We read the consensus on hepatic encephalopathy (HE)1 with great interest. However, we would like to comment on aspects of the utility of measuring serum ammonia in this disease.
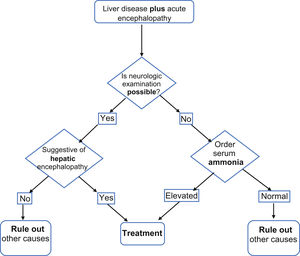
Differential diagnosisCritically ill patients hospitalized with chronic liver disease can develop the complication of HE. Making the diagnosis can be challenging, given that ∼50% of patients in the emergency room or intensive care unit are on invasive mechanical ventilation, with infusion of opioids and/or sedatives, or in coma, impeding neurologic examination. Encephalopathy in those patients could occur due to other common causes, such as delirium, sepsis, shock, meningitis/encephalitis and hypo/hypernatremia.
Prospective cohort studies, such as the one by Gundling et al.,2 have shown the utility of serum ammonia in the diagnosis of HE. In their study, serum ammonia levels >65.5 µg/dl correlated well with the West Haven criteria and critical flicker frequency (area under the curve = 0.71 and 0.861, respectively) in patients with cirrhosis.
Nicolao et al.3 found that levels of arterial ammonia >173.6 µg/dl and venous ammonia >121 µg/dl had a high correlation for diagnosing HE (r = 0.76).
In patients with acute-on-chronic liver failure (ACLF), Verma et al.4 showed that a serum ammonia level >132 mmol/l is an independent risk factor for the presence of HE at admission (OR 1.007, CI 1.004–1.010; p = –0.001) and during hospitalization (OR 1.002, CI 1.001–1.003; p = –0.001).
Given the above, we consider that determining serum ammonia could be useful for making or ruling out the diagnosis of HE in the settings described (Fig. 1), with the low cost of the test being its greatest advantage: ∼$200 MXN (∼$10.8 USD).
PrognosisIn patients with ACLF, elevated levels of serum ammonia are associated with HE progression (OR 1.002, CI 1.001–1.004; p = –0.011), as well as disease severity.4 Chiriac et al.5 observed that a venous ammonia level > 152.5 μmol/l was a good mortality predictor (area under the curve = 0.886). In a recent multicenter, prospective study on patients with cirrhosis, Shalimar et al.6 reported that serum ammonia correlated with HE severity and levels were significantly higher in patients that died (93 vs 67 µmol/l, p ≤ 0.001). In addition, a higher serum ammonia level was an independent risk factor for 28-day mortality (HR 1.009, p ≤ 0.001). Levels > 79.5 µmol/l were associated with a greater incidence of organ failure, and no decrease by day 5 was associated with a higher mortality rate.
In contrast to that recommended by the authors,1 the latest update from the European Association for the Study of the Liver strongly recommends determining the serum ammonia level in patients with delirium and/or encephalopathy associated with liver disease.
In conclusion, we assert that serum ammonia quantification is an inexpensive test that could be considered in critically ill patients with acute or chronic liver disease and encephalopathy, particularly in scenarios with numerous differential diagnoses.
Author contributionMEPP: Conceived the idea of the manuscript, contributed to the information search and the drafting and submission of the manuscript
ORPN: Conceived the idea of the manuscript, contributed to the information search and the drafting of the manuscript
NNHV and EDT: Reviewed the manuscript
TOML: Reviewed the manuscript and contributed to the drafting
Ethical considerationsNeither informed consent nor approval from the Bioethics Committee of the Hospital General San Juan del Río, Queretaro, was required for formulating the present document.
Because it is a letter to the editor, no cases or data of any patients or participants were presented and no interventions on animals were performed.
Conflict of interestAll the authors declare they have no conflict of interest.
Please cite this article as: Phinder-Puente ME, Pérez-Nieto OR, Hernández-Velázquez NN, Mondragón-Labelle TO, Deloya-Tomas E. Utilidad del amonio sérico en encefalopatía hepática en pacientes hospitalizados graves. Rev Gastroenterol Mex. 2023;88:455–456.