The formation of bezoars from indigestible materials can cause intestinal obstruction.1 A hemobezoar is an accumulation of blood residue in the intestinal lumen and is a rare complication of upper gastrointestinal bleeding. The majority of cases occur after bariatric procedures, in particular, in Roux-en-Y gastric bypass (RYGB) surgery. Hemobezoars can cause acute small bowel obstruction.2–5
A 92-year-old woman had a past medical history of chronic NSAID use. She arrived at the emergency department presenting with hematemesis, lethargy, dehydration, abdominal distension, nausea, and vomiting. The initial laboratory work-up showed Hb of 5.6g/dl, creatinine of 1.2mg/dl, and BUN of 38mg/dl. She underwent transfusion with three units of packed red blood cells and first received an 80mg intravenous (IV) bolus dose of omeprazole, followed by 40mg IV twice a day.
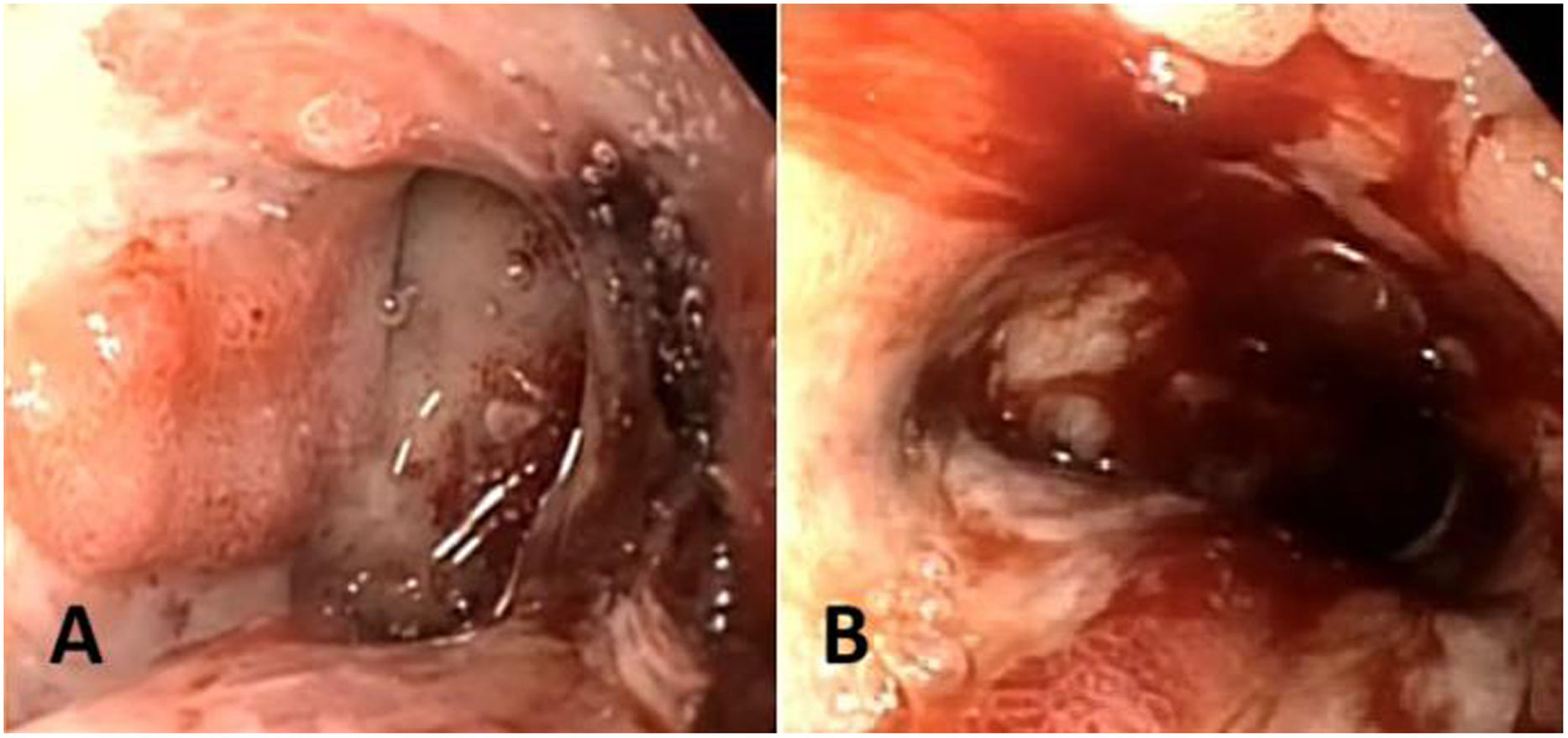
Upper endoscopy revealed a Forrest IIB duodenal ulcer (Fig. 1), which due to the complexity associated with its anatomic location, was treated only with removal of the attached clot and endoscopic adrenaline injection. Erosive gastritis and Los Angeles grade C esophagitis were also identified. Twenty-four hours later, the patient developed acute oral feeding intolerance, with a tendency toward low blood pressure. She showed neurologic signs of lethargy and presented with skin and mucous membrane dehydration, associated with a serum sodium level of 149mmol/l, oliguria with creatinine of 1.2mg/ dl, and BUN of 38mg/dl. She also presented with abdominal distension, epigastric pain, and multiple episodes of nausea and vomiting. Given that her hemoglobin level did not drop, and her clinical status did not worsen, suspected rebleeding was ruled out.
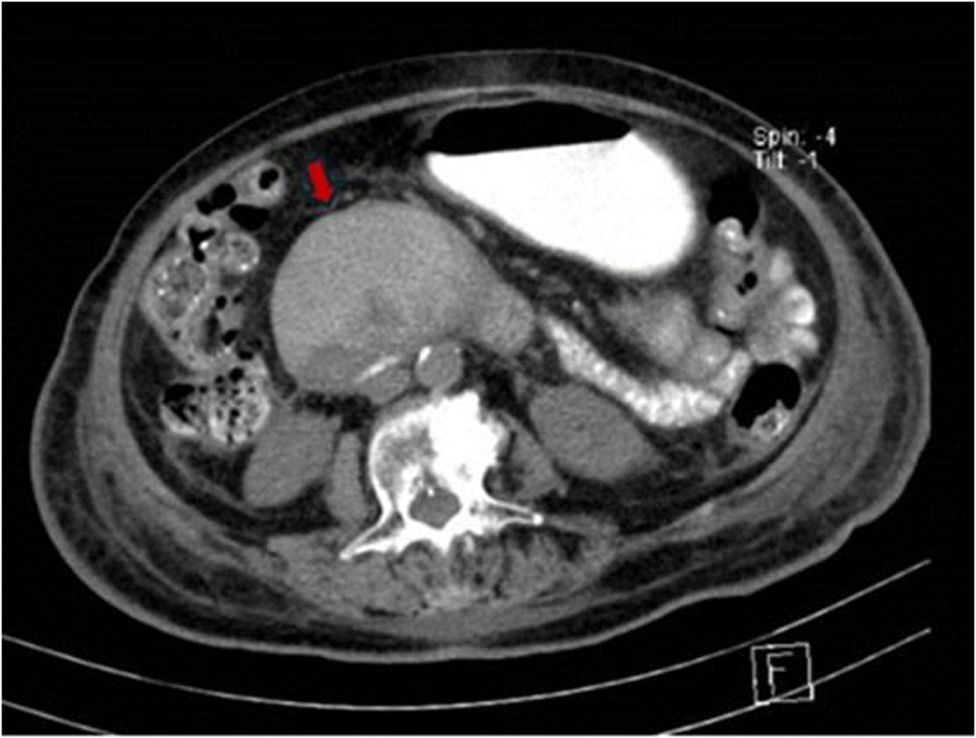
Additional evaluation was carried out by consulting with the internal medicine service. An abdominal computed tomography (CT) scan with oral contrast was ordered that revealed the presence of a hemobezoar in the second and third part of the duodenum, causing acute small bowel obstruction (Fig. 2).
The primary therapeutic approach consisted of hydration with crystalloid solutions, nasogastric tube placement, and intestinal lavage with a carbonated soda, with no success. The general surgery team suggested a surgical approach, but the patient and her relatives rejected it, and so conservative treatment through the placement of a nasojejunal feeding tube for enteral nutrition and the prevention of major obstruction was employed. Clinical improvement was achieved in two days, with the patient becoming hemodynamically stable and adequately tolerating the enteral nutrition tube. There were no signs of rebleeding, and so we decided to discharge the patient.
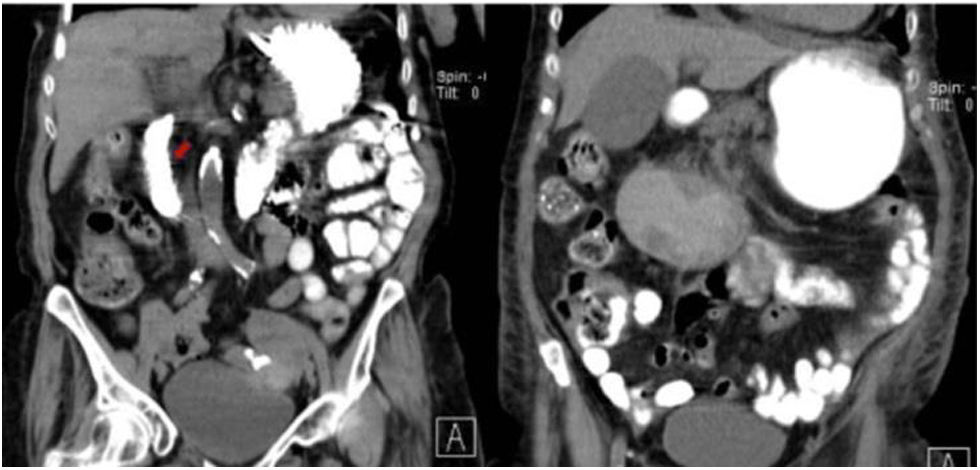
An abdominal CT scan with oral contrast was programmed for one month after her discharge and it showed that the duodenal obstruction had resolved (Fig. 3). The feeding tube was removed, and the patient remained under surveillance.
Our case is an example of successful conservative treatment of acute small bowel obstruction related to upper gastrointestinal bleeding, which can serve as a guide for physicians faced with similar cases. The main limitation of the present study is the fact that it describes only one case report, thus limiting its generalization.
Hemobezoars are a rare complication of upper gastrointestinal bleeding. The majority occur following bariatric procedures, specifically RYGB. They account for approximately 0.05 to 1.9% of small bowel obstructions in RYGB, causing the formation of intraluminal blood clots and intestinal obstruction in jejunostomy. Most cases are resolved through the laparoscopic approach and enterotomy.2–5 A recent case described acute intestinal obstruction from a hemobezoar after robotic gastric bypass surgery.6 In 2006, Groth et al.7 reported the first and only case of gastric outlet obstruction in the duodenum secondary to endoscopic sphincterotomy. Those authors found a large hemobezoar and unsuccessfully attempted its removal with a basket, scalpel, and polypectomy loop; a 16 F nasojejunal tube was placed in the proximal jejunum to prevent intestinal obstruction, which led to its resolution. Opting for conservative management and nasojejunal tube placement provided a successful result. Diagnostic abdominal CT and conservative treatment with a nasojejunal feeding tube can be a potential and safer option in such patients, especially those who are fragile and present with high surgical risks.
The present case report is the first documented appearance of acute intestinal obstruction related to a bleeding peptic ulcer and sets a precedent for the conservative treatment of those patients.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this article.
Ethical considerationsThe authors declare that the anonymity of the patient was maintained at all times during the preparation of this case report. In addition, we received the informed consent of the patient for the publication of the manuscript. The present work meets the current bioethical research regulations and was conducted in accordance with the knowledge and experience of the medical team. At no time was anything carried out for the sole purpose of publishing the report. Therefore, authorization from our institution’s ethics committee was not required.