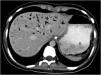
A 16-year-old female (BMI 16.8 kg/m2) sought medical attention due to epigastric abdominal pain, nausea, and vomiting of food, in addition to weight loss of 19 kg in 10 months from avoidant/restrictive food intake disorder. At hospital admission, her complete blood count, blood chemistry, and urinalysis test results showed no significant abnormalities. An abdominal CAT scan with contrast was ordered and revealed gastroduodenal distension with a transition zone at the level at the third portion of the duodenum due to compression of the superior mesenteric artery (SMA) (Fig. 1), gastric emphysema at the level of the major curvature, and portal pneumatosis (Fig. 2). A nasogastric tube was placed. Twenty-four hours after admission, endoscopy with CO2 was performed, finding subepithelial bleeding in the antrum and stomach body, with gastric necrosis, edema, and fibrin at the fundus. There was no extrinsic compression of the duodenum and a nasojejunal tube was advanced for enteral nutrition (Fig. 3). The patient was managed conservatively and had satisfactory clinical progression, tolerating oral intake at 7 days of treatment. A new CT scan was ordered that showed the absence of portal gas, and the patient was released from the hospital to undergo psychiatric and nutritional follow-up. Wilkie syndrome is caused by acute angulation of the SMA (6° to 22°) with a reduced aortomesenteric distance (2 to 8 mm) and has been associated with significant weight loss (Fig. 4). Hepatic portal venous gas is an ominous radiologic sign, associated with abdominal diseases that can be life-threatening (75% mortality). In the case described herein, gastric overdistension due to duodenal vascular compression resulted in gastric necrosis and embolization of intraluminal gas into the portal vein.
Multidetector computed tomography scan with intravenous and oral contrast (A and B), in the simple phase (C and D). A) Arterial phase, showing coronal view with important gastric distension that dissolved the contrast. B) Sagittal view, with dilatation of the first and second portion of the duodenum, with a sudden change of intestinal segment caliber. C) Axial view, showing a distance of 74 mm between the superior mesenteric artery (*) and the aorta (AA). D) Sagittal view, showing a 14 ° angle between the superior mesenteric artery (*) and the aorta (AA).
The authors declare that this work contains no information that could identify the patient and guarantees the right to privacy and preservation of anonymity of the patient. No experiments were conducted on humans or animals.
Financial disclosureNo financial support was received in relation to this article.