A bezoar is an accumulation of organic substances within the gastrointestinal tract. Rapunzel syndrome is a rare and infrequent form of a trichobezoar with a tail that extends beyond the stomach into the small bowel.
We present herein the case of a 10-year-old girl referred to our center for abdominal pain. The patient had a past history of trichophagia of several-week progression, chronic abdominal pain, unmeasured weight loss, and predominantly postprandial nausea and gastric vomiting for the past 7 days.
Upon physical examination, the patient was dehydrated, with generalized pallor, abdominal distension, and a palpable and painful mass in the epigastrium.
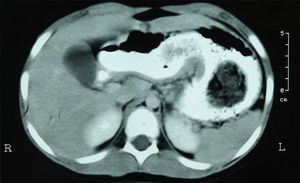
Laboratory work-up reported hemoglobin of 8.7g/dl (12-15g/dl), hematocrit of 26.9% (36-46%), leukocytes 9,250/mm3 (5,000-10,000/mm3), and platelets 274 x 103 mm3 (150-400/mm3). The rest of the laboratory tests were normal. Computed tomography scan identified an intragastric tumor extending into the duodenum that had no contrast medium enhancement (Fig. 1).
Exploratory laparotomy revealed a large intraluminal mass in the stomach. After gastrotomy, a large trichobezoar was found that extended into the small bowel, and it was removed. The patient did not present with any postoperative complications and was released on the 6th day after the procedure (Fig. 2).
Following the medical-surgical treatment, the patient was diagnosed with depressive disorder, anxiety syndrome, and poor self-esteem. She was initially treated at the medical psychology service and later referred to the pediatric psychiatry service at another center for her integrated treatment.
Rapunzel syndrome was first described by Vaughan in 1968. Since then, fewer than 100 cases have been described in the medical literature, with varying clinical characteristics. Different authors have used different criteria for reporting their cases of Rapunzel syndrome. Some have defined it as a gastric trichobezoar with a tail extending to the ileocecal valve, others have described it simply as a trichobezoar with a long tail that can extend into the jejunum, ileum, or ileocecal valve, and still others have defined it as a trichobezoar of any size that presents with bowel obstruction.1
Trichobezoar, a hairball in the proximal part of the gastrointestinal tract, is a rare condition and is seen almost exclusively in young women. Human hair is resistant to digestion and peristalsis because of its smooth surface, and thus accumulates in the folds of the stomach mucosa. After a period of time, the continued ingestion of hair results in its impaction, together with mucus and food, causing the formation of a trichobezoar. In the majority of cases, it is confined to the stomach. Nevertheless, in some cases, the trichobezoar extends beyond the pylorus into the jejunum, ileum, and even the colon.2
Patients with bezoars usually present with nonspecific gastrointestinal symptoms, such as abdominal pain, anorexia, and vomiting. Severe complications can occur, including obstruction, bleeding, or perforation.3
The most common presentation characteristics are abdominal pain (37%), nausea and vomiting (33%), obstruction (25%), and peritonitis (18%). Although not very common, patients can also present with weight loss (7%), anorexia, hematemesis, and intussusception (7%). The majority of patients deny any past history of trichotillomania or trichophagia, even when specifically asked. Therefore, psychiatric evaluation and management is recommended.1
Diagnostic studies include ultrasound, tomography, and panendoscopy. Computed axial tomography has a high accuracy rate, but ultrasound precision is not as high in these cases. Computed tomography reveals a well-circumscribed lesion in the gastric region composed of concentric spirals of different densities with air bubbles mixed up inside them. Oral contrast medium fills the most peripheral interstices of the lesion and a thin band of contrast medium circumscribes it. The absence of filling upon intravenous contrast medium-enhancement rules out a neoplastic lesion.4
Endoscopy plays the most important role in gastric bezoar detection, as well as in treating some of them. Tomography is useful for detecting small gastric bezoars and those in the small bowel. A tomography scan is particularly valuable in patients that need surgical management of small bowel bezoars, not only because it shows the obstructed site in the bowel, but also because it enables multiple bezoars to be observed.5
Conservatively managed cases have a poor prognosis and therefore surgical management is recommended once the preoperative diagnosis has been made. However, the majority of cases are diagnosed during laparotomy. Surgical removal through gastrotomy and enterotomy is suggested when necessary.1
Laparoscopic management can be successful for extracting a hairball. Other minimally invasive modalities are emerging, such as extracorporeal lithotripsy, endoscopic lithotripsy, and laser fragmentation. Their role and success rate still need to be established and at present the criterion standard is open surgical management.4
In our case, the patient presented with clinical symptoms of abdominal pain and weight loss, and with a known past history of trichotillomania. The diagnosis of Rapunzel syndrome was made after seeing the results of the computed axial tomography scan. It was decided that endoscopy would not add any new information to the diagnosis and given that the patient presented with symptoms of bowel obstruction and extension of the trichobezoar into the small bowel, the first choice for management was surgical rather than endoscopic.
Even though Rapunzel syndrome is the rare presentation of a trichobezoar that extends through the stomach and into the small bowel, it should always be included in the differential diagnosis in children that present with abdominal pain, vomiting, or weight loss. A previous history of trichophagia is essential for diagnostic suspicion.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Beristain-Silva JL, Cordero-Barberena R, Beristain-Hernández JL. Síndrome de Rapunzel: una causa rara de dolor abdominal. Revista de Gastroenterología de México. 2016;82:178–179.