Actinomyces spp. are Gram-positive facultative anaerobic bacteria that form part of the normal flora of the oropharynx, the gastrointestinal tract, and the female genital tract.1,2 The microorganisms are opportunistic pathogens when there is disruption of the mucus membranes after inflammation, trauma, surgery, or use of an intrauterine device.3 The location of up to half of the cases is cervicofacial, followed by a 20% frequency of abdominal location.4
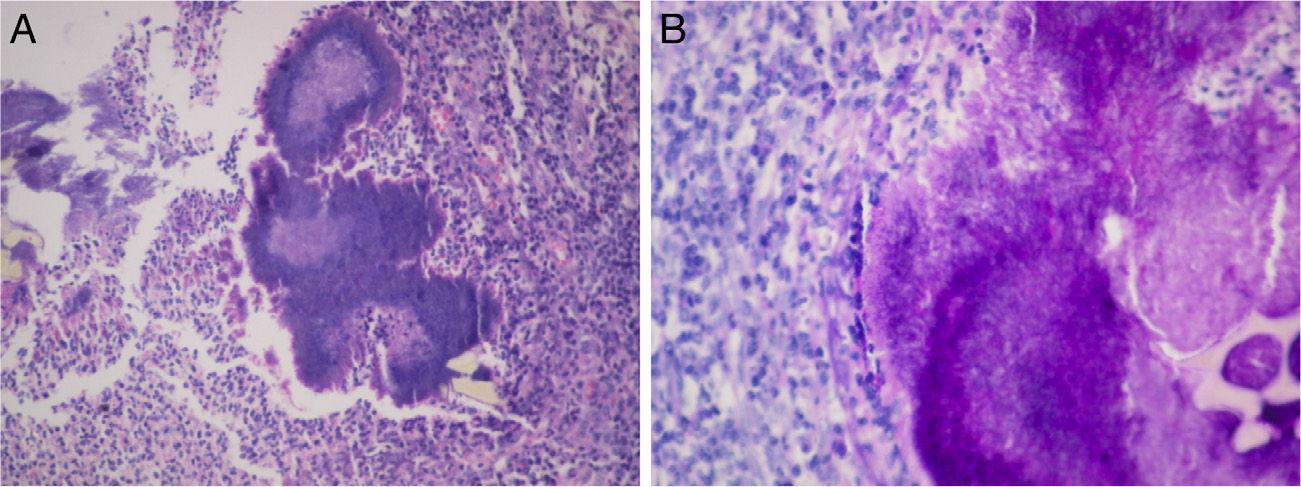
We present the case of a 58-year-old woman that sought medical attention for abdominal pain in the right flank of 2-month progression, changes in bowel habit with constipation, and a 5kg weight loss. Upon admittance her vital signs and laboratory tests were within normal limits. During physical examination a mass in the right iliac fossa was detected that was slightly painful upon palpation; there were no peritoneal irritation data. A strictured lesion in the cecum was encountered through colonoscopy. Biopsies were taken that only revealed nonspecific chronic inflammation. An abdominal tomography scan identified a 5cm tumor at the level of the cecum with thickening of the wall in the terminal ileum and the cecum, along with adenopathies (fig. 1). Because there was clinical suspicion of neoplasia, the patient underwent a laparoscopic right hemicolectomy. The intraoperative finding was peritumoral adenomegalies larger than 1cm. During macroscopic examination, a cecal appendix measuring 5 x 1.5cm was observed with thickened walls and fibroadipose obliteration of the lumen, along with a poorly delineated abscess-like lesion in the cecum. A pericecal abscess with extensive Actinomyces spp. colonization, «sulfur granules», and acute and chronic inflammation were viewed during the histopathologic study (fig. 2). Given these findings, 4-month therapy with amoxicillin plus clavulanic acid was begun. Postoperative progression was satisfactory and the patient was released 4 days after the surgery. Actinomycosis is a chronic suppurative disease that presents with the formation of fistula, sinus, inflammatory pseudotumor, or abscess. These are the characteristics that make it necessary to consider inflammatory bowel disease, inflammatory pelvic disease, and tuberculosis in the differential diagnosis. The infection can simulate malignancy due to its capacity to invade adjacent tissue and form masses.4–6 Up to 80% of the cases occur in women and 60% are associated with the use of an intrauterine device.2,4 The appearance of manifestations can take from months to years, given that the actinomycetes are slow-growing.1,2 Symptoms are nonspecific and in the majority of cases laboratory tests do not show abnormalities. Among the findings are normochromic anemia, leukocytosis, and increased globular sedimentation velocity. 2,7 Macroscopic examination of the surgical specimen of this case revealed inflammation at the level of the appendix. Actinomyces are normally found in stagnation zones, such as the cecum and appendix, the organs most frequently involved in the abdominal location.1,4,5 Early diagnosis of the acute appendicitis and opportune antibiotic therapy reduce the incidence of perforation, which is why inoculation through this inflammatory process is rare. Dissemination is mainly a result of tissue continuity; the hematogenic or lymphatic routes are less frequent, and so the presence of regional adenopathy is uncommon or is of late development.1,8 The peritumoral adenopathies in the present case made us suspect neoplasia as a first diagnostic possibility. The presentation of actinomycosis as a colonic mass suggestive of malignancy is infrequent (1%).4 Edema and mucosal ulceration can be found during colonoscopy, as well as umbilicated nodules, and in some cases, stricture. Contrast-enhanced tomography reveals extramural involvement and focal thickening of the colonic wall.9 Diagnosis through endoscopic or fine needle aspiration biopsies is complex, given that Actinomyces filaments are surrounded by widespread inflammation.5 Although preoperative diagnosis is useful for avoiding extensive resection, up to 96% of cases require surgical diagnosis. Through surgical management, the necrotic tissue is removed, fistulas are corrected, and the duration of antimicrobial treatment is reduced.3,4,10 Colonoscopy and tomography play an important role in the therapeutic follow-up. «Sulfur granules» are observed in the histopathologic study and they react to the Schiff and Grocott stains. Culture is complex and can be negative in up to 76% of the cases.5 The Actinomyces species is difficult to identify and the specific agent could not be recognized in our case. Nevertheless, they are susceptible to aminopenicillins and the combination with β-lactamase inhibitors should be considered first-line therapy. No disease recurrence is found after 4 months of treatment.10
In conclusion, actinomycosis should be included in the differential diagnosis of infiltrating tumors in the right colon, emphasizing the fact that in the majority of cases laboratory tests are normal and there are no adenopathies. A mass with attenuated focal areas invading adjacent structures is a characteristic finding in tomography scans. Even though Actinomyces normally reside in the appendix, there are few reports in the literature of cases in which appendicitis is the abdominal inoculation mechanism.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Blanco-Vela CI, Luna-Ayala VM, Perez-Aguirre J. Tumoración colónica secundaria a actinomicosis. Presentación de un caso y revisión de la literatura. Revista de Gastroenterología de México. 2014;79:206–208.