Prolapsing mucosal polyps of the colon are an uncommon finding during colonoscopy. However, when present, those lesions, which are a form of colonic polyps, are frequently unrecognized and misdiagnosed as neoplastic lesions, sometimes leading to unnecessary endoscopic or surgical resection.
We present herein a case of symptomatic prolapsing mucosal polyp of the colon. We also reviewed the clinical, endoscopic, and histopathologic characteristics, as well as the potential management, of that entity.
A 62-year-old woman with no relevant past medical history was referred to our outpatient clinic for resection of a polypoid lesion, previously detected during colonoscopy, that was located in the sigmoid colon. She had a 6-month history of nonspecific gastrointestinal symptoms consisting of constipation and abdominal bloating. Physical examination revealed mild abdominal tenderness in the left lower quadrant upon palpation. Laboratory tests were within normal range.
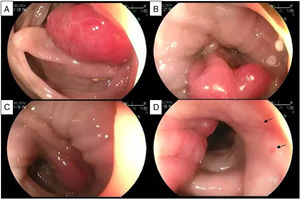
At flexible rectosigmoidoscopy, we found a 2cm, lobulated, bright, hyperemic mass projecting into the lumen of the sigmoid colon, with the morphologic characteristics of a polyp (Paris Ip – pedunculated polyp). It had a broad stalk with normal surrounding mucosa, as shown in fig. 1. We also observed a spastic colon and associated sigmoid diverticula. Hot snare polypectomy was performed.
Sequential images of the endoscopic appearance of a prolapsing mucosal polyp. A) Lobulated, bright, hyperemic mass. B) Obliteration of the lumen and long-standing spasm are present, showing a prolapsing mucosal polyp with a broad stalk. C) Retraction of the prolapsing mucosal polyp that continues with redundant mucosal folds. Notice the transition from congestive hyperemic mucosa to normal-looking surrounding mucosa. D) Lateral aspect of the lesion showing the redundant mucosal folds with petechiae (arrows).
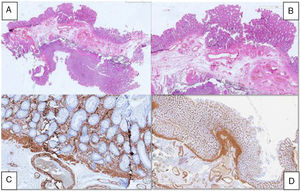
The pathology analysis of the resected lesion, as shown in fig. 2, identified glandular crypt abnormalities and a thickened muscularis mucosae, with fibromuscular obliteration of the lamina propria, all of which are characteristic features of a prolapsing mucosal polyp.
The patient was treated with a high-fiber diet, reporting symptom resolution, along with normal bowel movement frequency and stool consistency.
Prolapsing mucosal polyps are the result of chronic prolapse of the intestinal mucosa. They have been described in patients undergoing colonoscopic evaluation as large redundant hyperemic mucosal folds that mimic the appearance of a polypoid mass projecting into the lumen of the sigmoid colon. Due to under-recognition or misdiagnosis of said lesion, its true prevalence at endoscopic evaluation is unknown.
Prolapsing mucosal polyps form part of the spectrum of lesions called “mucosal prolapse syndrome”. That term was proposed in 1977 by Du Boulay et al. to encompass a variety of disorders with similar clinical and histologic characteristics.1 The proposed conditions that make up part of the so-called mucosal prolapse syndrome include solitary rectal ulcer syndrome,2–4 gastric antral vascular ectasia,5 inflammatory cloacogenic polyps,4 inflammatory”cap” polyps,6 and prolapsing mucosal polyps,6 all of which share similar histologic features.7
Prolapsing mucosal polyps have been described to occur in the sigmoid colon in association with diverticular disease.7,8 The exact mechanism leading to the formation of a prolapsing mucosal polyp is uncertain. However, in patients with a long history of defecation straining, a combination of venous congestion and mucosal redundancy secondary to repeated colonic spastic contractions is the most probable mechanism.8–10 In the largest case series available, Tendler et al.11 reported on 15 patients with prolapsing mucosal polyps in the sigmoid colon, describing their clinical, endoscopic, and histologic features. Occult gastrointestinal bleeding, hematochezia, cramping abdominal pain, and altered bowel habits were the most frequent presenting symptoms. The main endoscopic features were the presence of hyperemic polyps and prominent redundant folds with petechiae, all involving the sigmoid colon. The most frequently encountered histopathologic findings were glandular crypt abnormalities (hyperplasia, branching, elongation, distortion) in 100%, fibromuscular obliteration of the lamina propria in 93%, hypertrophy and extension of fibromuscular tissue into the lamina propria in 87%, and mucosal capillary abnormalities (congestion, hyalinization, thrombosis, dilation) in 87%.
Common differential diagnoses in patients with prolapsing mucosal polyps are adenomatous polyps, malignancy, ulcerative colitis, and hemangiomas. To the best of our knowledge there are no reports of malignant transformation of prolapsing mucosal polyps.
Currently, there is no consensus on the standard treatment of prolapsing mucosal polyps. Some reports have shown that conservative management based on a high-fiber diet results in a significant regression of those hyperemic polypoid lesions.10 Their clinical significance lies in the fact that they may be responsible for recurrent/persistent overt or occult bleeding and/or obstructive symptoms, settings in which surgical resection is a reasonable option. Long-term follow-up studies are needed to establish the significance and appropriate management of said hyperemic polypoid lesions.
Based on the best available data, endoscopists and pathologists should be familiarized with and recognize the characteristic features of prolapsing mucosal polyps, to prevent the morbidity and related costs of unnecessary endoscopic follow-up, polypectomy, or surgical resection.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Monreal-Robles R, González-González JA, Benavides-Salgado DE, Maldonado-Garza HJ. Pólipo prolapsado de mucosa: una forma de pólipo del colon que no debe ser olvidada. Revista de Gastroenterología de México. 2019;84:407–409.