Pulmonary embolism in patients with hepatocellular carcinoma (HCC) may result from tumor embolization, tumor thrombotic microangiopathy, or thromboembolism. The clinical presentation ranges from the asymptomatic to abdominal or chest pain, cough, hemoptysis, dyspnea, or ascites.
A 49-year-old man presented with esophageal variceal bleeding and was further diagnosed with metabolic dysfunction-associated fatty liver disease-related cirrhosis. He was subsequently referred to our center to investigate hepatic nodules detected on ultrasound. He was asymptomatic, with a Child-Pugh A5 classification, and a MELD score of 12. A contrast-enhanced computed tomography (CT) scan of the abdomen showed multinodular/infiltrative HCC, with a tumor thrombus inside the right hepatic vein, extending into the inferior vena cava (Fig. Fig. 1). In addition, emboli were identified in the lower lobe of the left lung on a chest CT scan (Fig. 2). Serum alpha-fetoprotein was 509 ng/ml, bone scintigraphy was unchanged, and transthoracic echocardiogram showed no neoplastic extension to the heart.
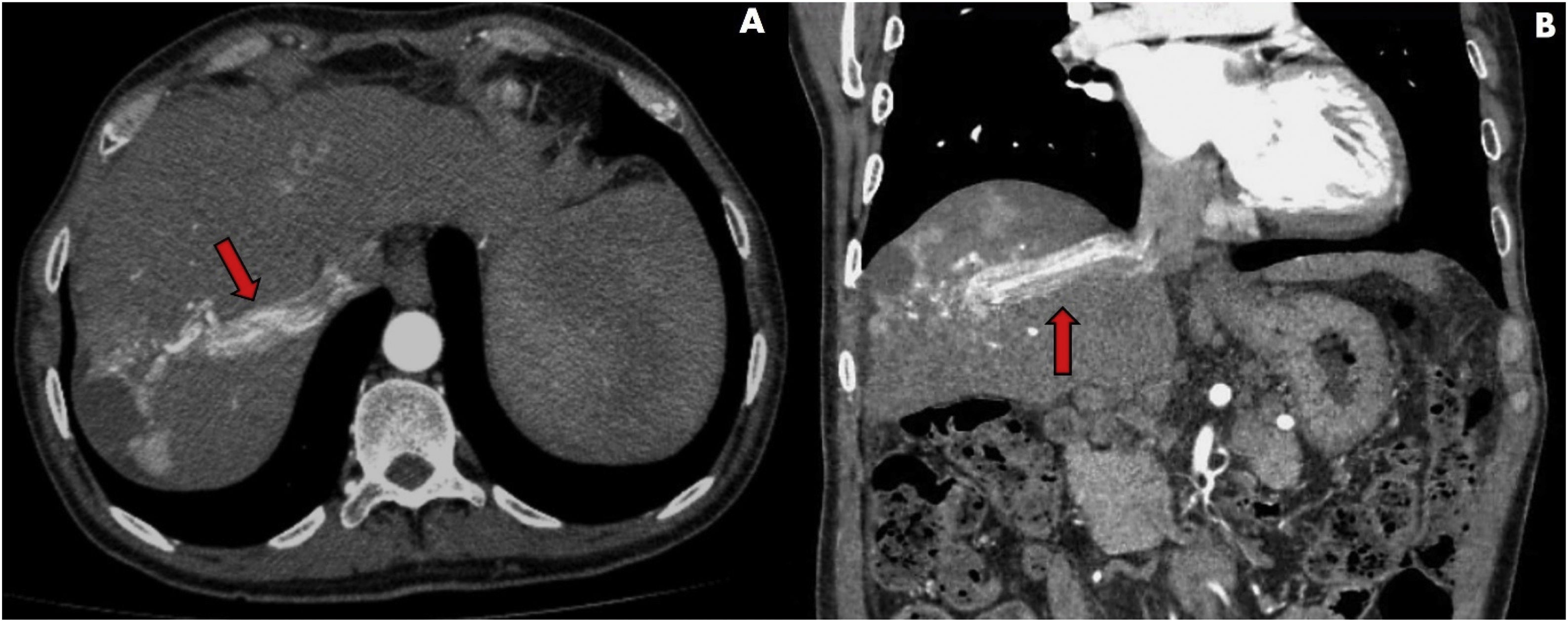
Computed tomography scan in the arterial phase: infiltrative and multinodular hepatocellular carcinoma with hypodense lesion between segments V/VIII measuring 60 mm at its largest diameter (necrosis). There is a contrast-enhanced thrombus within the right hepatic vein (red arrows) extending into the inferior vena cava. (A) Transverse plane, (B) Coronal plane.
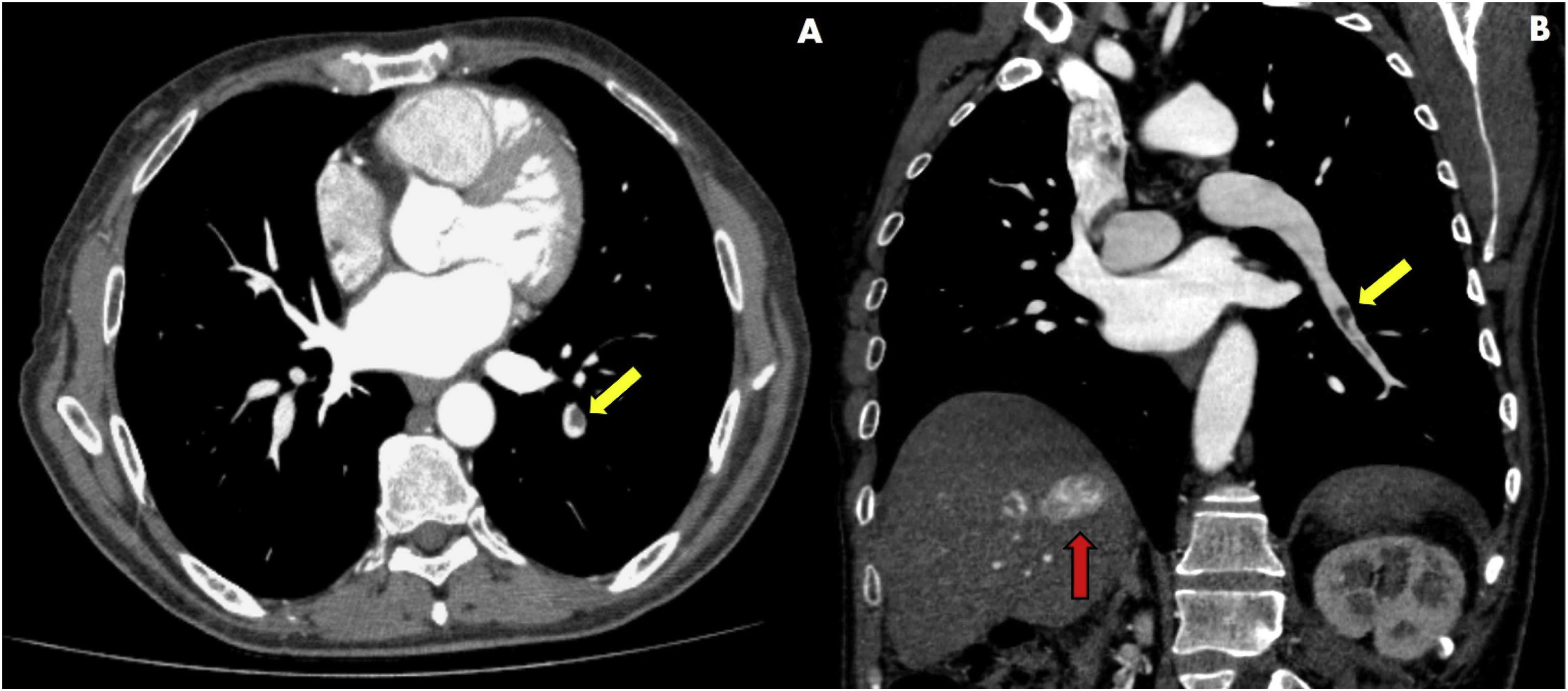
Computed tomography scan in the arterial phase. Yellow arrows show partial filling defects in the segmental arterial branches in the lower lobe of the left lung, corresponding to pulmonary embolism. There is no evidence of pulmonary metastasis. The red arrow reveals tumor thrombi within the right hepatic vein. (A) Transverse plane; (B) Coronal plane.
Tumor thrombus inside the inferior vena cava has been reported in less than 3% of patients with HCC and leads to worse survival. The patient’s lack of respiratory symptoms was possibly due to the involvement of only small pulmonary arterial branches, but migration of the thrombus could result in massive pulmonary embolism and death. Because he was in BCLC stage C, the patient was referred for systemic treatment with sorafenib, but was lost to follow-up. This report emphasizes the need to 1) look for HCC in all patients presenting with esophageal variceal bleeding as the first manifestation of cirrhosis, and 2) detect metabolic dysfunction-associated fatty liver disease in patients with advanced liver fibrosis to include them in HCC surveillance.
Ethical considerationsThis report was reviewed and approved by the Local Ethics Committee. The patient agreed to participate in the research and signed a written statement of informed consent, which is in the possession of the corresponding author. The authors declare that this article contains no personal information that could identify the patient.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Cunha-Silva M, Greca RD, Sevá-Pereira T. Carcinoma hepatocelular avanzado con trombosis tumoral de la vena cava inferior y embolia pulmonar. Rev Gastroenterol Méx. 2023;88:282–283.