Endoscopic retrograde cholangiopancreatography (ERCP) should be an exclusively therapeutic procedure, for both pancreatic and biliary pathologies. The knowledge and understanding of its complications have advanced considerably over the past decade. A standardized consensus of definitions of the complications has been developed, and several multicenter and multivariate studies have provided a clearer comprehension of the risks associated with the patient and the risks associated with the technique per se.1
Complications can encompass a broad spectrum, including pancreatitis, bleeding, cholecystitis, bowel perforation, and cardiovascular events, in approximately 0.8–10% of cases.2 There are risk factors for developing a complication, such as the number of cannulation attempts, portal hypertension, coagulopathy, anatomic anomalies of the papilla, bile duct obstruction, and biliary tract malignancy.3 It is important to understand that a successful procedure with minor, or even moderate, complications can be preferable to a failed procedure with no complications, given that the latter scenario often implies the need for major surgery or advanced interventional radiology procedures, both carrying their own morbidity and mortality risks, which are often greater than those of ERCP.4
The most common complications are usually the consequence of bile duct cannulation or sphincterotomy. However, the inadequate use of accessories can result in rare, but potentially catastrophic, complications. Such is the case of subcapsular hepatic hematoma, which is described in only a few case reports in the medical literature. Those patients usually present with abdominal pain, hemodynamic instability, and a decrease in hemoglobin. Diagnosis commonly requires imaging studies (tomography or ultrasound) within the first 5 days of the event.5 No case diagnosed in an intraoperative procedure following an ERCP has been reported in the literature.
There are 2 hypotheses as to cause. The first involves the laceration of small vessels of the hepatic parenchyma, as a result of intrahepatic duct or capsular perforation by a hydrophilic guidewire. In the second, traction force exerted on the common bile duct by an extraction balloon is the cause.6 In general, the majority of patients recover through conservative management. Prophylactic antibiotic administration is of vital importance, given that those patients are thought to be at an increased risk for infection due to bacteria gaining access into the biliary tract.7
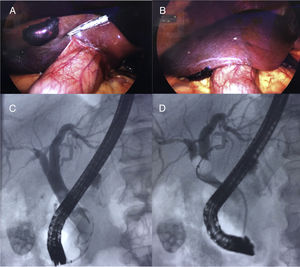
We present herein the case of a 30-year-old man, with no past history related to his current illness, who presented with sudden colicky, abdominal pain located in the right hypochondrium radiating to the back, jaundice, and fever. An abdominal ultrasound study identified gallstones and a 10mm dilation of the extrahepatic bile duct. The patient's total bilirubin level was 6mg/dl, with no coagulation alterations. He was diagnosed with cholangitis and at high risk for choledocholithiasis. Antibiotic therapy was begun and ERCP was performed. The bile duct was selectively cannulated with a hydrophilic guidewire (Hydra Jagwire™, Boston Scientific, USA). Cholangiography showed an approximately 8mm dilation of the intrahepatic bile duct, an 11mm dilation of the extrahepatic bile duct, with multiple repletion defects, and stones in the gallbladder. Wide biliary sphincterotomy of 15mm in diameter was carried out. All stones were then extracted with a balloon extractor (ExtractorTM Pro XL, 15mm/8mm Boston Scientific, USA), for 1min, resolving the choledocholithiasis (Fig. 1).
One day after the ERCP, the patient was asymptomatic. Early laparoscopic cholecystectomy was then performed, identifying a nonexpanding subcapsular hepatic hematoma at the level of segment V, measuring approximately 4cm×3cm, that was reported as a complication of the ERCP study. The procedure was completed with no complications. Treatment of the subcapsular hepatic hematoma was surveillance and follow-up with imaging studies (Fig. 1). The patient was released on postoperative day 3, to continue surveillance in the outpatient setting. At one month, we report a survival rate of 100%, mortality rate 0%, and complication rate 0%.
The number of cases required to maintain optimum surgical skill is not known, but most likely is 50–100 cases per year for routine biliary procedures and 200–250 per year for advanced pancreatic procedures. Finding the optimum balance between the risks and benefits for each patient is key for every endoscopist and the endoscopist's ability and experience must also be taken into account. Nevertheless, complications can still occur.8
Treatment is conservative for stable patients with a non-compressive, peripheral, limited subcapsular hepatic hematoma. Control hemoglobin counts and verification through abdominal computed tomography are advisable. Whenever there is hemodynamic instability with active bleeding and contrast medium extravasation, immediate treatment should be radiologic or surgical. The data in the literature are in favor of conservative treatment (43.5%), percutaneous embolization (26%), drainage (17.4%), and surgery (13%).9
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
The authors wish to thank the entire general surgery and gastrointestinal endoscopy services for the daily support and care of our patient that was performed with unequaled effort and dedication.
Please cite this article as: Fernández-Enríquez ER, Bada-Yllán O, López y López MA, Delano-Alonso R, Herrera-Esquivel JJ. Hematoma hepático subcapsular posterior a la colangiopancreatografía retrógrada endoscópica, un hallazgo intraoperatorio inusual. Revista de Gastroenterología de México. 2021;86:92–94.