Orthotopic liver transplant (OLT) is the definitive treatment of most types of liver failure. Transjugular intrahepatic portosystemic shunt (TIPS) and portocaval shunt placement procedures reduce the systemic vascular complications of portal hypertension. TIPS placement remains a “bridge” therapy that enables treatment of refractory symptoms until transplantation becomes available. The aim of the present study was to describe the operative impact of TIPS prior to OLT.
Materials and methodsA retrospective review was conducted on patients that underwent liver transplant at the Hospital San José within the timeframe of 1999 and February 2020.
ResultsWe reviewed a total of 92 patients with OLT. Sixty-six patients were male and 26 were female, with a mean age of 52 years. Nine (9.8%) of the 92 patients had a TIPS, before the OLT. Preoperative Child-Pugh class, MELD score, and sodium and platelet levels were similar between groups. We found no difference in the means of intensive care unit stay, operative time, or blood transfusions for liver transplant, with or without previous TIPS. There was no significant difference between groups regarding vascular and biliary complication rates or the need for early intervention. The overall one-year mortality rate in the TIPS group was 11%.
ConclusionsTIPS is an appropriate therapeutic bridge towards liver transplant. We found no greater operative or postoperative complications in patients with TIPS before OLT, when compared with OLT patients without TIPS. The need for transfusion, operative time, and ICU stay were similar in both groups.
El trasplante de hígado ortotópico (OLT, por sus iniciales en inglés) es el tratamiento definitivo para la mayoría de los tipos de falla hepática. Procedimientos tales como la derivación portosistémica intrahepática transyugular (TIPS, por sus iniciales en inglés) y la derivación portocava, reducen las complicaciones vasculares sistémicas de la hipertensión portal. El procedimiento de TIPS permanece como una terapia de “puente”, para permitir el tratamiento de síntomas refractarios hasta que el trasplante esté disponible. Este estudio busca describir el impacto operatorio de una TIPS previo a un OLT.
Material y métodosSe realizó una revisión retrospectiva en pacientes que fueron sometidos a trasplante hepático en el Hospital San José, de 1999 hasta febrero del 2020.
ResultadosSe incluyeron 92 pacientes con OLT. Sesenta y seis fueron masculinos y 26 femeninos, con una edad promedio de 52 años. Nueve de los 92 pacientes (9.8%) tuvieron una TIPS previo al OLT. Los valores de clase Child, MELD, sodio en sangre y plaquetas fueron similares en el preoperatorio de ambos grupos. No encontramos diferencia en las medias de estancia en la unidad de cuidados intensivos (UCI), tiempo operatorio y transfusiones de sangre para OLT, con o sin TIPS previa. Las tasas de complicaciones vasculares y biliares, así como la necesidad de una intervención temprana, no fueron significativamente diferentes entre los grupos. La mortalidad general en un año en el grupo TIPS fue del 11%.
ConclusionesLa TIPS es un puente terapéutico apropiado para el trasplante de hígado. No encontramos mayores complicaciones operatorias o postoperatorias en los pacientes con TIPS antes del OLT, en comparación con los pacientes con OLT sin TIPS. La necesidad de transfusión, el tiempo operatorio y la estancia en la UCI fueron similares en ambos grupos.
Liver transplantation has come a long way over the past 50 years, becoming the mainstay definitive treatment of most types of liver failure. Advancements in both operative techniques for enhanced recovery and pharmacologic management have greatly increased survival rates in recipients1. The disparity between available donors and waitlisted patients is still a great challenge. Of the 317 patients on Mexico’s 2019 liver transplant waiting list, only 223 received a graft, accounting for just 70% of the patients in need2. This seemingly universal barrier is also present in the developed world. The United Kingdom reported that the discrepancy leads to the death of ∼9% of patients listed for transplant, before a donor organ becomes available. The United States reports that waitlist mortality varies geographically, ranging from 6.5 to 37.4 deaths per 100 waitlist-years3,4.
Medical therapy has evolved and been optimized for the treatment of patients with liver failure, as have procedures designed to aid and restore the physiologic baseline. Procedures, such as transjugular intrahepatic portosystemic shunt (TIPS) and portocaval shunt placement, aim to reduce the systemic vascular complications of portal hypertension5. Rapid normalization leads to mesenteric venous decongestion, increased effective arterial blood volume, and increased response to pharmacologic management6,7 that clinically translates to a lower incidence of variceal bleeding, decreased bacterial translocation, and improved renal function8. Current indications for TIPS placement include refractory esophageal varices or early interventions for patients with a high risk of treatment failure, Budd-Chiari syndrome, and treatment-refractory ascites, showing superior control, increased survival, and better glomerular filtration rates, when compared with paracentesis8,9. However, the benefits of TIPS placement come at the cost of worsening liver function. Decreased perfusion shows increased international normalized ratio and bilirubin values, reduced albumin, and an increased risk of developing pulmonary hypertension, due to cardiac overload, and higher rates of encephalopathy, due to the shunting of unfiltered blood10–12. Risks for complications are also associated with the procedure. They include vascular injuries to the carotid arteries or right atrium, bleeding, portal or caval perforations, and biliary duct injury. The incidence of those complications, along with TIPS infection, have been reported at less than 1%13. Thus, TIPS can be a safe “bridging” therapy that enables the treatment of refractory symptoms until transplantation becomes available14. The aim of the present study was to compare operative time, operative bleeding, transfusions, intensive care unit (ICU) stay, and short-term survival in patients with TIPS prior to orthotopic liver transplantation (OLT) versus patients that only underwent OLT (OLT-only group).
We performed our study at a low-volume TIPS and OLT center.
Materials and methodsA retrospective review was conducted on patients that underwent liver transplantation at the Hospital San José Tec de Monterrey, since the program first began in 1999 until February 2020. Records for hospitalization, operative notes, and clinical data were reviewed for all patients. A total patient population of 92 was reviewed, of which 9 (9.8%) underwent TIPS prior to receiving the transplant. Clearance from the hospital ethics committee and patient consent were obtained for this study.
Transplants were distributed, according to the Mexican General Health Law, Article 336, which states that organ allocation is dependent on the receptor’s status, transplant opportunity, expected benefits, compatibility, and hospital location. Organs were recovered from donors after brain death in all cases and rapid extraction procurement with 4C in-situ portal and arterial preservation solution was carried out, followed by standard cold storage (Starzl). Wisconsin solution was used in the first 12 cases and histidine-tryptophan-ketoglutarate for all the remaining transplants. Whole liver transplantation was performed in all patients. The classic technique, with the aid of a venovenous bypass, was carried out in only one case, whereas a vena cava preservation technique was employed in the others. Biliary reconstruction was achieved via duct-to-duct anastomosis. All 9 TIPS placements were performed by the same interventional radiologist. Procedures were carried out under general anesthesia, with ultrasound-assisted right internal jugular vein puncture. Guidewires were navigated to achieve selective hepatic vein catheterization and pre-shunt measures were obtained for portal, hepatic, and inferior vena cava vessels. Portograms were analyzed for circulation aberrations. Balloon dilation was performed before stent placement, changes in portosystemic pressures were recorded, and shunt patency was verified.
After the initial analysis, 1:3 propensity score (PS) matching was performed through a multiple stepwise regression of age, smoking status, and Child-Pugh grade. The resulting PSs for complications and mortality were used to select control cases from the OLT-only patient pool, using a nearest neighbor algorithm with a .05 clamp.
Statistical analysisDemographic and operative variables were included for the analysis. Kolmogorov-Smirnov tests were used to assess normality. Parametric testing was performed using the Student’s t test or the ANOVA test with the Tukey test, where applicable. Non-parametric testing was done through the Mann-Whitney U test or the Kruskal-Wallis test. The categorical variables were analyzed using the chi-square test or Fisher’s exact test and the results were expressed as percentages and frequency. SPSS version 23 (SPSS Inc. Chicago, IL) software was employed for the statistical analysis. P values < 0.05 were considered statistically significant. Overall mortality was utilized in both groups as a surrogate indicator of quality, excluding possible recurring late complications for post-transplantation. Given that the hospital is a regional referral center, patients with minor complications do not always receive treatment at our center. Patient status was verified prior to drafting the manuscript, and survival was analyzed using the Kaplan-Meier survival curves, with a 10-year cutoff point for inclusion in the analysis, to avoid bias from a bygone era. Complications including vascular anastomosis leaks, stenosis, thrombosis, and surgical site bleeding were considered vascular complications. Complications pertaining to biliary structures, such as strictures, biliary leaks, anastomosis fistula, cholangitis, or obstruction, were considered biliary complications. Survival was analyzed through a Cox regression and results were expressed as hazard ratio.
ResultsOverall patient dataA total of 92 patients were included in the study. The mean patient age was 52.05 years, with a standard deviation (SD) of 13.43 years. Sixty-six (71.7%) patients were male and 26 (28.3%) were female. Eighty-three (90.2%) of the patients underwent an OLT without TIPS, whereas 9 (9.8%) had TIPS placement before their OLT. In the TIPS + OLT group, ages ranged from 15 to 65 years. The most common indication for transplant in that group was nonalcoholic steatohepatitis (3 of the 9 patients), followed by alcoholic hepatitis and autoimmune hepatitis (each in 2 of the 9 patients). Further details are displayed in Table 1. The Child-Pugh scores were as follows: Class A in 6 patients (6.5%), Class B in 48 (52.2%), and Class C in 38 (41.3%). The 3 most common indications for liver transplant according to etiology were hepatitis C virus in 22 patients (23.9%), ethanol consumption in 22 (23.9%), and nonalcoholic steatohepatitis in 17 (18.5%). Detailed findings are displayed in Table 2.
Demographics and waiting times for patients with TIPS
| Case # | Sex | Age | Time between TIPS and OLT (days) | Diagnosis | Indication | Complications |
|---|---|---|---|---|---|---|
| 1 | M | 56 | 98 | NASH | Variceal Bleeding | Encephalopathy |
| 2 | M | 53 | 229 | AH | Variceal Bleeding | |
| 3 | F | 55 | 16 | NASH | Variceal Bleeding | |
| 4 | M | 49 | 23 | Cryptogenic | Ascites | |
| 5 | M | 44 | 52 | AH | Variceal Bleeding | |
| 6 | F | 56 | 534 | Autoimmune Hepatitis | Variceal Bleeding | Shunt Revision |
| 7 | M | 65 | 417 | Autoimmune Hepatitis | Variceal Bleeding | |
| 8 | F | 63 | 25 | Glycogenosis | Variceal Bleeding | |
| 9 | M | 15 | 183 | NASH | Ascites |
AH: alcoholic hepatitis; NASH: nonalcoholic steatohepatitis; OLT: orthotopic liver transplant; TIPS: transjugular intrahepatic portosystemic shunt.
Baseline patient characteristics
| Count n = 92 (%) | |
|---|---|
| Patient age (±SD) | 52.05 (13.43) |
| Male | 66 (71.7%) |
| Female | 26 (28.3%) |
| Procedure | |
| OLT-only | 83 (90.2%) |
| OLT + TIPS | 9 (9.8%) |
| Child-Pugh Class | |
| Child-Pugh class A | 6 (6.5%) |
| Child-Pugh class B | 48 (52.2%) |
| Child-Pugh class C | 38 (41.3%) |
| Child-Pugh and MELD scores | |
| Child-Pugh score | 9.29 (2.73) |
| MELD score | 16.49 (5.56) |
| Patient characteristics | |
| DM | 20 (29.9%) |
| Smoker | 21 (30.9%) |
| BMI | 27.37 (5.71) |
| Underlying diagnosis | |
| HCV | 22 (23.9%) |
| Alcohol use | 22 (23.9%) |
| Autoimmune hepatitis | 14 (15.2%) |
| NASH | 17 (18.5%) |
| Others | 17 (18.5%) |
| Operation-related information | |
| Operative time | 437.86 |
| Operative transfusion | 7.32 |
| Outcome | |
| Alive | 87 |
| Death during surgery | 5 |
| ICU | |
| ICU stay | 5.76 |
BMI: Body mass index; DM: Diabetes mellitus; HCV: hepatitis C virus; ICU stay: intensive care unit stay; MELD score: model for end-stage liver disease score; OLT-only: orthotopic liver transplant alone; OLT + TIPS: orthotopic liver transplant + transjugular intrahepatic portosystemic shunt.
The median age was 55 years (15-65) in the OLT-only group and 54 years (13-75) in the OLT + TIPS group. Child-Pugh scores averaged 9.33 (±2.79) in the OLT-only group and 8.5 (±0.577) in the OLT + TIPS group. The Model for End-Stage Liver Disease (MELD) scores averaged 16.4 (±5.557), 14.5 (±4.72), and 17.88 (±5.4) in the OLT-only, OLT + TIPS, and OLT-only matched groups, respectively. We found no statistically significant differences in the aforementioned parameters. Table 3 shows the results.
Preoperative and operative analysis
| Patient characteristics | OLT-only | OLT + TIPS | p value | OLT-only PS match 1:3 | p value |
|---|---|---|---|---|---|
| Patient age | 55 (15-65) | 54 (13-75) | p = 0.746 | 52 (13-75) | p = 0.937 |
| DM (20) | 17 (29.3%) | 3 (33.3%) | p = 0.806 | 10(37%) | p = 0.841 |
| Tobacco use (23) | 19 (32.2%) | 2 (22.2%) | p = 0.546 | 7(25.9%) | p = 0.824 |
| Child-Pugh class A (6) | 5 (6%) | 1 (11.1%) | p = 0.794 | 1(3.7%) | p = 0.690 |
| Child-Pugh class B (48) | 44 (53%) | 4 (44.4%) | * | 12(44.4%) | * |
| Child-Pugh class C (38) | 34 (41%) | 4 (44.4%) | * | 14(51.9%) | * |
| MELD score | 16.4 (±5.57) | 14.5 (±4.72) | p = 0.121 | 17.88 (±5.4) | p = 0.548 |
| Child-Pugh score | 9.33 (±2.79) | 8.5 (±0.577) | p = 0.794 | 10.45(4.03) | p = 0.437 |
| Operative time (min) | 420 (360-600) | 420 (255-690) | p = 0.887 | 390 (360-450) | p = 0.557 |
| Operative transfusion | 6.1 (±4.36) | 3.7 (±1.89) | p = 0.774 | 8.25 (±6.21) | p = 0.877 |
| Death during surgery (5) | 5 (6%) | 0 (0%) | p = 0.214 | 0 | – |
| Vascular complications (7) | 7 (8%) | 0 (0%) | p = 0.115 | 3 (21.4%) | p = 0.273 |
| Biliary complications (16) | 14 (17.1%) | 2 (22.2%) | p = 0.700 | 7 (25.9%) | p = 1.0 |
| Early reintervention (22) | 20 (25%) | 2 (22.2%) | p = 0.855 | 10/27 (37%) | p = 0.685 |
| ICU stay (days) | 4 (1-7) | 3 (0-48) | p = 0.449 | 5.5 (1-30) | p = 0.910 |
DM: diabetes mellitus; OLT: orthotopic liver transplant; PS: propensity score; TIPS: transjugular intrahepatic portosystemic shunt.
Data presented as mean ± standard deviation, median (min-max) or n (%).
Patient characteristics are displayed depending on OLT-only, OLT with TIPS and OLT-only 1:3 match.
The average operating time for OLT in our population was 437.86 minutes. An average of 7.32 blood products was used. ICU stay averaged 5.76 days. Five patients (all in the OLT-only group) died during surgery. Population findings are further displayed in Table 3.
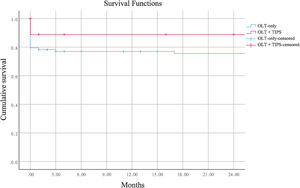
Postoperative data (by groups)The median length of stay in the intensive care unit was 4 (1–7) days in the OLT-only group versus 3 (0-48) days in the OLT + TIPS group. Twenty (25%) of the OLT-only patients had early reintervention versus 2 (22.2%) in the OLT + TIPS group (p = 0.855). In addition, the OLT-only PS-matched population resulted in 10 (37%) early reinterventions (p = 0.685). Vascular complications were reported in 7 (8%) patients in the OLT-only group, in 0 patients in the OLT + TIPS group (p = 0.115), and in 3 (21.4%) (p = 0.273) in the OLT-only PS-matched group. Biliary complications were found in 14 (17.1%) cases in the OLT-only group, 2 (22.2%) in the OLT + TIPS group (p = 0.700), and 7 (25.9%) (p = 1) in the OLT-only PS-matched group. Similar survival rates were identified, when comparing the TIPS group with the non-TIPS group, over the past 10 years, with a hazard ratio of .339 (0.5, 2.29) (p = 0.367). Those findings are displayed in Fig. 1.
Discussion and conclusionsTIPS decompression of portal circulation helps alleviate symptoms by normalizing portal pressure. It is not a definitive treatment but has long been used as a bridge to transplantation15. Its physiologic and anatomic effects have been thoroughly described, and prior studies have analyzed its impact on operative outcomes. The reduction in portal pressure is theorized to lead to reduced portosystemic collaterals and portal vein engorgement, which would translate into less operative risk, bleeding, and transfusions. The presence of those 3 factors have previously been associated with negative clinical outcomes by some authors, albeit with conflicting evidence16–19. Some of the complications described also result in higher resource use15. The intrahepatic nature of the shunt enables its removal in situ with the liver, with no additional maneuvers, but some studies describe extrahepatic migration of the stent or its creeping into the main portal vein, hepatic venous outflow, inferior vena cava, or mesenteric vein, resulting in intraoperative complications18,20. Thus, there are authors that categorize TIPS as a risk factor for surgical complications. The exact incidence of those complications and their actual impact has yet to be accurately described15.
Questions have been raised as to the extrahepatic benefits of TIPS, such as improvements in glomerular filtration rate and a consequent decrease in the MELD score, which could lead to inpatient classification inequality. Mumtaz et al. noted in their study that lower MELD scores associated with TIPS could lead to unequal transplant opportunities, with longer waiting times in equally decompensated patients8,21. Table 3 describes the waiting times for our cohort. Even with the benefits TIPS brings, the increased waiting time, the associated risk for infection, and failing liver function may prove to be counterproductive22. However, Casadaban et al. concluded that disease progression, even with TIPS, as reflected in the MELD score, is similar to patients without TIPS, suggesting that it does not significantly impact transplant candidacy23. In fact, Unger et al. noted there was no difference in 5-year survival between patients with TIPS without transplant and those that were transplanted. Both groups performed similarly, with respect to operating times and reinterventions24. In some studies, TIPS itself is suggested to be a high-mortality procedure, showing a 30-day mortality rate of up to 44%25. Further studies could dive deeper into waiting times in low volume settings and assess whether TIPS results in prolonged waiting times. A similar study in Vienna by Unger et al. found no impact on waiting times for patients that underwent pre-transplant TIPS in their setting24.
Other alternative therapies, such as surgical portosystemic shunts, achieve the same effect and prior studies have shown increased operative times due to adhesions, modified anatomy, and required TIPS reversal16,26. Our study found that vascular effects were insufficient for decreasing intraoperative transfusion requirements, but did not result in the previously described complications that lengthened operative times. The same was true for other associated variables, such as hospital stay and interventions, leading to the conclusion that TIPS can be safely undergone before transplant without positively or negatively affecting operative outcomes. In 2019, a total of 8,372 livers were transplanted in the United States27. Mexico, however, has a much lower transplantation volume. Official 2019 figures show that only 223 liver transplants were conducted nationwide, and of those, just 62 were performed at private institutions; 5 of them at our low-volume institution2.
To the best of our knowledge, our cohort is the first to describe outcomes in patients with TIPS + OLT, compared with patients that underwent OLT-only, at a low-volume center for both transplant and TIPS procedures in a developing country. While the information provided by our study might be useful for centers with similar scenarios, undoubtedly our study’s biggest limitation was the small size of the group of patients with TIPS. Further studies could include detailed reporting on both long-term and short-term complications, other than overall mortality.
In conclusion, TIPS placement continues to provide adequate bridge therapy for patients with recurrent ascites or refractory variceal bleeding, with safe operative results. In both developed and developing countries, the resources of surgeons, staff, and operating rooms are finite, and TIPS has no greater impact on their use than OLT-only procedures do. Its equal need for transfusion, operative time, and ICU stays shows it is an adequate tool, with no administrative costs during transplantation or effect on patient safety. Further studies on similar cohorts and in centers with similar volumes could further confirm such findings.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
We would like to thank the Comité de Investigación Clínica/Cirugía for its support.
See related content in DOI: 10.1016/j.rgmxen.2023.04.003, Transjugular intrahepatic portosystemic shunt safety inpatients on the liver transplantation waiting list. Risksand benefits. Rev Gastroenterol Mex. 2024;89:1–3.