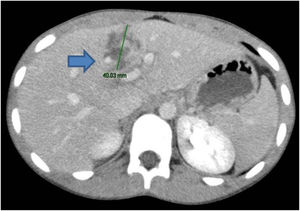
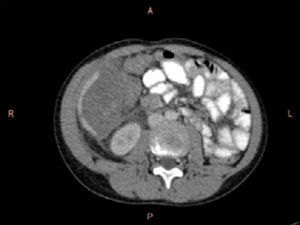
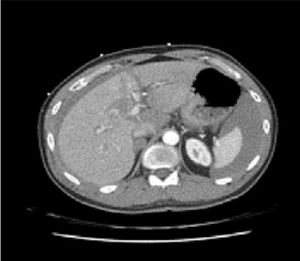
A 16-year-old male with an unremarkable past medical and surgical history suffered blunt abdominal trauma after a bicycle accident, in which the upper quadrants of the abdomen were injured by the handlebar. The patient did not lose consciousness. Upon arrival at the emergency department he was hemodynamically stable, and his physiologic parameters were within the normal range. Physical examination produced intense localized pain in the right hypochondrium and epigastrium. Laboratory study results were unaltered, with hemoglobin of 13.3 g/dl and hematocrit of 40.7%. An abdominal computed axial tomography scan identified hepatic lacerations at the level of segments IVa and IVb (Figs. 1 and 2), with no signs of active bleeding, corresponding to grade III injury, according to the organ injury scale of the American Association for the Surgery of Trauma (AAST),4 and moderate grade II injury, according to the World Society of Emergency Surgery (WSES) guidelines.5
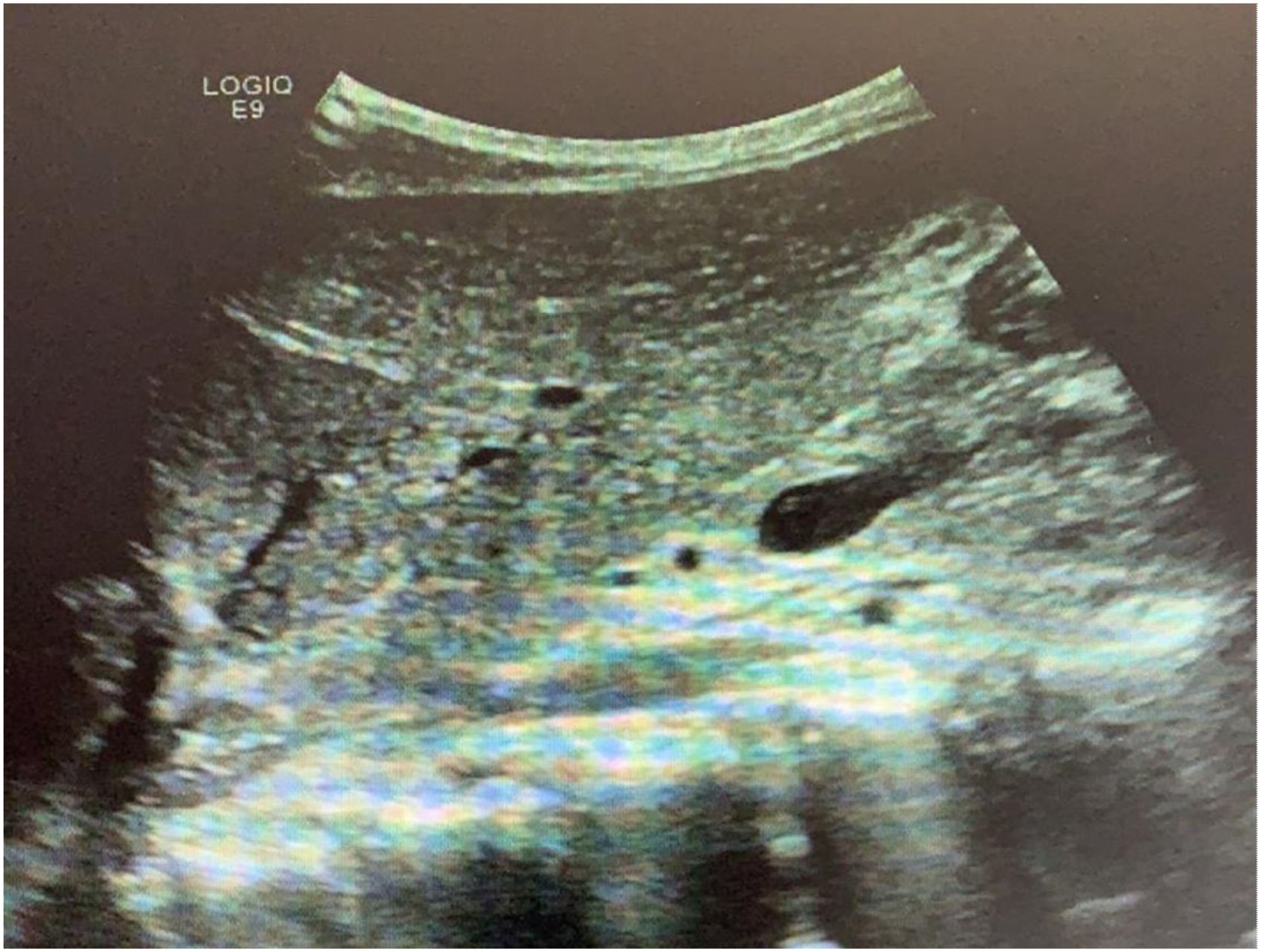
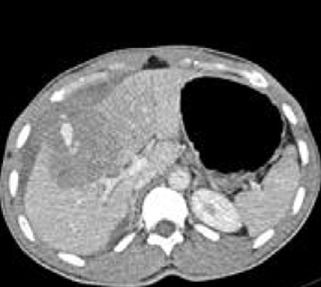
The patient was admitted to the intensive care unit, where he remained for 3 days. He was hemodynamically stable the entire time, did not require blood transfusion or vasopressors, made good clinical progression, and had stable laboratory parameters. He was sent to the hospital ward, where he was observed for 2 days. After a control abdominal ultrasound study showed good progression of the lesions (Fig. 3), the patient was released from the hospital to his home. At the follow-up consultation at 30 days, he was asymptomatic with no laboratory test result alterations. New imaging studies were not carried out.
The liver is a vulnerable organ in the context of blunt abdominal trauma, being the most frequently injured solid organ, whether individually or associated with injury to other intra-abdominal organs. Hepatic compromise should be suspected in all patients with anterior, as well as posterior, chest and abdominal trauma, especially if they present with a state of shock.6 Treatment of isolated blunt liver trauma has advanced considerably, and currently there is a clear tendency toward conservative or nonoperative management, when feasible.
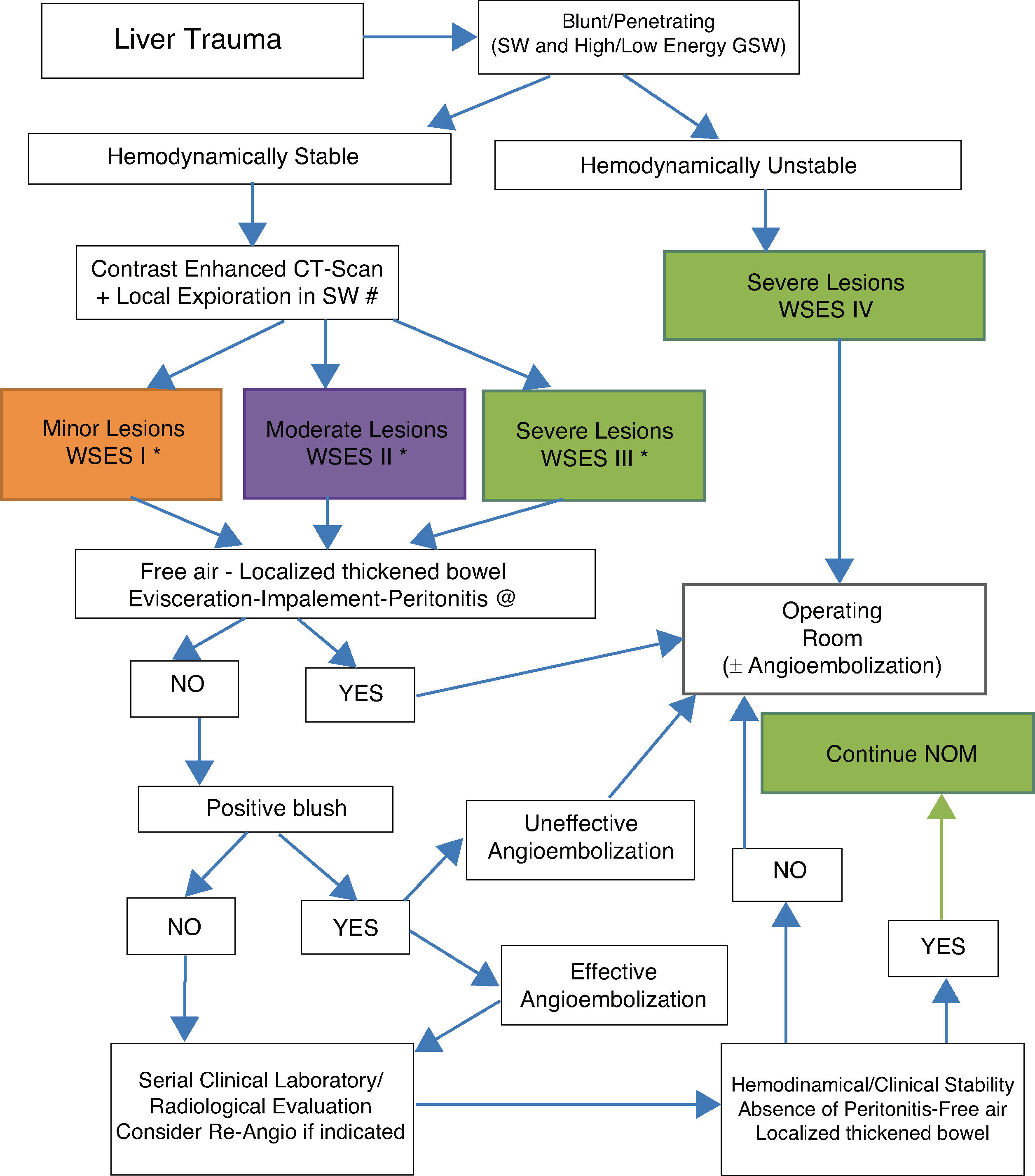
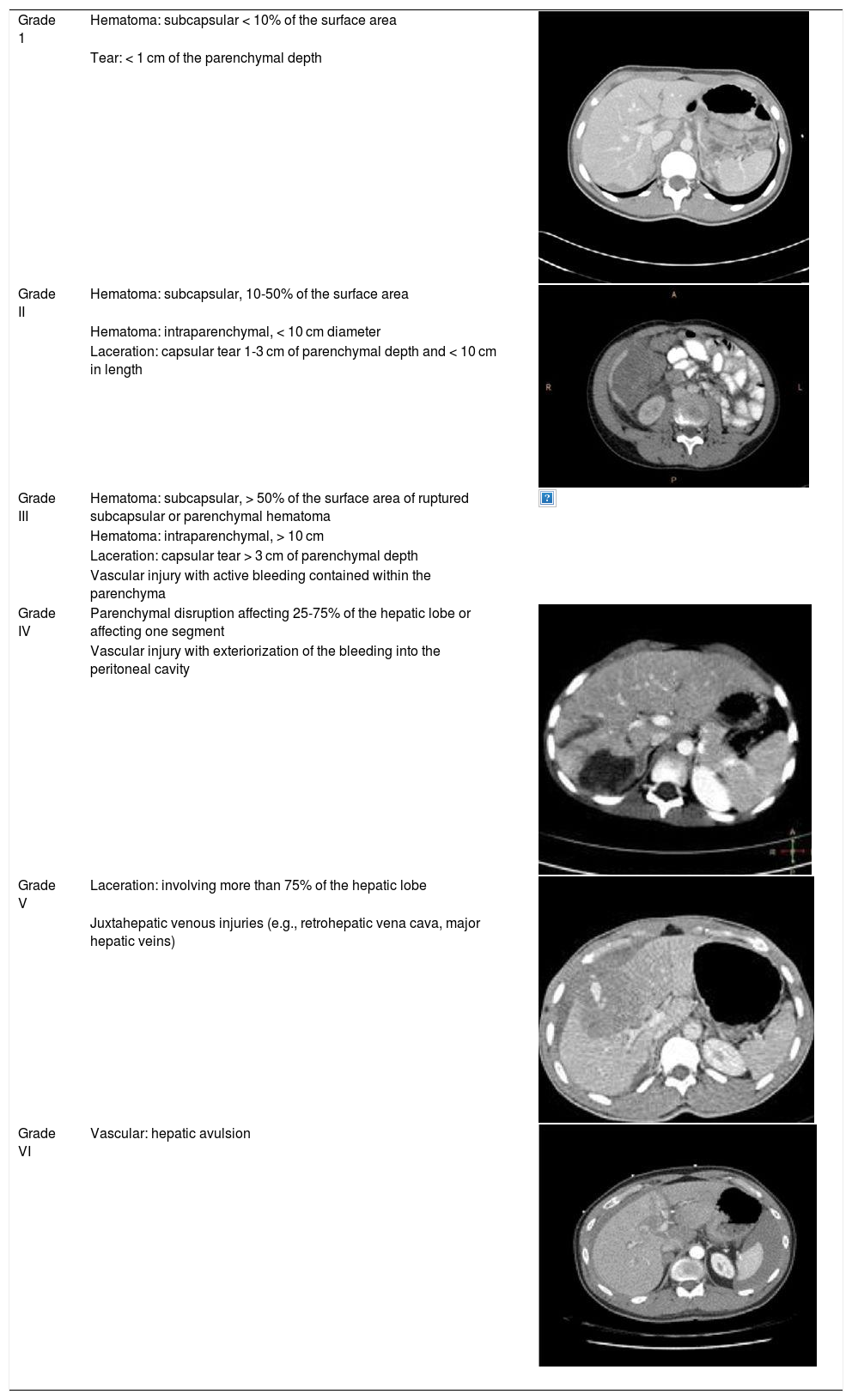
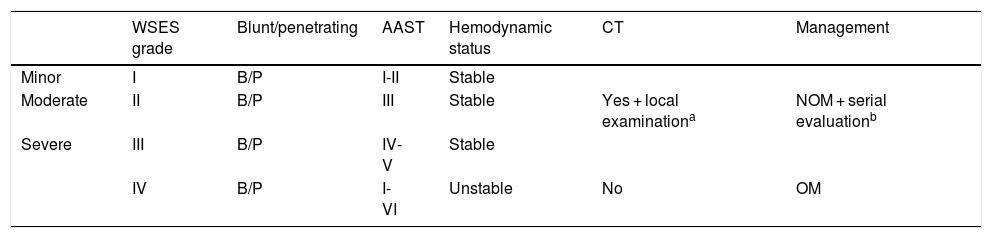
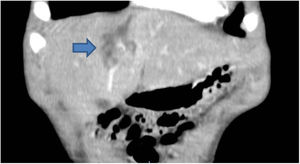
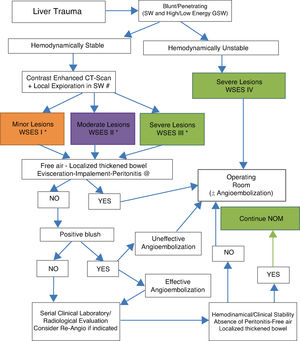
The advances made in the study of nonoperative management in the polytrauma patient, despite the difficulty of conducting prospective studies on that type of patient, have contributed to a reduction in the extremely high mortality rate associated with that type of trauma.7 The use of clinical guidelines aids in optimizing the management of those patients.8 The classification of liver injury according to the AAST and WSES grades (Tables 1 and 2) are particularly useful, as is the WSES therapeutic algorithm (Fig. 4), which recommends nonoperative management of blunt liver trauma in the absence of injuries that require surgical repair. It should be kept in mind that the management of those types of injuries is constantly evolving, and consequently there are other guidelines that not only take into account the extension of the injury, but also its location and mechanism.9
The American Association for the Surgery of Trauma (AAST) liver injury scale4 and the corresponding CT images.
| Grade 1 | Hematoma: subcapsular < 10% of the surface area | |
| Tear: < 1 cm of the parenchymal depth | ||
| Grade II | Hematoma: subcapsular, 10-50% of the surface area | |
| Hematoma: intraparenchymal, < 10 cm diameter | ||
| Laceration: capsular tear 1-3 cm of parenchymal depth and < 10 cm in length | ||
| Grade III | Hematoma: subcapsular, > 50% of the surface area of ruptured subcapsular or parenchymal hematoma | |
| Hematoma: intraparenchymal, > 10 cm | ||
| Laceration: capsular tear > 3 cm of parenchymal depth | ||
| Vascular injury with active bleeding contained within the parenchyma | ||
| Grade IV | Parenchymal disruption affecting 25-75% of the hepatic lobe or affecting one segment | |
| Vascular injury with exteriorization of the bleeding into the peritoneal cavity | ||
| Grade V | Laceration: involving more than 75% of the hepatic lobe | |
| Juxtahepatic venous injuries (e.g., retrohepatic vena cava, major hepatic veins) | ||
| Grade VI | Vascular: hepatic avulsion |
*One-grade progression due to multiple lesions up to grade III.
The World Society of Emergency Surgery (WSES) classification of liver trauma.5
| WSES grade | Blunt/penetrating | AAST | Hemodynamic status | CT | Management | |
|---|---|---|---|---|---|---|
| Minor | I | B/P | I-II | Stable | ||
| Moderate | II | B/P | III | Stable | Yes + local examinationa | NOM + serial evaluationb |
| Severe | III | B/P | IV-V | Stable | ||
| IV | B/P | I-VI | Unstable | No | OM |
NOM: nonoperative management; OM: operative management.
Diagnostic and therapeutic algorithm of liver trauma injuries (with permission of the WSES).5
Around 80% of patients with liver trauma have been shown to be successfully treated through conservative management.10 Reported failure rates have reached 3 to 10% and are mostly due to late bleeding, hematomas, and associated injuries.11 From the perspective of a significant reduction in the mortality rate in patients treated conservatively (from 5.6 to 1.3%), those results indicate improved use of the nonoperative management focus, compared with initial case series, in which 60% of the cases were treated conservatively, with a resultant failure rate of 15%.12
In the cases of isolated liver trauma, with hemodynamic stability and no need for surgery, nonoperative management is an option established in the latest guidelines that has had high success rates, preventing the morbidity and mortality associated with emergency surgery that is not always necessary. Biliary tree injury worsens outcome and requires endoscopic retrograde cholangiopancreatography.13 In cases in which nonoperative management is not possible, bleeding control by an interventional radiologist is an option to consider. The evolution of and experience with angioembolization makes it part of the therapeutic armamentarium in cases of severe hepatic trauma, in which there are signs of active bleeding.
Even though the majority of solid organ injuries can be treated with nonoperative management, mainly due to improvement in the interdisciplinary general treatment of trauma, an increased application of interventional radiology can be a key characteristic. The techniques of interventional radiology, especially in cases of contrast medium extravasation, have previously been described as important diagnostic and therapeutic tools in a relevant number of patients with blunt liver trauma for improving nonoperative management success rates and preventing unnecessary operations.14–17 Organ recovery rates vary from 86% to 100%, with success rates between 79% and 92% in liver trauma, through the use of arterial embolization,12,18,19 even when morbidity rates and complications, such as rebleeding, after angiography, are taken into consideration.14
Nonoperative management of liver trauma is not exempt from complications. In a review of 136 patients, Croce and Fabian20 reported bleeding (3.3%), biliomas (3%), abscesses (0.7%), and enteric lesions (0.3%), half of which were treated successfully through interventional radiology. However, liver injury still requires surgical intervention in the more complex cases.21 The main intervention principle should be liver damage control, with the adequate technique.
Fodor et al.22 confirmed the effectiveness of nonoperative management in patients with liver trauma, suggesting a safe and effective therapeutic focus, with general mortality rates below 2%. According to those findings, the majority of patients can be less invasively treated through nonoperative management, preventing unnecessary laparotomies. That has been shown to be particularly true in recent nonoperative management rates in liver trauma that surpass 95%.
Despite the continuous advances made in the areas of trauma surgery and surgical critical care, mortality due to complex liver injury remains extremely high. Likewise, its surgical management is a challenge of great difficulty, even for surgeons with vast experience in trauma. The inability to control bleeding continues to be the primary cause of death, accounting for more than 50% of cases. AAST grade IV and V lesions are the most severe injuries facing the trauma surgeon. The majority of those patients are in a state of shock, entering into the vicious cycle of the lethal acidosis, hypothermia, and coagulopathy triad23 that invariably leads to arrythmias and death. The complexity of those injuries forces the surgeon to employ surgical procedures that are not commonly performed. Given that only 5% of injuries are grades IV and V, few trauma centers have an important level of experience in their management.24 Better results will be obtained, the more experience the surgeon has in liver trauma surgery and control of the resulting damage.25
FundingThere was no source of funding.
Declaration of Competing InterestThe authors declare that they have no conflict of interests.
Please cite this article as: Pérez-Alonso A, Rodríguez-Martinón P, Caballero-Marcos L, Petrone P. Manejo no operatorio en un paciente con traumatismo hepático contuso de grado moderado. Revista de Gastroenterología de México. 2020;85:486–490.