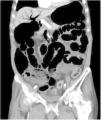
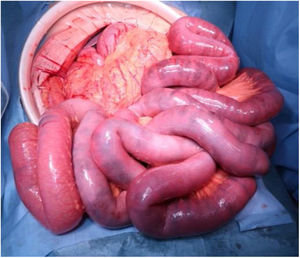
An 81-year-old man with a history of type 2 diabetes mellitus was admitted to our hospital because of abdominal bloating. He had started taking voglibose six days earlier. Physical examination showed abdominal distension, but no abdominal tenderness. Contrast-enhanced abdominal computed tomography revealed an expanded intestinal tract and portal emphysema (Fig. 1). Voglibose was suspended, and the patient underwent emergency laparotomy for suspected non-occlusive mesenteric ischemia. However, there were no signs of intestinal necrosis or perforation (Fig. 2). Bowel decompression was then performed. Computed tomography was carried out on the seventh day of hospitalization, showing no portal emphysema (Fig. 3), and oral diet was started on day 10. The patient’s clinical course was uneventful, and he was transferred to a long-term care hospital on day 24. Portal venous gas has been known to be a rare complication in patients taking alpha-glucosidase inhibitors (α-GIs) and could result from pneumatosis cystoides intestinalis, rather than intestinal ischemia.1,2 It can be managed conservatively, and unnecessary surgical treatment should be avoided.
Written informed consent was obtained from the patient for publication of this article. Because the present work is a case report, no authorization by the institution’s ethics committee was required.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe author declares that there is no conflict of interest.
The author wishes to thank S. Kawano for his support in daily clinical practice.
Please cite this article as: Ito H. Gas en vena porta inducido por inhibidor de alfa glucosidasa: no siempre es indicación para cirugía. Revista de Gastroenterología de México. 2021;86:307–308.