The prevalence and incidence of inflammatory bowel disease (IBD) has increased significantly in Latin America. Extraintestinal manifestations (EIMs) have elevated morbidity and are poorly characterized in the region. Our aim was to describe the characteristics of EIMs in patients with IBD at the Hospital Universitario Fundación Santa Fe de Bogotá, utilizing the EIM classification proposed by the European Crohn’s and Colitis Organisation (ECCO).
Materials and methodsA cross-sectional study was conducted based on an institutional database of patients with IBD and the EIM definition used by the ECCO. Prevalence and prevalence ratios (PRs) of the EIMs were calculated.
ResultsThe study included 168 patients, 66 of whom were diagnosed with Crohn’s disease (CD) and 102 with ulcerative colitis (UC). A total of 30.4% patients had at least one EIM, and the most frequent were oral ulcers (13.7%), arthritis (10.1%), and uveitis/episcleritis (6.5%). There was a greater prevalence of EIMs in CD (31.8% vs 29.40% in UC) and women (32.47% vs 28.57% in men). There was a significant PR between uveitis/episcleritis and arthritis, erythema nodosum and arthritis, and erythema nodosum and other eye diseases.
ConclusionsOur study shows a high prevalence of EIMs, surpassing that of previous Colombian studies, with a predominance of CD. Oral manifestations stand out as the most common. Prevalence studies on EIMs in Colombia are needed to establish multidisciplinary specialized centers, improving the quality of life of patients with IBD.
La prevalencia e incidencia de la Enfermedad Inflamatoria Intestinal (EII) ha aumentado significativamente en América Latina. Las Manifestaciones Extraintestinales (MEI), tienen morbilidad elevada y están poco caracterizadas en la región. El objetivo de este estudio es describir las características de las manifestaciones extraintestinales en pacientes con EII del Hospital Universitario Fundación Santa Fe de Bogotá, utilizando la clasificación de MEI propuesta por la Organización Europea de Enfermedad de Crohn y Colitis (ECCO).
Materiales y métodosSe realizó un estudio transversal a partir de una base de datos institucional de pacientes con EII y la definición de MEI por la Organización Europea de Enfermedad de Crohn y Colitis (ECCO). Se calcularon la prevalencia y las razones de prevalencia (RP) entre las MEI.
ResultadosSe incluyeron 168 pacientes, 66 diagnosticados con Enfermedad de Crohn (EC) y 102 con Colitis Ulcerosa (CU). El 30.4% presentaba al menos una MEI. Las más comunes fueron úlceras orales (13.7%), artritis (10.1%) y uveítis / epiescleritis (6.5%). Se observó una mayor prevalencia de MEI en EC (31.8% vs. 29.40% en CU) y en mujeres (32.47% vs. 28.57% en hombres). Se encontró una RP significativa entre uveítis/epiescleritis y artritis, eritema nodoso y artritis, y eritema nodoso y enfermedades oculares.
ConclusionesEste estudio muestra una alta prevalencia de MEI, superando investigaciones previas en Colombia, con una predominancia en EC. Las manifestaciones orales destacan como las más comunes. Se necesitan estudios de prevalencia sobre MEI en Colombia para establecer centros especializados multidisciplinarios que mejoren la calidad de vida de los pacientes con EII.
Inflammatory bowel disease (IBD) is a chronic inflammatory disorder that mainly affects the gastrointestinal tract but is not exclusively limited to that system.1,2In fact, extraintestinal manifestations (EIMs), which are often observed in IBD, can involve multiple organ systems, such as the joints, eyes, hepatobiliary tract, and skin.3,4 These systemic manifestations contribute even more to the complexity and heterogenicity of IBD, highlighting the need for a comprehensive understanding of the clinical spectrum of the disease and its associated comorbidities. The aim of the present study was to describe EIM characteristics in a patient cohort seen at the Hospital Universitario Fundación Santa Fe de Bogotá, based on the definition proposed by the European Crohn’s and Colitis Organisation (ECCO).
The ECCO has defined EIMs as “an inflammatory pathology in a patient with IBD that is located outside the gut and for which the pathogenesis is either dependent on extension/translocation of immune responses from the intestine, or is an independent inflammatory event perpetuated by IBD or that shares a common environmental or genetic predisposition with IBD”,3,4 causing increased morbidity, sometimes surpassing that of the intestinal disease itself, and significantly impacting the quality of life of those patients. That organization has developed and proposed an EIM classification that differentiates “true” EIMs from the extraintestinal conditions and complications of IBD that are consequences of the disease itself. They include osteoporosis, nephrolithiasis, cholelithiasis, thromboembolic events, and side effects related to IBD medications, and not classified as true EIMs.4
In addition, these EIMs can respond adequately to treatment for IBD, specifically to certain anti-tumor necrosis factor (anti-TNF) therapies.5 Studies have also shown that the presence of a single EIM increases the probability of developing others, and is often present before the IBD is diagnosed.4,6 Therefore, the presence of an EIM should motivate the search for underlying IBD, thus reducing diagnostic uncertainty and saving time.5
Various studies have currently sought to characterize and determine the prevalence of EIMs in patients with IBD, reporting prevalence rates ranging from 6% to 47%. However, they are not consistent in the predominance of a specific diagnosis.4,7–12 The majority of those studies have been carried out on populations in Europe,7,8 the Middle East,9 and Asia.12 A Colombian study conducted in Medellin found a 23.3% prevalence of EIMs in patients with IBD, with a greater prevalence in patients with Crohn’s disease (CD) (26.5%), compared with those with ulcerative colitis (UC) (22.6%).11 In a study conducted in Bogotá, prevalence was 24.8% in patients with UC and 35% in patients with CD.10
Despite those data, information on the epidemiology of EIMs in patients with IBD is still limited in Latin America. This is most likely due to the perception of IBD as a rare condition in this region, which has recently changed. Nevertheless, it is important to underline that the Colombian studies have shown small discrepancies in their results, such as the occurrence of EIMs in patients with CD, compared with UC, as well as variations in the prevalence of different types of EIMs.10,11Thus, it is imperative to conduct additional studies that can improve our understanding of the behavior and clinical importance of EIMs in the Colombian context. We present herein a cross-sectional study conducted on patients with active IBD seen at the Fundación Santa Fe de Bogotá, a national referral center. Our aim was to determine the prevalence of EIMs and other associated conditions in those patients and explore the interactions between the EIMs and the intrinsic patient characteristics, to aid in providing them with better comprehensive care.
Materials and methodsSubjects and data collectionAn observational, cross-sectional study utilizing the STROBE checklist for observational studies was carried out to determine the prevalence of EIMs and other comorbidities described by the ECCO in 2019.
The patients were selected from the IBD database of the Gastroenterology Research Group of the Hospital Universitario Fundación Santa Fe in Bogotá, Colombia. Included in the database were patients that had been admitted to the hospital, evaluated at the emergency department and/or had disease follow-up at the hospital, within the time frame of January 2018 to December 2022. Diagnosis of CD or UC was confirmed, utilizing the code of the 10th revision of the International Statistical Classification of Diseases (ICD-10) in their medical records: K500, K508, K501, K509, K519, and K518. The diagnosis was verified according to clinical, endoscopic, radiologic, laboratory, and histopathologic criteria specified in the consensus of the Pan American Crohn’s and Colitis Organization (PANCCO).13 The patients that did not meet those diagnostic criteria were excluded from the analysis.
VariablesThe primary result was the presence of EIMs linked to IBD, presented by the patient or diagnosed by a professional, that coincided with “true” EIMs, according to the categorization suggested by the ECCO.3,14 The “true” EIMs identified included spondyloarthritis (peripheral and axial); eye diseases, such as uveitis and episcleritis; oral aphthous ulcers; skin diseases, such as erythema nodosum and pyoderma gangrenosum, and primary sclerosing cholangitis (PSC). Also considered in the study were secondary results, which entailed exploring other categories of the ECCO definition. “IBD complications” and their treatment mainly included metabolic bone disease, nephrolithiasis, and venous thromboembolism. In addition, the study included the analysis of “associated conditions with an uncertain mechanism”, such as noninflammatory arthralgia, autoimmune hepatitis, and eczema. Other variables collected for the analysis were age, age at diagnosis, time since diagnosis, treatment (anti-TNF, vedolizumab, ustekinumab, tofacitinib, azathioprine, 5-ASA, and surgery), and sex.
Statistical analysisThe statistical analysis was performed using R version 4.1.3 and the R Studio version 2022.12.0 + 353 software. Relative frequency for the categorical variables and means with standard deviation for the continuous variables were calculated. Prevalence ratios (PRs) were used to express the associations between the primary results and the categorical variables, and the simple logistic regression analysis was employed to evaluate the association between the primary results and the continuous variables.
Ethical considerationsThe study was approved by the institutional ethics committee of the Hospital Universitario Fundación Santa Fe de Bogotá before its commencement (communication number CCEI-14356-2022). Informed consent was obtained from all participants before the data collection. The data supporting this article are available from the corresponding author upon reasonable request.
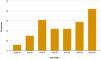
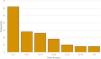
ResultsA total of 178 patients were retrospectively reviewed. Ten patients did not meet the diagnostic criteria for CD or UC. Of the remaining 168 patients, 91 were men (54.17%) and 77 (45.83%) were women. UC was the most frequent diagnosis, with 102 patients (60.72%), whereas 39.28% (66) of the patients were diagnosed with CD. Mean patient age was 52.57 years (SD 19.24), and the age group with the highest number of patients was the group above 70 years of age (Fig. 1). The mean time since diagnosis was 8 years, with a higher number of individuals having a time lapse of 5 years since their diagnosis (Table 1, Fig. 2). In general, 51 patients had a history of EIMs (30.4%).
Summary of study patient characteristics.
| Characteristics | Value (SD) / (%) |
|---|---|
| Age | 52.57 (19.24) |
| Age at IBD diagnosis | 41.45 (17.72) |
| Time since diagnosis | 8 (9.77) |
| Sex | |
| Male (%) | 91 (54.17) |
| Female (%) | 77 (45.83) |
| Diagnosis | |
| Ulcerative colitis (%) | 102 (60.72) |
| Crohn’s disease (%) | 66 (39.28) |
IBD: inflammatory bowel disease; SD: standard deviation.
Of the patients with EIMs, 38 had only one EIM (74.51%), 10 had two EIMs (19.61%), two had three EIMs (3.92%), and one patient had a history of four EIMs (1.96%). In addition, 49% of those patients were women and 51% were men. The most common EIMs were oral aphthous ulcers (n = 23; 13.7%), followed by arthritis (n = 17; 10.1%) and episcleritis/uveitis (n = 11; 6.5%). Arthritis, uveitis/episcleritis, and erythema nodosum were more common in the patients with CD, whereas PSC, pyoderma gangrenosum, and oral aphthous ulcers were more common in UC. Eighteen patients presented with disease complications (10.7%), and the most common was venous thromboembolism (n = 6, 3.6%), which was more frequently present in patients with UC (4.9% vs 1.5%). Lastly, associated conditions with an uncertain mechanism were found in 37 patients (22%) and the most common was noninflammatory arthralgia (n = 27; 16.1%), which was more common in patients with CD (21.2% vs 13%). Table 2 presents a detailed description of those findings.
Diagnosis and frequency of extraintestinal manifestations, disease complications, and disease-associated conditions with an uncertain mechanism.
| Ulcerative colitis | Crohn’s disease | Total | |||||
|---|---|---|---|---|---|---|---|
| Number of patients (n) | 102 | 66 | 168 | ||||
| n | % | n | % | n | % | ||
| EIMs present | 30 | 29.4 | 21 | 31.8 | 51 | 30.4 | |
| Number of EIMs | |||||||
| One | 24 | 23.5 | 14 | 21.2 | 38 | 22.6 | |
| Two | 4 | 3.9 | 6 | 9.1 | 10 | 6 | |
| Three | 1 | 1 | 1 | 1.5 | 2 | 1.2 | |
| Four | 1 | 1 | 0 | 0 | 1 | 0.6 | |
| Oral aphthous ulcers | 15 | 14.7 | 8 | 12.1 | 23 | 13.7 | |
| Arthritis | 7 | 6.9 | 10 | 15.2 | 17 | 10.1 | |
| Uveitis/episcleritis | 5 | 4.9 | 6 | 9.1 | 11 | 6.5 | |
| Erythema nodosum | 6 | 5.9 | 4 | 6.1 | 10 | 6 | |
| Primary sclerosing cholangitis | 4 | 3.9 | 1 | 1.5 | 5 | 3 | |
| Pyoderma gangrenosum | 1 | 1 | 0 | 0 | 1 | 0.6 | |
| Disease complications | 11 | 11 | 7 | 10.6 | 18 | 10.7 | |
| DVT/PTE | 5 | 4.9 | 1 | 1.5 | 6 | 3.6 | |
| Bone metabolism | 2 | 2 | 2 | 3 | 4 | 2.4 | |
| Nephrolithiasis | 1 | 1 | 1 | 1.5 | 2 | 1.2 | |
| Others | 3 | 2.9 | 3 | 4.5 | 6 | 3.6 | |
| Associated conditions with an uncertain mechanism | 21 | 20.6 | 16 | 24.2 | 37 | 22 | |
| Arthralgias | 13 | 12.7 | 14 | 21.2 | 27 | 16.1 | |
| Dermatitis | 4 | 3.9 | 5 | 7.6 | 9 | 5.4 | |
| Autoimmune hepatitis | 4 | 3.9 | 0 | 0 | 4 | 2.4 | |
| Others | 1 | 1 | 1 | 1.5 | 2 | 1.2 | |
DVT: deep vein thrombosis; EIMs: extraintestinal manifestations; PTE: pulmonary thromboembolism.
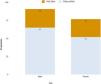
Upon stratification by diagnosis, 30 of the 102 patients with UC had documented EIMs (29.4%), compared with 21 of the 66 patients with CD (31.8%; PR = 1.08; CI: 0.68, 1.72; p = 0.757) (Fig. 3). There was a greater documented prevalence of EIMs in women (28.57% vs 32.47%; PR = 1.14; CI: 0.72, 1.80; p = 0.587) (Fig. 4). No statistical association was found between the presence of EIMs and age or time since diagnosis (years) (OR = 0.99; CI: 0.97, 1.004; p = 0.151 and OR = 1.02; CI: 0.99, 1.06; p = 0.173, respectively).
In contrast, significant associations were seen between the presence of EIMs and therapy with ustekinumab (PR = 3.58; IC: 2.79, 4.58; p < 0.001), as well as a marginal positive association with a history of surgery that was not statistically significant (PR = 1.59; CI: 0.99, 2.55; p = 0.054) (Table 3). We also found that some EIMs were more prone to present together. The PR was significant in eye disease and arthritis (p ≤ 0.001), erythema nodosum and arthritis (p < 0.001), and erythema nodosum and eye disease (p = 0.003). Table 4 summarizes those associations.
Odds ratios and prevalence ratios that show association between characteristics of the disease presenting with extraintestinal manifestations and therapies.
| EIMs | |||
|---|---|---|---|
| n | PR (CI) | p | |
| Age (OR) | – | 0.99 (0.97; 1.004) | 0.151 |
| Age at diagnosis (OR) | – | 0.98 (0.96; 1.0004) | 0.06 |
| Time since diagnosis (OR) | – | 1.02 (0.99; 1.006) | 0.173 |
| Female sex | 25 | 1.14 (0.72; 1.80) | 0.587 |
| Male sex | 26 | 0.88 (0.56; 1.39) | 0.594 |
| Crohn’s disease | 21 | 1.08 (0.68; 1.72) | 0.757 |
| Ulcerative colitis | 30 | 0.92 (0.58; 1.47) | 0.738 |
| Anti-TNF | 13 | 0.84 (0.49; 1.45) | 0.539 |
| Vedolizumab | 6 | 1.11 (0.54; 2.26) | 0.788 |
| Ustekinumab | 2 | 3.58 (2.79; 4.58) | <0.001** |
| Tofacitinib | 1 | 1.16 (0.23; 5.85) | 0.867 |
| Azathioprine | 20 | 1.24 (0.76; 2.01) | 0.393 |
| 5-ASA | 26 | 0.98 (0.60; 1.59) | 0.941 |
| Surgery | 21 | 1.59 (0.99; 2.55) | 0.054 |
CI: confidence interval; EIMs: extraintestinal manifestations; OR: odds ratio; PR: prevalence ratios.
Prevalence ratios that show the associations between the extraintestinal manifestations in inflammatory bowel disease.
| Oral aphthous ulcers | Arthritis | Uveitis/episcleritis | Erythema nodosum | Primary sclerosing cholangitis | Pyoderma gangrenosum | |
|---|---|---|---|---|---|---|
| Oral aphthous ulcers | PR = 0.84 | PR = 0.63 | PR = 2.70 | PR = 1.58 | - (-) | |
| CI: 0.21, 3.44 | CI: 0.08, 4.70 | CI: 0.75, 9.71 | CI: 0.18, 13.49 | |||
| p = 0.818 | p = 0.67 | p = 0.129 | p = 0.691 | |||
| Arthritis | PR = 0.85 | PR = 7.40 | PR = 5.92 | - (-) | - (-) | |
| CI: 0.22, 3.30 | CI: 2.52, 21.70 | CI: 1.85, 18.92 | ||||
| p = 0.825 | p <0.001** | p = 0.003* | ||||
| Uveitis/episcleritis | PR = 0.65 | PR = 5.95 | PR = 6.12 | PR = 3.57 | - (-) | |
| CI: 0.10, 4.37 | IC: 2.55, 13.85 | CI: 1.83, 20.44 | CI: 0.44, 29.26 | |||
| p = 0.668 | p <0.001** | p = 0.003* | p = 0.237 | |||
| Erythema nodosum | PR = 2.37 | PR = 4.86 | PR = 5.92 | - (-) | - (-) | |
| CI: 0.84, 6.65 | CI: 1.94, 12.21 | CI: 1.85, 18.95 | ||||
| p = 0.102 | p <0.001** | p = 0.003* | ||||
| Primary sclerosing cholangitis | PR = 1.48 | - (-) | PR = 3.26 | - (-) | - (-) | |
| CI: 0.25, 8.93 | CI: 0.51, 20.80 | |||||
| p = 0.68 | p = 0.213 | |||||
| Pyoderma gangrenosum | - (-) | - (-) | - (-) | - (-) | - (-) |
CI: confidence interval; PR: prevalence ratio.
The aim of the present study was to establish the frequency of EIMs and related conditions in patients with CD and UC, according to the definition proposed by the ECCO. The results of this analysis indicate a 30.4% prevalence of EIMs, with a slightly higher occurrence in patients with CD (29.4%), even though there were more patients diagnosed with UC. There was also a slightly higher prevalence of EIMs in women (31.65%), compared with men (27.96%). Among the patients with EIMs, 25.59% had a history of multiple EIMs, whereas 75.51% had only one EIM. These results are consistent with those reported in the 2015 Swiss Inflammatory Bowel Disease Cohort Study (SIBDCS), in which 29.3% of all patients with IBD had one EIM and 25% had multiple EIMs (up to 5).5
In addition, the SIBDCS showed that approximately one-third of the patients with CD had a history of at least one EIM, whereas that was the case in only 21.7% of the patients with UC.6 In our study, the prevalence of EIMs was also slightly higher than that reported in a previous Colombian descriptive study. That study included 759 patients, and the prevalence of EIMs was 23.3%, with a higher prevalence in patients with CD (26.5%) than in patients with UC (22.6%), and 18.1% of the patients had multiple EIMs.11 Nevertheless, our percentage results were lower than those in studies conducted on a Middle Eastern cohort (52.3%),9 a cohort at the Mayo Clinic (40%),15 and a Greek cohort (33.1%).8
Unlike prior studies, ours revealed that aphthous ulcers were the predominant EIM. This finding can be attributed to the relative simplicity with which patients can report symptoms of this type or the possibility of underdiagnosing other EIMs by depending on a specialized evaluation for their accurate identification. The majority of studies have reported manifestations in the joints as the most prevalent EIMs in patients with IBD. Specifically, Colombian,6 Swiss,5,16 Greek,7 and Middle Eastern8 studies reported manifestations in joints in 13.5%, 20.5%, 23.3%, and 33.3% of the patients with IBD, respectively. Contrastingly, we observed a 10.1% prevalence in patients with arthritis, with a slight predominance in patients with CD.
The Colombian study was the only one to have used the classification proposed by the ECCO, which could have resulted in the inclusion of other arthropathies classified as associated conditions with an uncertain mechanism in the calculations. In addition, the prevalence of joint pain reported in the Greek study was 16.7%.7 We evaluated associated conditions with an uncertain mechanism at different sites and found that arthralgia was the most prevalent condition, with an incidence of 16.1%, which, when combined with inflammatory arthritis, was similar to the prevalence reported in other studies. Arthropathies are seen more frequently in female patients receiving anti-TNF therapy and in patients with a history of IBD surgery, as well as in patients that present with other EIMs.6,9 Our study also found an association with other EIMs, especially erythema nodosum and eye disease, concurring with results seen in the analyses of the Swiss, Middle Eastern, and Greek cohorts.5,7,8,10
Coexisting EIMs are more frequently reported in patients with CD than in patients with UC.5,7,8,10 In our study, one-third of the patients with CD had multiple EIMs, whereas they were present in only one-fifth of the patients with UC. As observed by Karmiris et al.,8 the majority of patients that develop more than one EIM do so within a short period of time and they are more often diagnosed during disease flare-ups, which could be related to the pathogenic mechanisms of EIMs.5,7
Currently, there are two predominant hypotheses explaining the pathophysiologic mechanisms behind the appearance of EIMs in patients with IBD. These assumptions suggest that EIMs are the result of an increase in the tropism of T cells into extraintestinal tissues, which can be attributed to cytokine overexpression that is generally limited to the intestine. Elevated levels of circulating T cells, in response to intestinal inflammation and injury during active disease phases, are also suggested to contribute to the development of EIMs. Said hypotheses are supported by previous studies and explain the underlying biologic processes that give rise to EIMs in patients with IBD.3,11
There was a 6.5% prevalence of skin and eye manifestations in the present study, which is consistent with previous studies that report a prevalence range of approximately 5-15% for EIMS and 2-7% for ocular EIMs.4,6,9,17 Of the ocular EIMs, scleritis, episcleritis, and uveitis were the most frequent; symptoms of red eye were commonly reported and frequently associated with intestinal inflammation, especially in cases of scleral inflammation. The lack of a timely diagnosis of scleritis can result in permanent damage to vision, and treatment protocols for scleritis differ from those of uveitis, underlining the importance of a rapid and accurate diagnosis.4 However, the diagnosis of those EIMs largely depends on a specialized evaluation, and, as is the case with rheumatologic EIMs, they can be underdiagnosed, leading to significant morbidity due to limited access to medical attention in the Colombian context.
PSC is one of the EIMs that requires a thorough evaluation and diagnosis because of its treatment limitations and association with the development of end-stage liver disease and colorectal cancer.4 The present study indicated there was a greater occurrence of PSC in patients with UC than in patients with CD (3.9% vs 1.5%), which is consistent with results from previous studies, including those conducted in Colombia, Switzerland, and Hungary (4.2% vs 1.5%, 4% vs 1%, and 1.6% vs 0.8%, respectively).6,11,17
The secondary aim of our study was to examine diseases and complications described at other sites in the ECCO classification.3 Associated conditions with an uncertain mechanism were more frequent than complications, and thromboembolic diseases, albeit still rare, were the most frequently observed complication. Said diseases are classified as complications associated with an increased inflammatory burden but caused by inadequate treatment and underutilized thrombosis prophylaxis.3,7,18 Patients with UC had more probability of experiencing thromboembolic diseases, which is consistent with previous studies.8,9
The findings of our study must be interpreted with caution, given that the data were retrospectively collected from a referral center and could be subject to biases and incorrect classifications due to the possibility of incorrect interpretation of definitions and classifications by the researchers. The study design also restricted the interpretation and generalization of the results, given that temporality is a critical characteristic of the clinical importance of EIMs. The data were collected from a referral center, and so the extrapolation of the findings to the general population was limited by the size of the study sample. Despite these limitations, the study reflects trust in the accurate classification of the majority of EIMs because the specialists in IBD have experience in patient follow-up and collected information from the clinical records. The database of the IBD center was carefully constructed by the group, utilizing ambulatory and hospitalized patient data from the hospital’s electronic clinical records. Lastly, comparisons between the current findings and those from previous studies should also be addressed with care, given that certain definitions are not included in all the prior studies and some classifications remain open to the interpretation of the researchers.
ConclusionOur study results showed a high prevalence of EIMs in a Colombian population sample with IBD, with a greater prevalence in CD, compared with UC. The study identified additional conditions that are not included as “true” EIMs in the classification proposed by the ECCO (“disease complications” and “associated conditions with an uncertain mechanism”) but that are associated with the morbidity of the disease, as reported in previous studies. Our study also identified potential interactions and risks that could be clinically significant and serve as the basis for future clinical research. Prevalence studies on EIMs in Colombia are necessary for the development of specialized multidisciplinary centers that can improve the quality of life of patients with IBD. Finally, this demonstrates the need for a clear classification of EIMs, to guarantee the reproducibility of the study and the overall analysis of the individual results.
What do we presently know? Extraintestinal manifestations (EIMs) are a common problem in patients with inflammatory bowel disease (IBD). Even though EIM pathophysiology has been clarified to a certain degree, their real-world behavior is still not fully understood. In particular, the epidemiology of these manifestations that significantly affect IBD patient management and quality of life shows a variety of behaviors and largely depends on the definition and understanding of EIMs. The European Crohn’s and Colitis Organisation (ECCO) has developed a classification that categorizes what were traditionally considered EIMs into groups. This classification serves as a basis for universal comprehension and the creation of recommendations for patient care. The ECCO classification includes “true EIMs”, “associated conditions with an uncertain mechanism”, and “complications of IBD and/or its treatment”.
What is new herein? This study presents new data based on the 2019 classification proposed by the ECCO and was conducted at an IBD referral center in Colombia. The prevalence reported in this strict analysis differs from that reported in large European, Asian, and Middle Eastern cohorts. These findings suggest that the prevalence of EIMs largely depends on diagnostic resources, the contribution of different experts, and the interpretation of the ECCO classification.
How can this article aid patient care? This study is an important first step in understanding how EIMs present in the Colombian context. The analysis of the prevalence of EIMs and the factors that influence them can contribute to more informed decision-making at centers and by multidisciplinary healthcare groups, with respect to patients. The knowledge obtained from this research can lead to improved patient care for individuals with IBD and EIMs in Colombia.
JAR: Study design, data collection and interpretation, writing of the manuscript, and editing of the important intellectual content.
DRC, JGMQ, SGSG: Study design, data collection, writing of the manuscript, and editing of the important intellectual content.
LCA, EJCN: Patient recruitment, data collection.
RGD, ELS, AMRR, BMM, RPLP: Study design, patient recruitment, data collection, writing of the manuscript, and editing of the important intellectual content.
Financial disclosureNo financial support was received in relation to this study.
The authors wish to thank the physicians, Kevin Rico and Silvia Ballesteros, of the Subdirección de Estudios Clínicos e Investigación of the Fundación Santa Fe de Bogotá, and all members of the IBD Multidisciplinary Group for their collaboration.