Chronic pancreatitis is a pathologic fibroinflammatory syndrome of the pancreas. Treatment includes medical management and endoscopic and/or surgical interventions. Our aim was to describe progression in patients with chronic pancreatitis whose initial management was either endoscopic or surgical.
Material and methodsA retrospective, analytic, observational, and longitudinal study was conducted that included patients diagnosed with chronic pancreatitis treated at the Hospital de Especialidades of the Centro Médico Nacional Siglo XXI from 2015 to 2021.
ResultsTwenty-two patients were included in the study; 12 underwent endoscopy and 10 underwent surgery. The mean number of interventions performed was 3 in the endoscopic management group and 1.1 in the surgical management group (p = 0.001). Regarding pain remission (partial or total), results were statistically significant in favor of surgical management (p = 0.035). Of the 12 patients that initially underwent endoscopy, 7 (58.3%) eventually required surgery during follow-up. There were no statistically significant differences with respect to opioid and pancreatin use, readmissions, weight loss, steatorrhea, newly diagnosed diabetes, or deaths during follow-up.
ConclusionPain is the main indication for invasive treatment, whether endoscopic or surgical, in patients with chronic pancreatitis. Slightly more than half of the patients that were initially managed endoscopically required surgery during follow-up. Management decisions should be multidisciplinary and individualized for each patient.
La pancreatitis crónica es un síndrome fibroinflamatorio patológico del páncreas. El tratamiento incluye manejo médico, e intervenciones endoscópicas y/o quirúrgicas. Nuestro objetivo fue conocer la evolución, entre los pacientes con pancreatitis crónica sometidos a cirugía y aquellos tratados por endoscopia de manera inicial.
Material y métodosEstudio observacional, retrospectivo, analítico y longitudinal, incluyendo a los pacientes con diagnóstico de pancreatitis crónica atendidos en el Hospital de Especialidades del Centro Médico Nacional Siglo XXI de 2015 a 2021.
ResultadosSe incluyeron 22 pacientes, 12 en el grupo endoscópico, y 10 para el grupo quirúrgico. El promedio de intervenciones realizadas fue de 3 para el grupo endoscópico y de 1.1 para el grupo quirúrgico (p = 0.001). En la remisión del dolor (parcial o total), se encontró significancia estadística a favor del manejo quirúrgico (p = 0.035). De los 12 pacientes que de manera inicial fueron tratados con manejo endoscópico, 7 (58.3%) eventualmente requirieron cirugía durante el seguimiento. No se encontraron diferencias estadísticamente significativas en cuanto uso de opioides y pancreatina, reingresos, pérdida de peso, esteatorrea, diabetes de reciente diagnóstico o mortalidad durante el seguimiento.
ConclusiónLa principal indicación para tratamiento invasivo ya sea endoscópico o quirúrgico en los pacientes con pancreatitis crónica es el dolor. Poco más de la mitad de los pacientes que fueron manejados endoscópicamente de manera inicial requirieron cirugía durante el seguimiento. La decisión de que manejo ofrecer debe de tomarse de manera multidisciplinaria, e individualizarse para cada paciente.
Chronic pancreatitis is a pathologic fibroinflammatory syndrome in individuals with genetic, environmental and/or other risk factors, who develop persistent pathologic responses to the parenchymatous lesion or to stress.1,2 The estimated incidence is 4–14 for every 100,000 persons per year. Alcohol abuse (>5 drinks/day) is the most important risk factor for its development (OR 3.1; 95% CI 1.87–5.14) and is present in 70% of adult cases.2,3
The most frequent manifestations are abdominal pain, occurring in more than 80% of patients, and steatorrhea. When approximately 90% of pancreatic function is lost, patients develop signs of exocrine dysfunction, such as steatorrhea, malabsorption, and liposoluble vitamin deficiencies. Likewise, due to the development of extensive fibrosis, patients can also develop endocrine dysfunction, presenting as pancreatogenic diabetes. Weight loss and malnutrition are frequent, resulting from fat malabsorption and anorexia related to pain.2–4
In the absence of medical therapies that modify the disease, management consists mainly of the detection and treatment of related complications. Approaches are medical, endoscopic and/or surgical. Patients with significant anatomic obstruction are candidates for endoscopic or surgical therapy. In general, medical therapy is recommended for patients with no pancreatic duct obstruction or for those with less intense pain.5 Around 30 to 60% of the patients that have uncontrolled pain with medical treatment will require invasive procedures, such as endoscopic or surgical interventions.6
Whether endoscopic treatment or a surgical intervention should be performed first, continues to be a subject of debate.7 At present, there is no high-quality evidence regarding invasive procedures1 but almost half of the patients with chronic pancreatitis will eventually require some type of surgical intervention for treating unresolved chronic pain after treatment with less invasive methods.6,8
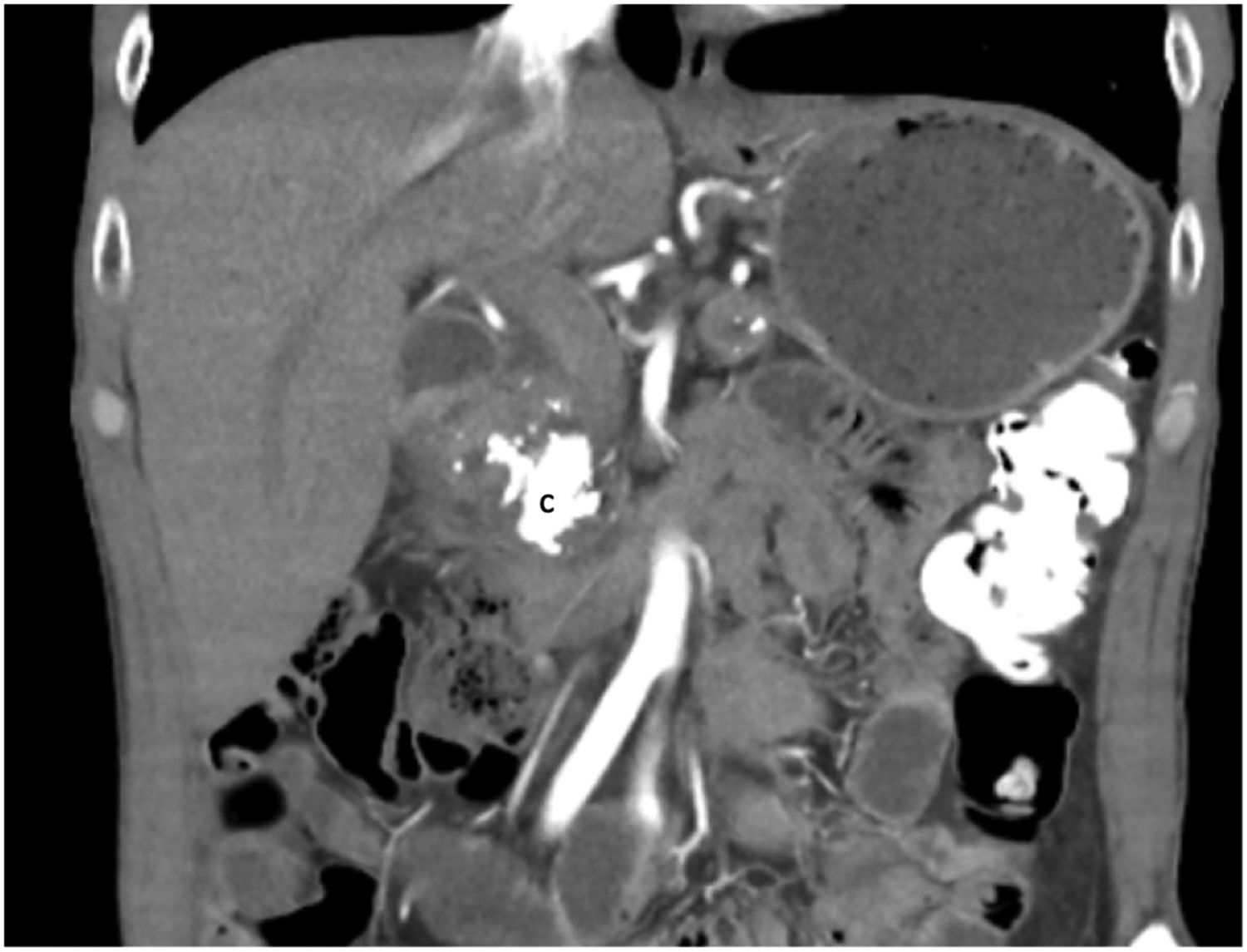
Endoscopy, surgical resection, and drainage procedures, or their combination, can be utilized to treat pain when medical therapies are not successful. Those procedures alleviate obstruction due to stones, stricture, or both, by attempting to reduce intraductal hypertension, and in turn, pain. The surgical procedures utilized included partial resection (e.g., Whipple procedure, distal pancreatectomy), drainage (e.g., Puestow procedure), and the combination procedures of partial resection and drainage (e.g., Frey, Berne, and Beger)4 (Fig. 1).
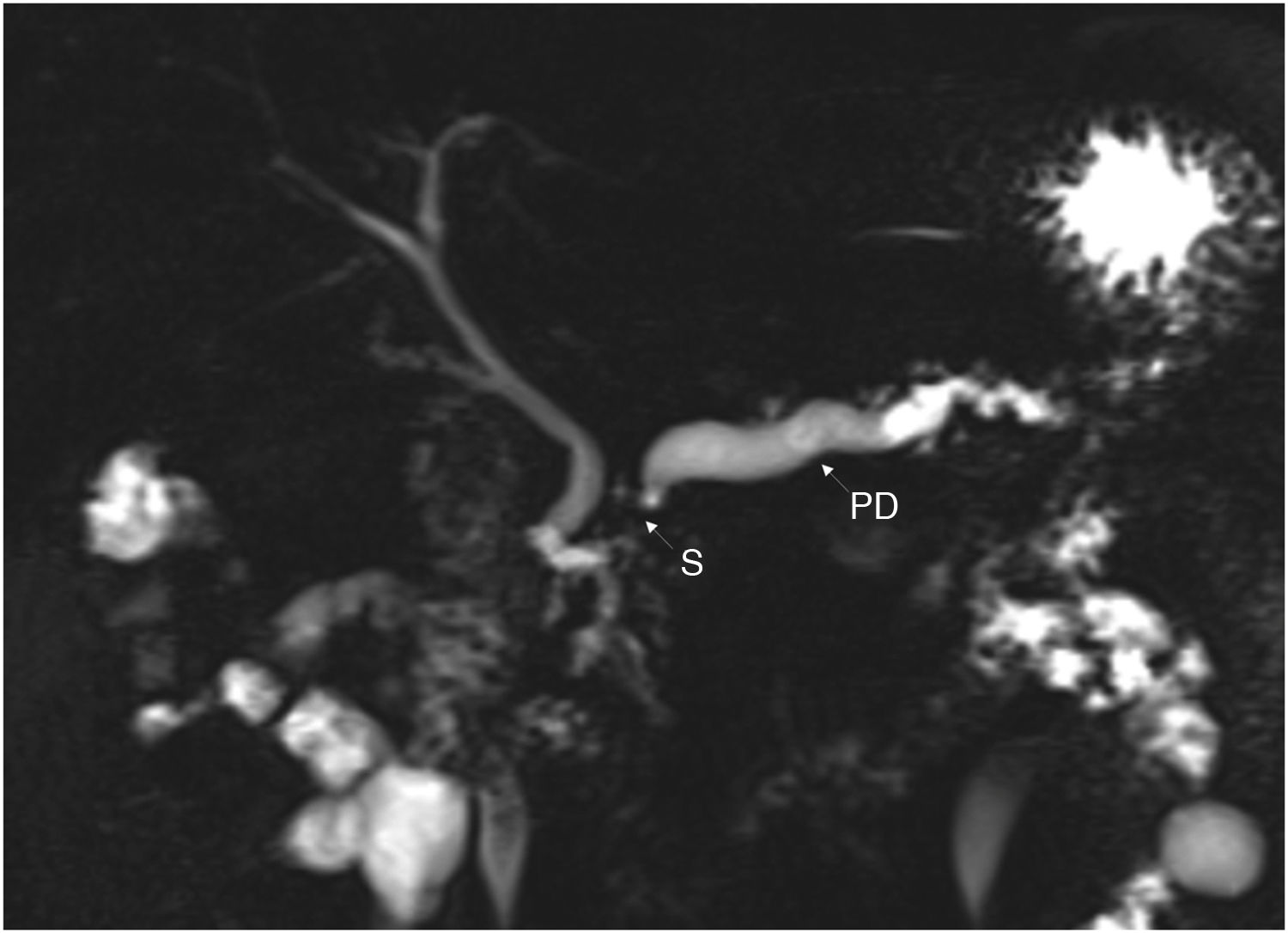
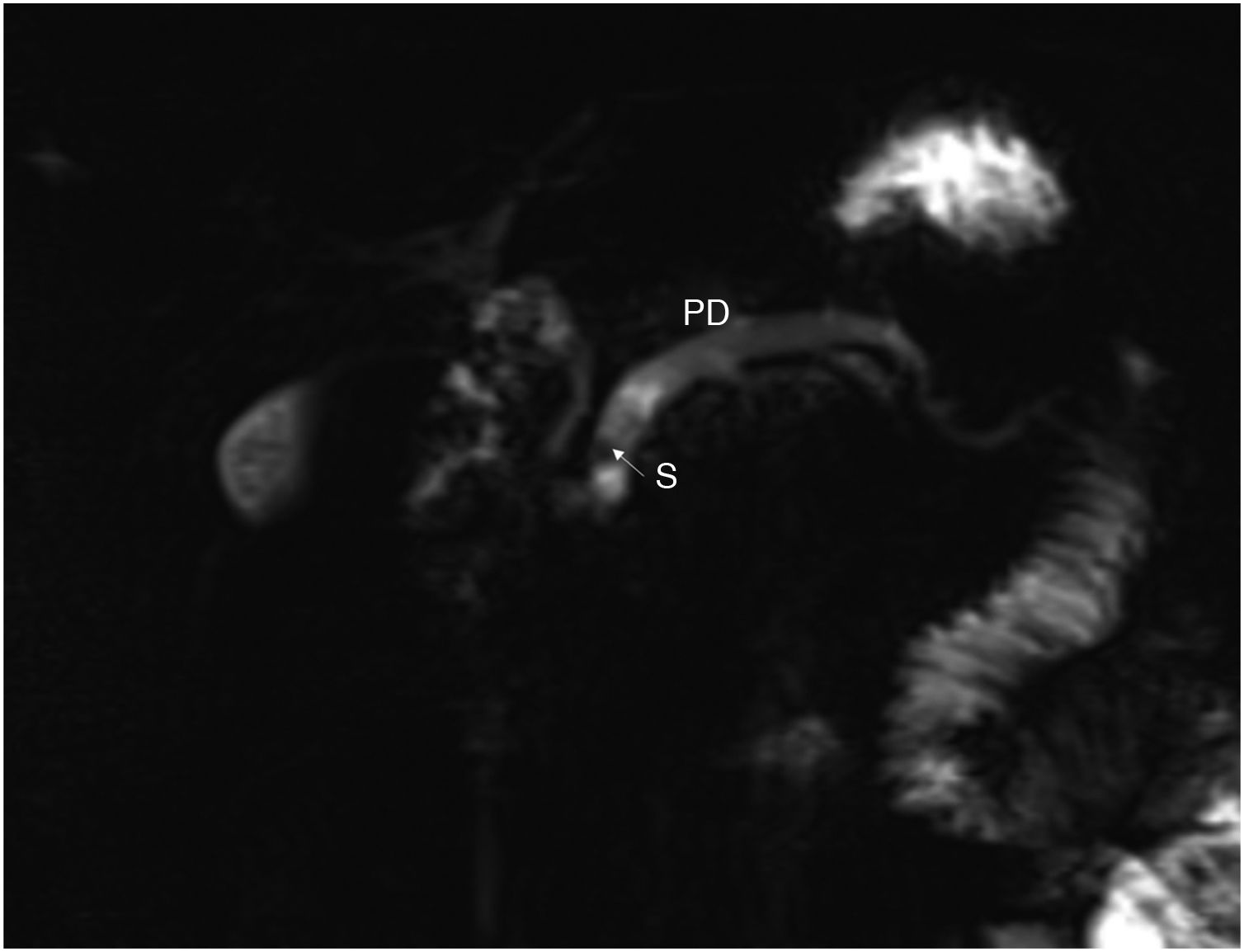
Endoscopic procedures include endoscopic retrograde cholangiopancreatography (ERCP)-guided procedures, such as pancreatic sphincterotomy, stent placement, stricture dilation, stone extraction, lithotripsy, and the endoscopic ultrasound (EUS)-guided procedures of pancreatic duct intervention and celiac nerve block6 (Figs. 2 and 3).
Our aim was to describe the progression of patients with chronic pancreatitis that initially underwent surgery and those that were initially treated through endoscopy.
Material and methodsA retrospective, analytic, observational, longitudinal study was conducted that included patients diagnosed with chronic pancreatitis at the Gastrosurgery and Gastroenterology Services that underwent surgical or endoscopic treatment at the Hospital de Especialidades “Dr. Bernardo Sepúlveda Gutiérrez” of the Centro Médico Nacional Siglo XXI of the Instituto Mexicano del Seguro Social, within the time frame of January 1, 2015, and December 31, 2021. Patients diagnosed with chronic pancreatitis whose anatomopathologic study revealed malignancy were excluded, as well as patients whose clinical records or follow-up at the unit were lost. Chronic pancreatitis etiology, initial treatment (endoscopy or surgery), the procedures performed, re-interventions, complications, and deaths were registered. For the result comparison, pain remission (partial or total), need for opioids to manage pain, need for pancreatin to manage exocrine pancreatic insufficiency, and the development of diabetes mellitus during follow-up were registered. All the data were collected from the clinical records of the patients. Sequential non-probabilistic sampling was carried out, including all the patients treated within the time frame of the study. Verification was carried out using the STROBE checklist.
Statistical analysisDescriptive and inferential statistics were carried out. Measures of central tendency and dispersion were obtained for the demographic variables. For the postoperative variables, groups were compared through parametric and nonparametric tests, utilizing the IBM SPSS Statistics 29.0 program.
Ethical considerationsThis study meets the current bioethical research regulations and was authorized by the institutional committees on health research and ethics of the Hospital de Especialidades “Dr. Bernardo Sepúlveda Gutiérrez” of the Centro Médico Nacional Siglo XXI, IMSS (CLIS 3601). Informed consent was not required for the publication of this study because it contains no personal data that could identify the patients.
ResultsTwenty-two patients were included in the study. Twelve of them (7 men and 5 women) received initial endoscopic treatment and 10 (9 men and 1 woman) underwent surgical treatment. Mean patient age in the group that had endoscopic management was 39.9 years (range 17−67), and 43.3 years (range 18−68) for the patients that initially underwent surgery. Regarding comorbidities, in the endoscopic management group, 5 patients had no associated disease, 4 were diagnosed with diabetes mellitus, one had high blood pressure, one had diabetes mellitus and high blood pressure, and one patient had polycystic ovarian syndrome. In the surgical management group, 7 patients had no associated disease, one was diagnosed with high blood pressure, one had diabetes mellitus and high blood pressure, and one patient had a history of lymphoma.
In the endoscopic management group, chronic pancreatitis etiology was recurrent acute pancreatitis in 7 patients (58%), alcohol use disorder in 2 patients (17%), obstructive disease in 2 patients (17%), and autoimmune disease in one patient (8%). In the surgical management group, the cause was obstructive disease in 4 patients (40 %), idiopathic disease in 4 patients (40%), and alcohol consumption in 2 patients (20%).
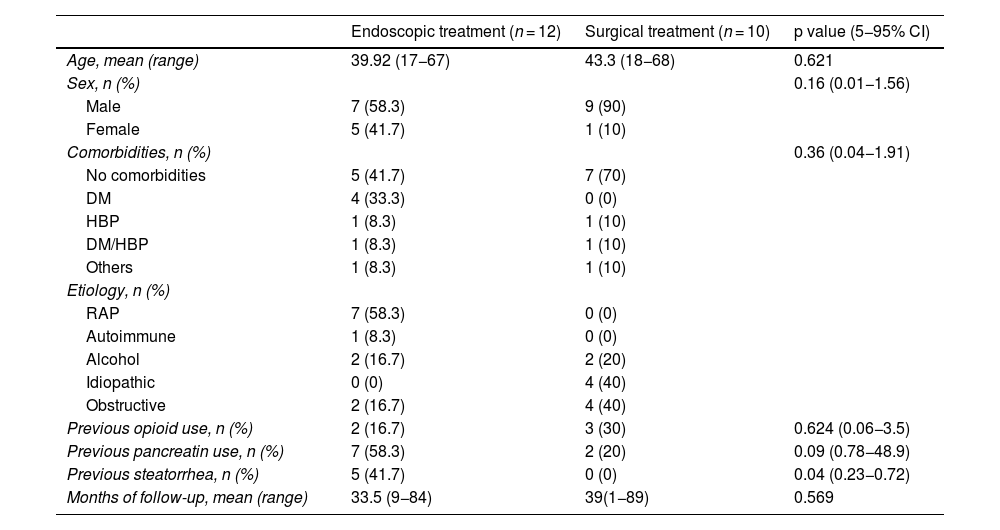
As part of the medical management of pancreatic disease, in the endoscopic management group, 2 patients (17%) received opioids and 7 patients (58%) received pancreatin. In the surgical management group, 3 patients (30%) received opioids and 2 patients (20%) received pancreatin (Table 1).
Demographic characteristics.
| Endoscopic treatment (n = 12) | Surgical treatment (n = 10) | p value (5−95% CI) | |
|---|---|---|---|
| Age, mean (range) | 39.92 (17−67) | 43.3 (18−68) | 0.621 |
| Sex, n (%) | 0.16 (0.01−1.56) | ||
| Male | 7 (58.3) | 9 (90) | |
| Female | 5 (41.7) | 1 (10) | |
| Comorbidities, n (%) | 0.36 (0.04−1.91) | ||
| No comorbidities | 5 (41.7) | 7 (70) | |
| DM | 4 (33.3) | 0 (0) | |
| HBP | 1 (8.3) | 1 (10) | |
| DM/HBP | 1 (8.3) | 1 (10) | |
| Others | 1 (8.3) | 1 (10) | |
| Etiology, n (%) | |||
| RAP | 7 (58.3) | 0 (0) | |
| Autoimmune | 1 (8.3) | 0 (0) | |
| Alcohol | 2 (16.7) | 2 (20) | |
| Idiopathic | 0 (0) | 4 (40) | |
| Obstructive | 2 (16.7) | 4 (40) | |
| Previous opioid use, n (%) | 2 (16.7) | 3 (30) | 0.624 (0.06−3.5) |
| Previous pancreatin use, n (%) | 7 (58.3) | 2 (20) | 0.09 (0.78−48.9) |
| Previous steatorrhea, n (%) | 5 (41.7) | 0 (0) | 0.04 (0.23−0.72) |
| Months of follow-up, mean (range) | 33.5 (9−84) | 39(1−89) | 0.569 |
DM: diabetes mellitus; HBP: high blood pressure; RAP: recurrent acute pancreatitis.
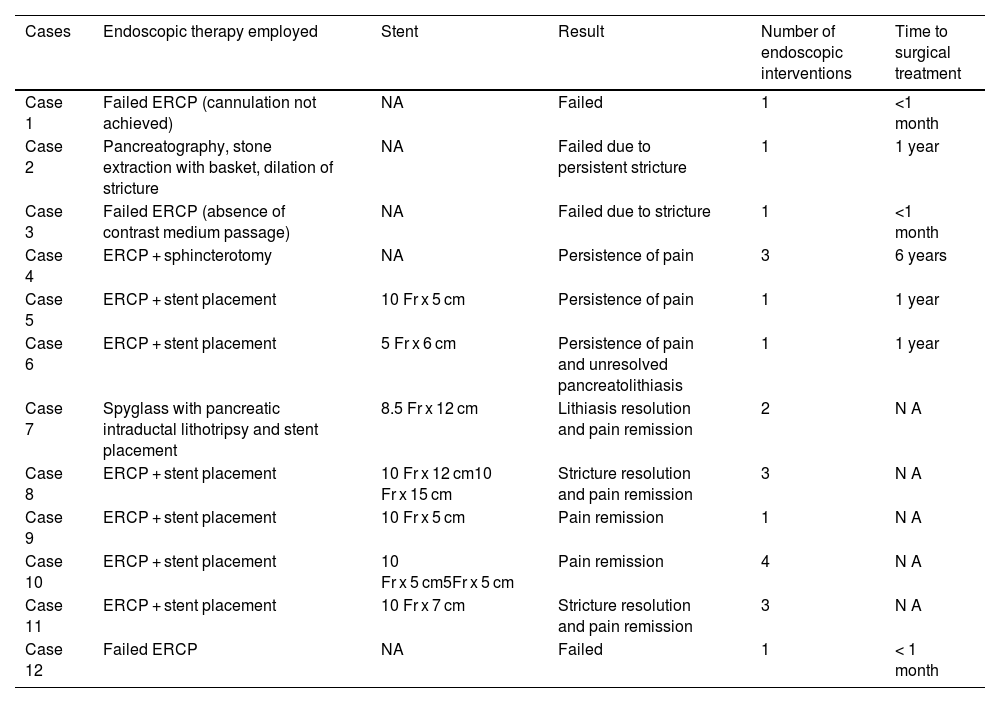
Regarding the type of endoscopic management performed, 7 patients (59%) had ERCP with stent placement, 3 patients (25%) had ERCP reported as failed, one patient (8%) had ERCP with sphincterotomy, and one patient (8%) had the Spyglass® (Boston Scientific, USA) technique with intraductal lithotripsy (Table 2).
Endoscopic treatment characteristics.
| Cases | Endoscopic therapy employed | Stent | Result | Number of endoscopic interventions | Time to surgical treatment |
|---|---|---|---|---|---|
| Case 1 | Failed ERCP (cannulation not achieved) | NA | Failed | 1 | <1 month |
| Case 2 | Pancreatography, stone extraction with basket, dilation of stricture | NA | Failed due to persistent stricture | 1 | 1 year |
| Case 3 | Failed ERCP (absence of contrast medium passage) | NA | Failed due to stricture | 1 | <1 month |
| Case 4 | ERCP + sphincterotomy | NA | Persistence of pain | 3 | 6 years |
| Case 5 | ERCP + stent placement | 10 Fr x 5 cm | Persistence of pain | 1 | 1 year |
| Case 6 | ERCP + stent placement | 5 Fr x 6 cm | Persistence of pain and unresolved pancreatolithiasis | 1 | 1 year |
| Case 7 | Spyglass with pancreatic intraductal lithotripsy and stent placement | 8.5 Fr x 12 cm | Lithiasis resolution and pain remission | 2 | N A |
| Case 8 | ERCP + stent placement | 10 Fr x 12 cm10 Fr x 15 cm | Stricture resolution and pain remission | 3 | N A |
| Case 9 | ERCP + stent placement | 10 Fr x 5 cm | Pain remission | 1 | N A |
| Case 10 | ERCP + stent placement | 10 Fr x 5 cm5Fr x 5 cm | Pain remission | 4 | N A |
| Case 11 | ERCP + stent placement | 10 Fr x 7 cm | Stricture resolution and pain remission | 3 | N A |
| Case 12 | Failed ERCP | NA | Failed | 1 | < 1 month |
ERCP: endoscopic retrograde cholangiopancreatography; NA: not applicable.
With respect to the type of procedure in the surgical management group, 5 patients (50%) underwent the modified Puestow procedure, 2 patients (20%) had distal pancreatectomy with splenectomy, 2 patients (20%) had the Whipple procedure, and one patient (10%) underwent the Frey procedure.
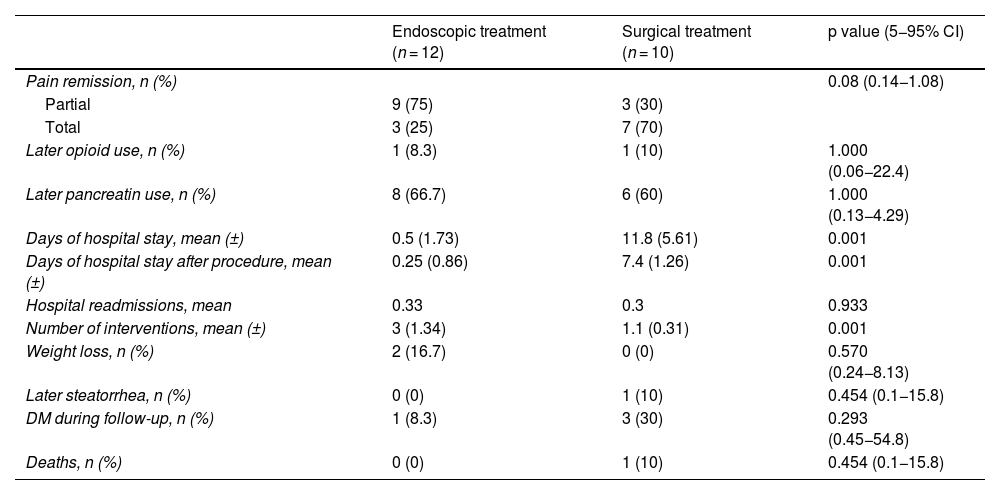
All patients (100%) had pain improvement after the intervention. Partial response was considered when patients reduced their analgesic intake, including the suspension of opioids; total response was the complete suspension of analgesic management after the procedure; and no response was the patient’s own report of said response or if the same pre-procedure analgesic drug therapy was needed after the procedure.
In the endoscopic management group, 9 patients (75%) were considered to have partial response and 3 patients (25%) total response. In the surgical management group, 3 patients (30%) had partial response and 7 patients (70%) had total response. According to those results, the need for opioid use in the patients decreased. Two patients in the endoscopic management group and 3 in the surgical management group suspended their use. A similar response for pancreatin (pancreatic enzymes) use was not found; it continued to be used during follow-up by 8 patients (67%) in the endoscopic management group and 7 patients (70%) in the surgical management group.
Hospital stay duration was noticeably shorter in the endoscopic management group, given that it was an outpatient procedure in practically all cases. The mean total length of stay in the endoscopic management group was 0.5 days (SD ± 1.73) and 11.8 days (SD ± 5.61) in the surgical management group. The mean length of stay after the procedure was 0.25 (SD ± 0.86) and 7.4 (SD ± 1.26), for endoscopic and surgical management, respectively. The mean of hospital readmissions related to chronic pancreatitis was 0.33 for the endoscopic management group and 0.3 for the surgical management group. The mean number of interventions performed was 3 (SD ± 1.34) for the endoscopic management group and 1.1 (SD ± 0.31) for the surgical management group.
Mean follow-up was 36 months; 33.5 months for the endoscopic management group and 39 months for the surgical management group. During follow-up, 7 patients (58.3%) initially treated with endoscopy, required surgery. Indications for surgery were the presence of strictures in the main pancreatic duct with pain persistence in 2 patients, pain persistence in 2 patients, endoscopic pancreatic stone removal failure in one patient, pain persistence and pancreatolithiasis in one patient, and failed ERCP in one patient.
During post-procedure progression, 2 patients in the endoscopic management group had weight loss and one patient in the surgical management group, who underwent distal pancreatectomy, developed steatorrhea. Four patients (one in the endoscopic management group and 3 in the surgical management group) were diagnosed with diabetes mellitus during follow-up. There were no hospital deaths, but one surgical management group patient was readmitted to the hospital on postoperative day 17 and suddenly died (Table 3).
Results after procedure.
| Endoscopic treatment (n = 12) | Surgical treatment (n = 10) | p value (5−95% CI) | |
|---|---|---|---|
| Pain remission, n (%) | 0.08 (0.14−1.08) | ||
| Partial | 9 (75) | 3 (30) | |
| Total | 3 (25) | 7 (70) | |
| Later opioid use, n (%) | 1 (8.3) | 1 (10) | 1.000 (0.06−22.4) |
| Later pancreatin use, n (%) | 8 (66.7) | 6 (60) | 1.000 (0.13−4.29) |
| Days of hospital stay, mean (±) | 0.5 (1.73) | 11.8 (5.61) | 0.001 |
| Days of hospital stay after procedure, mean (±) | 0.25 (0.86) | 7.4 (1.26) | 0.001 |
| Hospital readmissions, mean | 0.33 | 0.3 | 0.933 |
| Number of interventions, mean (±) | 3 (1.34) | 1.1 (0.31) | 0.001 |
| Weight loss, n (%) | 2 (16.7) | 0 (0) | 0.570 (0.24−8.13) |
| Later steatorrhea, n (%) | 0 (0) | 1 (10) | 0.454 (0.1−15.8) |
| DM during follow-up, n (%) | 1 (8.3) | 3 (30) | 0.293 (0.45−54.8) |
| Deaths, n (%) | 0 (0) | 1 (10) | 0.454 (0.1−15.8) |
The main indication for performing an endoscopic or surgical procedure in patients with chronic pancreatitis is the presence of pain, associated with stricture or obstruction due to stones in the main pancreatic duct. The initial approach to either of these options is associated with different factors. Our aim was to report the progression of the patients, according to their initial management.
An advantage of endoscopic management is a shorter hospital stay, such as that of our patients, given that the majority of the endoscopies were outpatient procedures. However, our patients that underwent initial endoscopy required more interventions (more endoscopic procedures, and in some cases, surgical management), similar to that reported in the literature.9,10
The control of abdominal pain was the main indicator that treatment was satisfactory. Our results concur with those of the majority of studies reported in the literature, in which the two techniques have similar results regarding short-term follow-up (the first 2 years after the procedures). Nevertheless, the majority of patients managed endoscopically require numerous interventions to maintain said control. The endoscopic management group in our study required a mean of 3 procedures to control pain, concurring with the results of previous reports.9,11
Regarding partial or total pain remission, our analysis found a statistically significant difference in favor of surgical management. Díte et al. reported no short-term difference but found a difference in favor of surgery at the 5-year follow-up. Likewise, in a systematic review, Mendieta et al. described a statistically significant long-term (more than 2 years) difference and no short-term difference.12,13 We also found no decrease in opioid use in our patients after the procedures.9 There was no statistically significant difference regarding the development of exocrine or endocrine pancreatic insufficiency in our patients, which is similar to that reported in the literature. In a meta-analysis with a total of 570 patients, there was a lower incidence of endocrine insufficiency in the surgical management group, and in a Cochrane review, an association between surgical management and preserved exocrine pancreatic function was found, but with no significant benefit at a more than 5-year follow-up.9,12,14,15 Determining the grade of exocrine pancreatic insufficiency in our population is difficult because we do not have fecal elastase, and so monitoring and treatment decisions are clinical, depending on the presence of steatorrhea. Even though the response in terms of pain remission could be considered satisfactory in our study, the need for medical management with pancreatic enzymes increased during follow-up in both groups, which could be attributed to disease progression, regardless of treatment.
It should be underlined that more than half of our patients in the endoscopic management group underwent surgery during follow-up, a result that has been previously reported in the literature. It is important to try and identify those patients that will eventually require surgery to be able to perform it as soon as possible, given that this disease is characterized by a continuous inflammatory process that causes irreversible damage to the pancreas. Therefore, early surgery can aid in reducing or slowing disease progression.10 In our study, 4 patients were diagnosed with diabetes mellitus during follow-up; one had initially been treated endoscopically, and the others had initially undergone resection (one had distal pancreatectomy, one had subtotal pancreatectomy, and one had pancreatoduodenectomy). Results show that more than half of patients managed through endoscopy eventually require surgery and patients that initially undergo surgery require fewer re-interventions and have better pain control. 10,16
ConclusionsPain is the chief complication in chronic pancreatitis and the main indication for invasive treatment, whether endoscopic or surgical. Slightly more than half of our patients that were managed endoscopically required surgery during the follow-up. Seventy percent of the patients that initially underwent surgery had total pain remission. Deciding which management to offer should be a multidisciplinary decision and individualized for each patient.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.