Gastrointestinal (GI) tract perforation is a complication found in only 1% of cases of foreign body ingestion.1–4 Medication blister packs are a rare cause of GI tract perforation, mainly affecting the esophagus and ileum.1,2,5 Currently, there is no consensus on diagnosing and treating esophageal perforations. Surgical management is the most accepted method, although less invasive therapies have produced good results in some instances.6
A 73-year-old man had a past medical history of prostate cancer with metastasis to the right acetabulum, treated with radiotherapy and goserelin; diabetes controlled with metformin; and recurrent episodes of anxiety. He came to the emergency service due to dysphagia to solids and intense neck pain that presented 8 days after having taken, in a crisis of anxiety, several tablets of paracetamol/tramadol, on a single occasion. Upon admission, his vital signs were BP 114/78 mmHg, HR 80 bpm, RR 20 bpm, temperature 36.2 °C, and oxygen saturation 94%. The patient had no signs of bleeding, hemodynamic instability, or systemic inflammatory response and presented only with crackling at the level of the muscular triangle. Laboratory work-up reported hemoglobin 13.4 g/dL, leukocytes 7.14 thousand/mm3, absolute neutrophils 5.2 thousand/mm3, platelets 259 thousand/mm3, PT 15 s, aPTT 29.2 s, and INR 1.35.
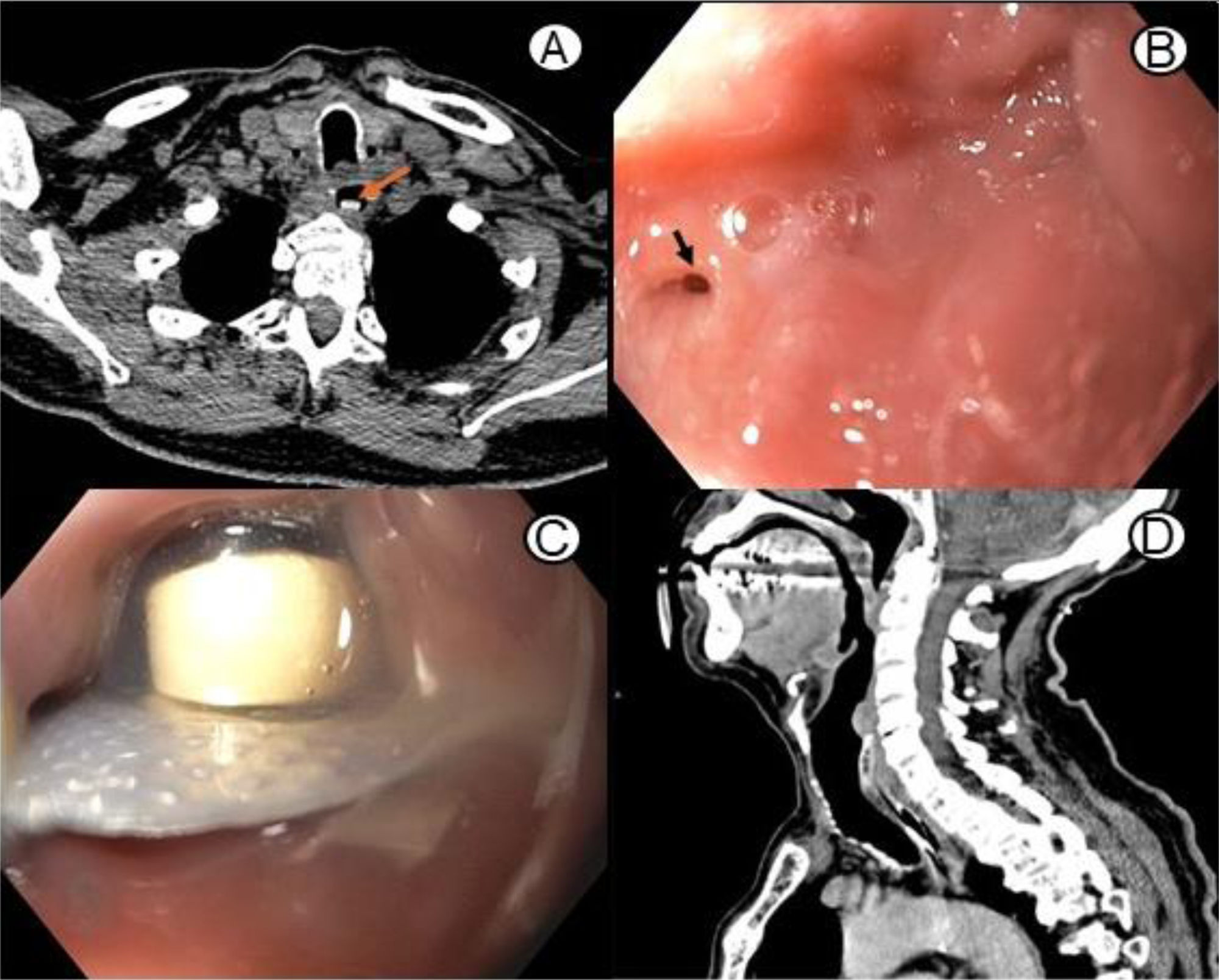
A computed tomography scan was ordered and revealed retropharyngeal air and a foreign body in the cervical esophagus (Fig. 1A). The patient underwent esophagogastroduodenoscopy with an Olympus GIF HQ190 gastroscope. A 3 mm perforation was found in the hypopharynx (Fig. 1B) and a tablet still inside its blister pack was detected 2 cm distal to the cricopharyngeal muscle (Fig. 1C). The blister pack was removed with foreign body forceps. A second perforation, measuring 25 × 5 mm, was observed at the level of the cervical esophagus. A nasogastric tube was placed, and a prophylactic antibiotic regimen with ceftriaxone and metronidazole was started.
Tomographic and endoscopic findings of a foreign body impacted in the cervical region of the esophagus. A) Axial CT view showing a foreign body (arrow) in the esophageal lumen. B) EGD showing a 3 mm perforation (arrow) on the left side of the hypopharynx. C) EGD showing the tablet and its blister pack in the cervical esophagus. D) Control CT at 5 days after the endoscopic examination, showing no signs of esophageal perforation.
The patient’s post-procedural progression was favorable, with improvement in pain and no signs of a systemic inflammatory response. At 48 h from treatment, enteral nutrition was started. Five days later, the patient was discharged from the hospital, with a computed tomography scan showing no signs of a lesion (Fig. 1D). The management video is available in the annex (Video 1 in Supplementary material).
Three weeks later, a control esophagogastroduodenoscopy revealed no signs of a lesion, and so the patient was prescribed a bland diet. At the one-year follow-up, he is asymptomatic, with no sequelae.
Perforation of the esophagus is rare.3 It is a medical emergency, with a 15–30% mortality rate.7 The intrathoracic region of the esophagus is the most affected (55%), followed by the cervical (25%) and abdominal (20%) areas.3,6
There is no consensus on the treatment of esophageal perforation. Variables, such as the size and location of the lesion, progression time, and the presence of contamination, should be considered. To choose the optimum management, the patient’s condition must be considered.6
The Cameron criteria (well-circumscribed intramural or transmural perforation, a sealed lesion, and no signs of sepsis, distal obstruction, or malignant esophageal disease outside of the abdominal esophagus) aid in selecting the patients that can be managed conservatively. The patient that does not meet those criteria should be treated surgically.7 The European Society of Gastrointestinal Endoscopy suggests that conservative treatment include broad-spectrum antibiotic therapy, symptom control with analgesics and antacids, fasting, nasogastric aspiration, and strict surveillance.8 There is a lower risk for contamination of the mediastinum in the cervical esophagus. Thus, conservative treatment in that region offers better results.8 Our patient met all the Cameron criteria, and the perforation was contained in the cervical esophagus, resulting in our opting for conservative treatment.
The period from perforation to its diagnosis is the main prognostic factor for survival in these patients.6,7 In a meta-analysis, Biancari et al.9 reported a 7.4% mortality rate in the patients whose treatment started before the first 24 h from the time of the perforation and rose to 20.3% in the patients whose treatment began after the first 24 h.9 Most of the patients with esophageal perforation due to blister pack ingestion were diagnosed and treated 24 h after said ingestion. All the literature regarding patient follow-up shows that no signs of lesions were found in the control studies, and two of those patients died. In the case of our patient, no lesion was detected in the control endoscopy at 3 weeks and his progress at one year was favorable, with no sequelae.
In contrast to our case, in 2023, Yu et al.10 reported on a patient, who after nine days from having ingested a blister pack, was managed surgically through laparotomy, after evidence of an uncontained lesion in the esophageal wall. Despite said management, the patient needed mechanical ventilation in the postoperative period and presented with bilateral pleural effusion; he developed multiorgan failure and died on postoperative day 15.10 By comparison, our case underlines the importance of having different factors for adequate management selection, such as the time interval from the perforation to its diagnosis and the clinical conditions of the patient. In addition, even if the selection of the therapeutic method is satisfactory, different associated factors can result in considerable differences in therapeutic success.
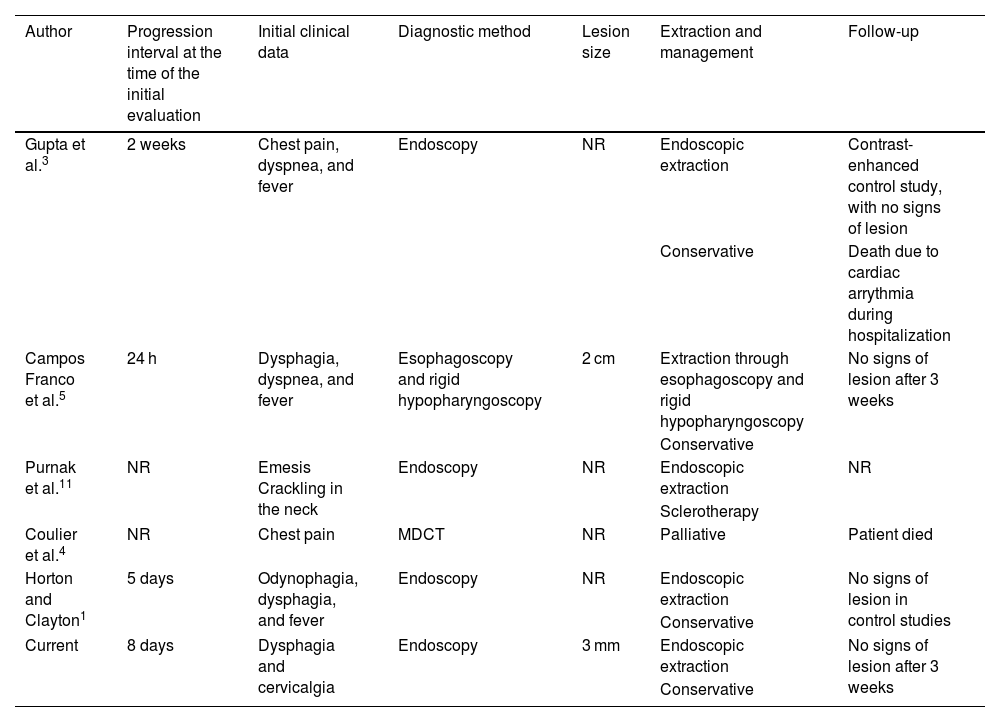
Foreign body ingestion is a common problem in the advanced-age population, and due to polypharmacy, the incidence of blister pack ingestion is expected to increase.4 In 2015, Yao et al.2 described 17 cases of GI tract perforation related to medication blister packs, 14 located in the ileum and 3 in the esophagus. Since then, according to our research, 2 more cases of esophageal perforation due to medication blister pack ingestion have been reported (Table 1).1,3–5,11
Cases of esophageal perforation related to the ingestion of medication blister packs reported in the literature.
| Author | Progression interval at the time of the initial evaluation | Initial clinical data | Diagnostic method | Lesion size | Extraction and management | Follow-up |
|---|---|---|---|---|---|---|
| Gupta et al.3 | 2 weeks | Chest pain, dyspnea, and fever | Endoscopy | NR | Endoscopic extraction | Contrast-enhanced control study, with no signs of lesion |
| Conservative | Death due to cardiac arrythmia during hospitalization | |||||
| Campos Franco et al.5 | 24 h | Dysphagia, dyspnea, and fever | Esophagoscopy and rigid hypopharyngoscopy | 2 cm | Extraction through esophagoscopy and rigid hypopharyngoscopy | No signs of lesion after 3 weeks |
| Conservative | ||||||
| Purnak et al.11 | NR | Emesis Crackling in the neck | Endoscopy | NR | Endoscopic extraction | NR |
| Sclerotherapy | ||||||
| Coulier et al.4 | NR | Chest pain | MDCT | NR | Palliative | Patient died |
| Horton and Clayton1 | 5 days | Odynophagia, dysphagia, and fever | Endoscopy | NR | Endoscopic extraction | No signs of lesion in control studies |
| Conservative | ||||||
| Current | 8 days | Dysphagia and cervicalgia | Endoscopy | 3 mm | Endoscopic extraction | No signs of lesion after 3 weeks |
| Conservative |
MDCT: multidetector computed tomography; NR: not reported.
Blister pack ingestion is a rare but increasing cause of esophageal perforation. Early diagnosis and treatment are vital for preventing fatal outcomes. Conservative management can be an acceptable option with good results and prognosis in a select group of patients.
Author contributionsJPPM: research, supervision, writing of the original draft, and review and editing of the writing; MERS: validation and visualization; AYOC: research, supervision, writing of the original draft; AIHG: validation and visualization; EFMB: review and editing of the writing. All the authors read and approved the final manuscript.
Ethical considerationsThe authors declare that this article contains no information that could identify the patient. Informed consent was obtained from the patient at the time of receiving medical attention, undergoing treatments. This report complies with the current bioethical research regulations, did not require the authorization of the Bioethics Committee because the integrity, health of the patient were not compromised.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.