Granulomatosis with polyangiitis (GPA), formerly known as Wegener’s granulomatosis1,2, is a necrotizing vasculitis that affects the small vessels, with systemic granulomatous inflammation predominantly in the upper respiratory tract, lungs, and kidneys. It is associated with the presence of cytoplasmic anti-neutrophil cytoplasmic antibodies (c-ANCAs) and anti-proteinase 3 (anti-PR3) antibodies1–3. Albeit infrequently, cases of GPA with gastrointestinal (GI) involvement have been reported at 5–11%1,2. The clinical manifestations vary from abdominal pain to massive bleeding and perforation3,4.
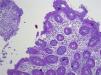
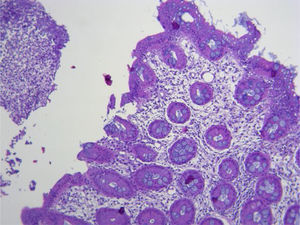
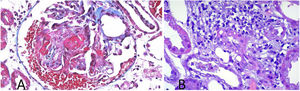
We present herein the case of a 57-year-old woman, with an unremarkable past medical history, that presented with constitutional symptoms and symmetrical polyarthralgia for two months, as well as bloody stools on three occasions, resulting in her seeking medical attention at the emergency department. Upon hospital admission, her vital signs were within normal parameters. Physical examination revealed abdominal pain in the hypogastrium, increased peristalsis, no signs of peritoneal irritation, joint inflammation in the wrists and ankles, and prolonged capillary refill time; the rest of the examination showed no alterations. Laboratory test results were hemoglobin 9g/dl, leukocytes 13,220 cell/mm3, PMN 81.3%, creatinine 3.40mg/dl, BUN 39.5mg/dl, urea 84.6mg/dl, creatinine clearance 14.6ml/min, sodium 135mmol/l, potassium 4.99mmol/l, C-reactive protein 210mg/dl; urinalysis: proteinuria 1.51g/l, hemoglobinuria +++, >100 erythrocytes, 8–10 leukocytes per field, and negative urine culture. Non-contrasted abdominal computed axial tomography (CAT) scan identified wall thickening and edema of the gastric mucosa, and in the terminal ileum, with scant free fluid. Management was started with omeprazole and antibiotic therapy with linezolid and metronidazole. Upper GI endoscopy and colonoscopy were performed, observing a 5mm ulcer in the antrum (Forrest III) and multiple small ulcerations, with fibrin and a cobblestone pattern, in the terminal ileum and cecum. Biopsy results reported a perivascular inflammatory infiltrate, fibrinous exudate, edema of the lamina propria, and no evidence of malignancy (Fig. 1). Methylprednisolone and mesalazine were started and the rheumatology service was consulted. Laboratory results showed positive C-ANCA 1:1,280 and positive anti-PR3 with 427 IAs. Percutaneous kidney biopsy revealed granulomatosis with polyangiitis (Fig. 2). Cyclophosphamide was added, along with trimethoprim/sulfamethoxazole as Pneumocystis jirovecii prophylaxis. The patient improved and was released on day seven of hospitalization. There were no remarkable findings at the follow-up at six months.
The current worldwide incidence of GPA is 20 cases per million, affecting patients between 50 and 70 years of age, with a predominance in White and Asian populations2,4. Clinical manifestations include constitutional symptoms, rapidly progressive necrotizing glomerulonephritis, and involvement of the respiratory tract, peripheral nerves, eyes, joints, and skin1,2,4. GI involvement is rare and tends to occur after the diagnosis of GPA. When it presents simultaneously, it is associated with greater kidney involvement and mortality1,2,5. The disease is caused by a mesenteric vasculitis or direct damage to the submucosal vessels2–6. It tends to present as abdominal pain, nausea, vomiting, gastrointestinal bleeding, intestinal ischemia, and perforation3,5–8. Those symptoms tend to remit with the management of GPA1,2. Nevertheless, other causes of gastrointestinal involvement must be ruled out before starting treatment1,6,9.
The diagnosis of gastrointestinal involvement in GPA is based on the presence of GI symptoms, associated with the involvement of other organs, and is complemented by the presence of C-ANCA in 90% of cases, anti-PR3 in 75%, or myeloperoxidase in 20%2,4,6–8. Pneumoperitoneum, wall thickening, abscesses, free fluid, and microaneurysms in the mesenteric artery can be seen in imaging studies1,9. Endoscopy and colonoscopy may be normal, even in severe cases, but multiple small, round, clear ulcers, associated with clots or recent bleeding, and with diffuse erythema and edema of the mucosa, are commonly observed1,5,9. Biopsies confirm GI involvement, reporting neutrophil infiltrates in the submucosal small vessels (arterioles, venules, and capillaries), causing necrosis, ulceration of the mucosa, granulomatous inflammation surrounded by irregular fibrinoid necrosis, thrombosis, and fibrosis1,4,5,9.
Conservative management with fasting, fluid therapy, nutrition, systemic antibiotic therapy, and systemic glucocorticoids in combination with immunosuppressants, such as cyclophosphamide or rituximab, enable resolution in weeks, in the majority of patients1,2,4. In cases of intestinal perforation or severe bleeding, surgical management is required1,3,6,8.
Without treatment, the prognosis is fatal outcome at six months4. With treatment, the prognosis is reserved, due to the high relapse rate (30–60%)2,4,7. The main causes of death are surgical complications in 44% of patients7 and chronic kidney failure in 50%2.
To the best of our knowledge, this is the first case of a patient with GPA with GI involvement to be reported in Latin America. It is important to emphasize the relation between GPA and GI bleeding, to make the diagnosis and provide opportune treatment.
Ethical considerationsThe present study complies with the current bioethical research regulations, including the protection of persons and animals, data confidentiality following the protocols of the work center regarding their publication and the preservation of patient anonymity, right to privacy, and informed consent. The authors declare that there is no personal information that can enable patient identification.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Pérez-Macías JP, Rodarte-Shade M, Garza-García CA, Tueme-De la Peña D, Rodríguez-Guerra ML. Granulomatosis con poliangitis (granulomatosis de Wegener) con involucro gastrointestinal: reporte de caso. Rev Gastroenterol Méx. 2022;87:392–394.