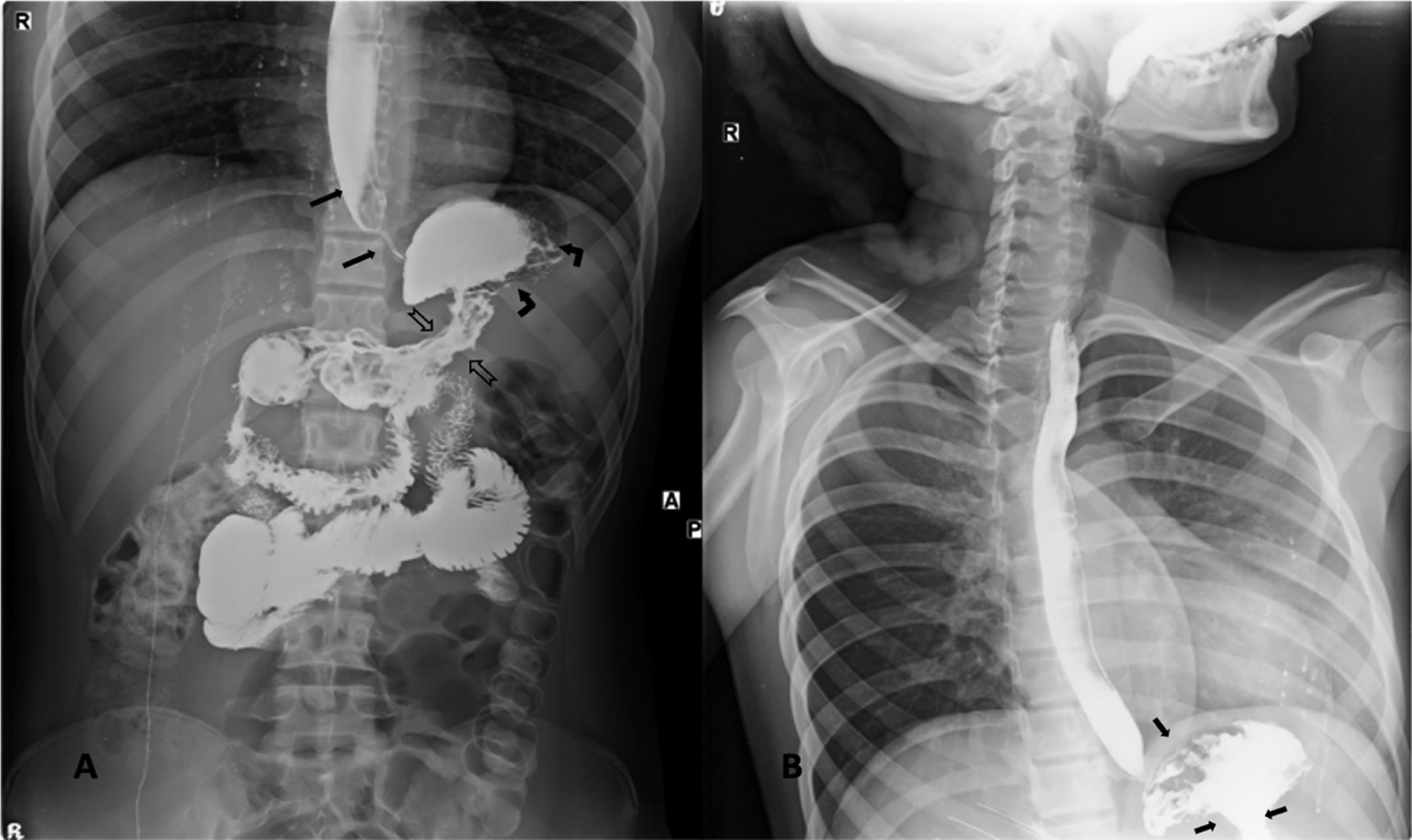
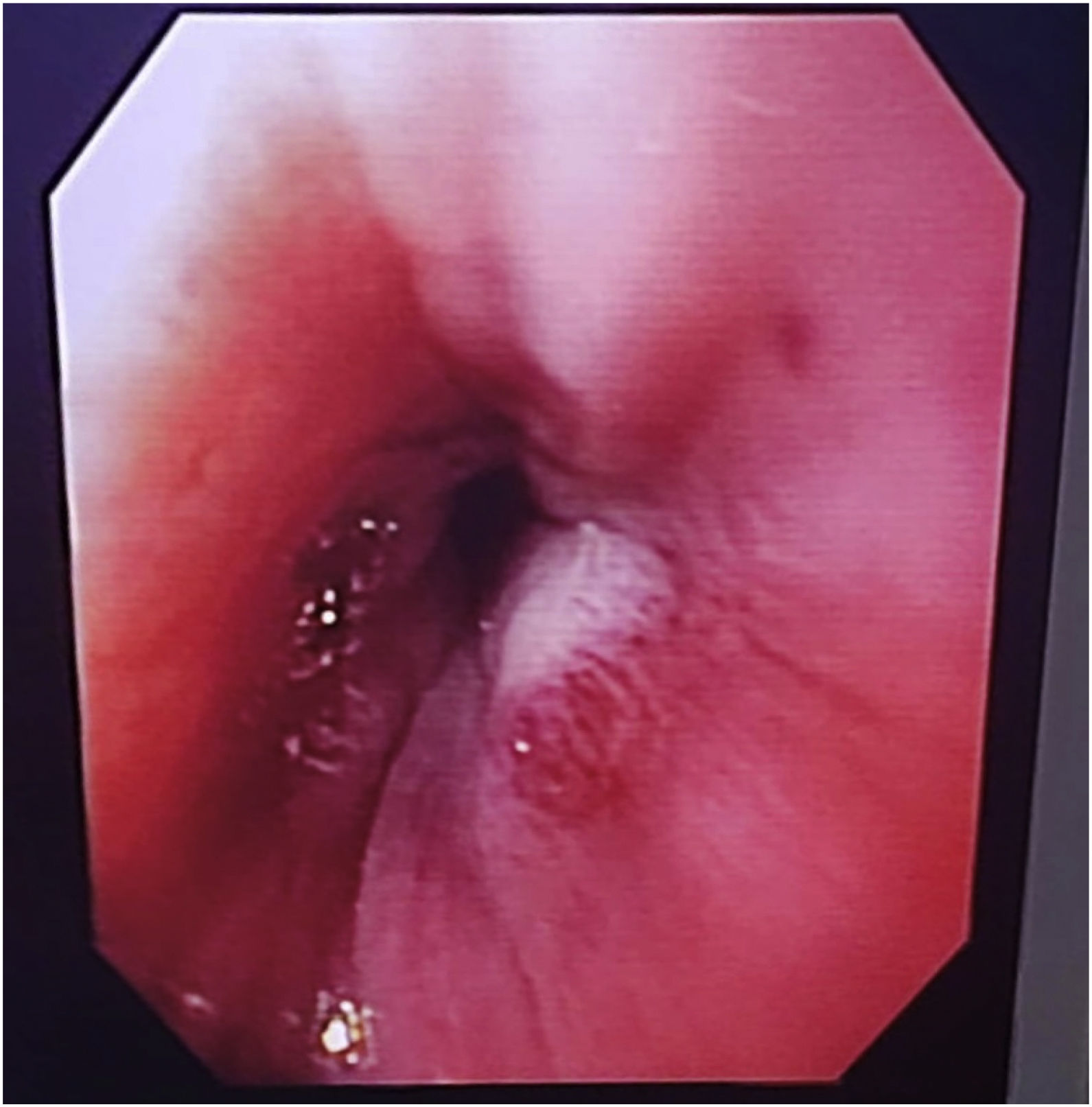
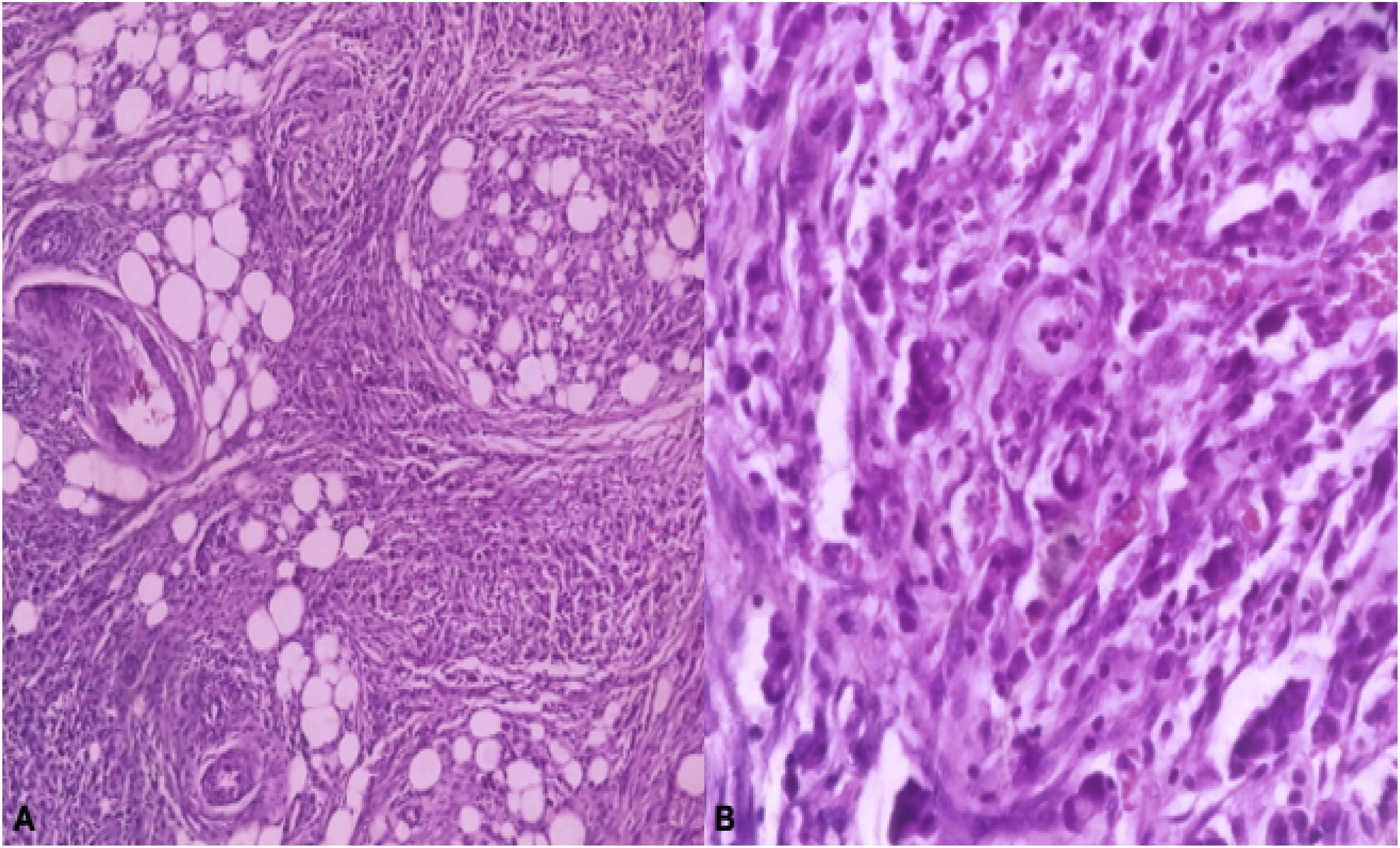
A previously healthy 18-year-old female came to the emergency department due to diffuse abdominal pain of 2-month progression, associated with nausea, vomiting, and weight loss of approximately 14kg. One month before hospital admission, she presented with dysphagia to solids. Her vital signs were normal. Physical examination of the abdomen identified no palpable masses or pain upon palpation. An abdominal ultrasound study revealed the presence of ascites. A barium swallow study (Fig. 1A and B) revealed a distal esophageal stricture (filiform and irregular passage of the contrast medium through the gastroesophageal junction) and marked gastric narrowing (linitis plastica). Esophagogastroduodenoscopy was performed, confirming the esophageal stricture; it impeded the passage of the endoscope (Fig. 2). Serology for Helicobacter pylori was negative. Tumor markers showed: CA 19-9: 928U/mL (reference value: <37U/mL), CA 125: 230U/mL (reference value: <35U/mL). Exploratory laparotomy revealed a markedly rigid stomach with a thickened wall, as well as multiple tumor implants in the omentum, small bowel, and colon. Palliative surgical treatment was carried out through a Stamm jejunostomy. Biopsy of the omentum revealed the presence of poorly differentiated adenocarcinoma (Fig. 3A and B). The patient was treated with chemotherapy and palliative care.
Barium swallow. A) Hollow arrows: marked narrowing of the gastric lumen (linitis plastica). Curved arrows: irregularities of the mucosa in the proximal part of the stomach with reduced distensibility. Long arrows: dilation of the middle esophagus with severe distal narrowing (pseudoachalasia) that produced filiform and irregular passage of the contrast medium through the gastroesophageal junction. B) Distorted gastric mucosal folds and stiff walls in the region of the body.
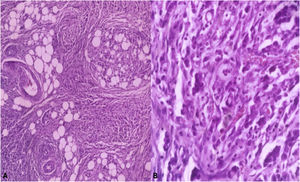
Biopsy of the omentum: poorly differentiated adenocarcinoma. A) H/E stain ×20. Soft tissues infiltrated by malignant neoplasm with epithelial appearance. B) H/E stain ×10. Poorly cohesive cells with infiltrating aspect, some with a plasmacytoid morphology, eccentric nucleus displaced by cytoplasmatic vacuoles. Images courtesy of Dr. María Cecilia Loredo (Pathology Department, Nuevo Hospital Monte España).
The authors declare that informed consent was obtained from the patient for the publication of this article. The present work meets the current bioethical research norms and was approved by the institutional Ethics Committee. The authors declare that this article contains no information that could identify the patient and guarantee the patient’s right to privacy and preservation of anonymity. No experiments were conducted on animals or humans.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Marín-López CA, Maltez AS. Seudoacalasia y linitis plástica. Rev Gastroenterol Méx. 2023;88:284–286.