A 77-year-old woman came to the emergency department presenting with abdominal pain of 48-h progression that initially was epigastric and then became generalized. Her other symptoms were pain in the center of the chest with dyspnea, nausea with no vomiting, and a progressively deteriorating general health status; as the hours progressed, her level of consciousness began to diminish. She had an important history of iron deficiency anemia that was treated with oral iron.
Upon arrival she presented with hypotension (blood pressure 76/60mmHg), tachycardia (121 bpm), tachypnea (27rpm), and desaturation (SaO2: 89%). The first examination revealed a distended and tympanic abdomen with diffuse pain upon palpation and obvious signs of generalized peritoneal irritation. Nasogastric tube placement was unsuccessful. Blood analysis showed elevated levels of C-reactive protein and procalcitonin - 110mg/l and 282 ng/ml, respectively -, leukopenia (1,200 l/ml), acute renal failure (urea of 69mg/dl and creatinine of 1.68mg/dl), and hypoxemia with compensated metabolic acidosis. Electrocardiogram results showed no signs of acute myocardial ischemia.
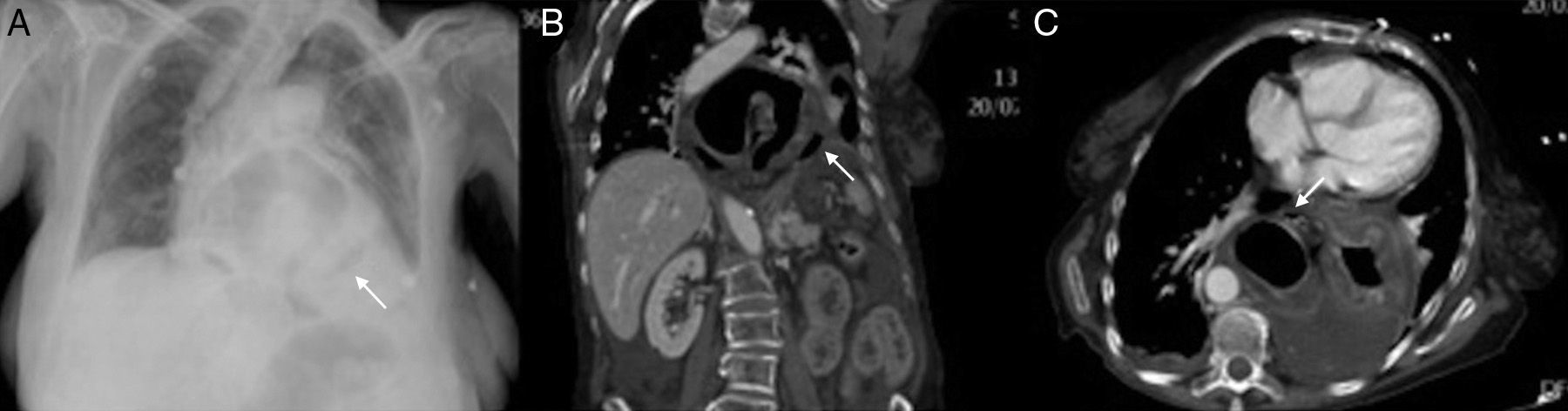
A plain chest x-ray taken with a portable machine showed a large hiatal hernia with probable stomach protrusion and an image of paragastric gas (suggesting pneumoperitoneum) (fig. 1A). Crystalloid and colloid resuscitation was begun due to the symptoms of shock, and once the hemodynamic parameters improved, an abdominal computed tomography scan was carried out (figs 1B and C); it revealed paraesophageal gastric herniation with organoaxial volvulus (intrathoracic disposition of the fundus and body with the gastroduodenal junction in the normal position); it also showed signs of ischemia in the gastric wall and perigastric ectopic gas bubbles.
Chest x-ray. A): Large hiatal hernia with a probably ectopic paragastric air bubble (black arrow). Left pleural effusion. CT: coronal (B) and axial (C) views: paraesophageal gastric herniation with organoaxial volvulus. Intrathoracic disposition of the fundus and body with normal location of the gastroduodenal junction. The herniated gastric walls present with concentric thickening due to edema and there is little contrast uptake due to ischemic damage. Multiple ectopic gas bubbles (white arrow) and fluid in the hernial sac due to visceral perforation are visible.
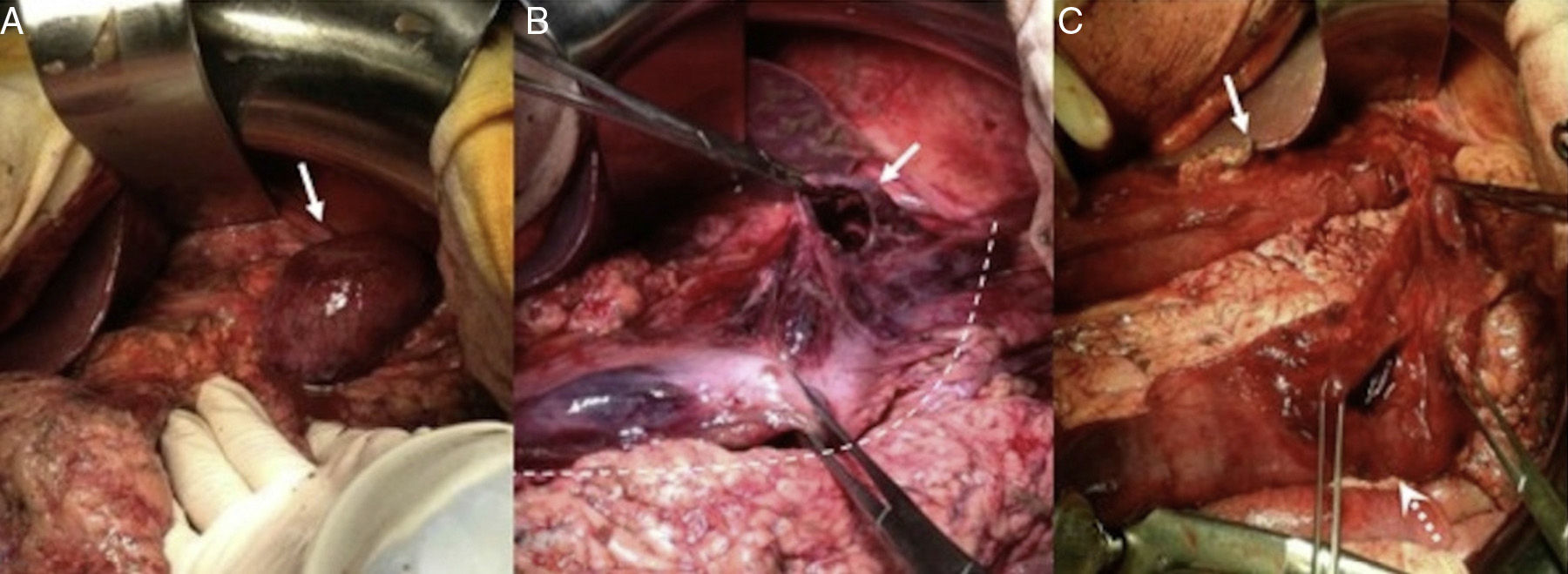
Emergency surgery was indicated and the patient underwent laparotomy through a midline incision that revealed diffuse peritonitis with abundant free fluid and a paraesophageal hernia with organoaxial gastric volvulus that presented with signs of ischemia in the entire greater curvature, as well as a 3cm perforation in the fundic portion of the curvature. Given the patient's situation (48-h symptom progression, the need for vasoactive drug perfusion from the start of the procedure, and the fact that the lesser curvature was apparently not involved), the entire cavity was thoroughly washed, the hernia was reduced, and atypical tubular gastrectomy was performed, extirpating practically the complete greater curvature. Gastropexy from the remnant to the diaphragm and its left pillar was then carried out (fig. 2).
Images of the surgery: A) After pushing back the left hepatic lobe, the paraesophageal hernia with the intrathoracic stomach and ischemic aspect can be observed (white arrow). B) After reducing the herniated stomach, ischemia affecting the greater curvature (white dotted line) and 3cm perforation at the level of the curvature in the gastric body (white arrow) is seen C) Tubular gastrectomy resecting the ischemic greater curvature and gastric perforation (white arrow shows gastric tubularization; dotted white arrow shows gastric resection)..
The patient was placed in the intensive care unit. She showed slight improvement and then within the first 24hours presented with hemodynamic deterioration that was refractory to catecholamines. Her previous respiratory and renal failure worsened, progressing to multiorgan failure and consequent death.
Paraesophageal hernias (PEH) are produced by a herniation of the gastric fundus through the diaphragm with the gastroesophageal junction (GEJ) in the normal position. They make up 5%1 of the hiatal hernias and are considered to be caused by a weakness in the pleuroperitoneal membrane that allows the anterior wall of the stomach to protrude between the esophagus and the phrenoesophageal ligament.2 Because of the position of the GEJ, these patients do not usually present with the typical symptomatology of gastroesophageal reflux disease, but rather seek medical attention due to dysphagia (resulting from esophageal compression by the herniated stomach), chronic anemia from mucosal bleeding, postprandial fullness, nausea, and vomiting.3 However, some patients remain asymptomatic or begin to present with the appearance of complications.
Acute PEH can be produced by gastric volvulus, incarceration, strangulation, massive bleeding, or perforation.4 Gastric volvulus is an infrequent entity, arising from a 180° rotation of the stomach over its own axis.5 Despite being described as a primary presentation, the majority of cases are secondary to other pre-existing pathologies (paraesophageal hernias, traumatism, etc.) In regard to the rotational axis, there are 2 types of volvulus: the organoaxial (60%), in which the stomach rotates over its longer axis, with the greater curvature in a cephalad direction and the lesser curvature in a caudal one; and the mesenteroaxial (30%), in which the rotation is over the shorter axis. The remaining 10% are mixed and undetermined forms.
Organoaxial volvulus is frequently (2/3 of the cases) secondary to PEH, traumatism, and eventration or diaphragmatic paralysis. In its acute form it can present with the classic Borchardt triad (epigastric pain, inability to vomit, and difficulty in placing the nasogastric tube),6 and constitute a surgical emergency due to its frequent association with strangulation as a result of the consequent vascular compromise.
The surgical treatment of choice in these cases includes hernial reduction, the resection of ischemic tissue (total or partial gastrectomy), and repair of the hernial defect, if there is one.7 Good results with laparoscopic approaches have been described for gastric volvulus in stable patients,8 but its use in cases of perforation is controversial.
In our case, the deterioration of the patient and the location of the perforation led to the decision to perform partial tubular gastrectomy associated with gastropexy. We felt this was the most adequate option for extirpating the ischemic tissue, maintaining the digestive transit, avoiding the performance of a gastrointestinal anastomosis and its potential complications, and preventing possible recurrence. The delay from the time of symptom onset to the diagnosis, together with the important subsequent clinical deterioration of the patient, conditioned the poor postoperative progression that resulted in her death.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Martínez-Pérez A, Garrigós-Ortega G, Gómez-Abril S, Torres-Sánchez T, Uceda-Navarro D. Vólvulo gástrico perforado por hernia paraesofágica incarcerada. Revista de Gastroenterología de México. 2014;79:204–206.